Description of the drug JARDINS® (DZHARDINS)
Cases of diabetic ketoacidosis, a serious and life-threatening condition requiring urgent hospitalization, have been reported with the use of empagliflozin, including. with fatal outcome. In some of these cases, the manifestations were atypical and were expressed in a moderate increase in blood glucose concentration (not more than 14 mmol/L (250 mg/dL)).
The risk of developing diabetic ketoacidosis should be considered in the event of the appearance of nonspecific symptoms such as nausea, vomiting, lack of appetite, abdominal pain, severe thirst, difficulty breathing, disorientation, unmotivated fatigue or drowsiness. If such symptoms develop, patients should be promptly evaluated for ketoacidosis, regardless of blood glucose concentration. If ketoacidosis is suspected, empagliflozin should be discontinued, the patient assessed and treated promptly.
Patients who may be at higher risk of developing diabetic ketoacidosis include those on a very low carbohydrate diet (in which case this combination may further increase the body's production of ketones), patients with acute illness, and patients with pancreatic disease. glands suggestive of insulin deficiency (eg, type 1 diabetes mellitus, history of pancreatitis, or pancreatic surgery), with reduced insulin dosage (including insulin pump failure), patients with alcohol abuse, patients with severe dehydration, and patients with a history of ketoacidosis .Caution should be exercised when reducing the dose of insulin. In patients receiving empagliflozin, consider monitoring for ketoacidosis and temporarily discontinuing empagliflozin in clinical situations predisposing to the development of ketoacidosis (eg, prolonged fasting due to acute illness or surgery).
It is recommended to monitor renal function before starting treatment and periodically during treatment (at least once a year), as well as before prescribing concomitant therapy that may adversely affect renal function. In patients with renal failure (GFR <45 ml/min/1.73 m2), empagliflozin is contraindicated.
Patients aged 75 years and older have an increased risk of dehydration. These patients were more likely to experience adverse reactions caused by hypovolemia.
Use with caution in cases where a decrease in blood pressure is undesirable, for example, in patients with cardiovascular diseases; patients taking antihypertensive drugs (with a history of arterial hypotension), as well as in patients over 75 years of age.
If a patient receiving empagliflozin develops conditions that may lead to fluid loss (for example, gastrointestinal diseases), the patient's condition, blood pressure, and hematocrit and electrolyte balance should be carefully monitored. Temporary discontinuation of empagliflozin may be required until fluid balance is restored.
If complicated urinary tract infections develop, temporary discontinuation of empagliflozin therapy is necessary.
According to the mechanism of action, glucose is detected in the urine in patients receiving empagliflozin.
Impact on the ability to drive vehicles and machinery
During the treatment period, patients should be careful when driving vehicles and machinery, because When using epagliflozin (especially in combination with sulfonylurea derivatives and/or insulin), hypoglycemia may develop.
Jardiance®
Empagliflozin is a reversible, highly active, selective and competitive inhibitor of sodium glucose transporter type 2 with a concentration required to inhibit 50% of enzyme activity (IC50) of 1.3 nmol. The selectivity of empagliflozin is 5000 times greater than the selectivity of sodium-dependent glucose transporter type 1, responsible for the absorption of glucose in the intestine.
In addition, empagliflozin was found to be highly selective for other glucose transporters responsible for glucose homeostasis in various tissues.
Sodium-dependent glucose transporter type 2 is the primary transport protein responsible for the reabsorption of glucose from the glomeruli back into the bloodstream.
Empagliflozin improves glycemic control in patients with type 2 diabetes mellitus (T2DM) by reducing renal glucose reabsorption. The amount of glucose excreted by the kidneys through this mechanism depends on the concentration of glucose in the blood and the glomerular filtration rate (GFR). Inhibition of sodium-dependent glucose transporter type 2 in patients with type 2 diabetes and hyperglycemia leads to the excretion of excess glucose by the kidneys.
In a 4-week clinical study, it was found that in patients with type 2 diabetes, renal glucose excretion increased immediately after the first dose of empagliflozin; this effect lasted for 24 hours. The increase in renal glucose excretion persisted until the end of treatment, averaging about 78 g/day when using empagliflozin at a dose of 25 mg once daily. In patients with type 2 diabetes, an increase in renal glucose excretion led to an immediate decrease in plasma glucose concentrations.
Empagliflozin (at a dose of 10 mg and 25 mg) reduces the concentration of glucose in the blood plasma both when taken on an empty stomach and after a meal.
The mechanism of action of empagliflozin does not depend on the functional state of pancreatic beta cells and insulin metabolism, which contributes to a low risk of possible development of hypoglycemia. Positive effects of empagliflozin on surrogate markers of beta cell function, including the HOMA-β (Homeostasis Model-B) index and proinsulin-to-insulin ratio, were observed. In addition, additional excretion of glucose by the kidneys causes a loss of calories, which is accompanied by a decrease in the volume of adipose tissue and a decrease in body weight.
Glucosuria observed during the use of empagliflozin. is accompanied by a slight increase in diuresis, which may contribute to a moderate decrease in blood pressure.
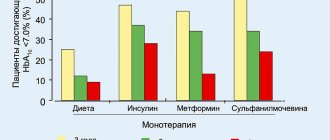
In clinical studies using empagliflozin as monotherapy; combination therapy with metformin; combination therapy with metformin in patients with newly diagnosed type 2 diabetes; combination therapy with metformin and sulfonylurea derivatives; combination therapy with pioglitazone +/- metformin; combination therapy with linagliptin in patients with newly diagnosed type 2 diabetes; combination therapy with linagliptin added to metformin therapy; combination therapy with linagliptin compared with placebo in patients with inadequate glycemic control while taking linagliptin and metformin; combination therapy with metformin compared with glimepiride (data from a 2-year study); combination therapy with insulin (regimen of multiple insulin injections) +/- metformin; combination therapy with basal insulin: combination therapy with a dipeptidyl peptidase-4 (DPP-4) inhibitor, metformin +/- another hypoglycemic oral drug has been shown to have a statistically significant decrease in glycosylated hemoglobin (HbAlc), a decrease in fasting plasma glucose concentrations, and a decrease in blood pressure and body weight.
A clinical trial examined the effect of JARDINS® on the incidence of cardiovascular events in patients with type 2 diabetes and high cardiovascular risk (defined as the presence of at least one of the following diseases and/or conditions: coronary artery disease (history of myocardial infarction, coronary artery bypass grafting). arteries, ischemic heart disease with damage to one coronary vessel, ischemic heart disease with damage to several coronary vessels), a history of ischemic or hemorrhagic stroke, peripheral arterial disease with or without symptoms), receiving standard therapy, which included hypoglycemic drugs and drugs for the treatment of cardiovascular diseases. The primary endpoint was cardiovascular death, non-fatal myocardial infarction, and non-fatal stroke. Additional prespecified endpoints included cardiovascular death, all-cause mortality, development of nephropathy or progressive worsening of nephropathy, and hospitalization for heart failure.
Empagliflozin improved overall survival by reducing cardiovascular death. Empagliflozin reduced the risk of hospitalization for heart failure. JARDINS® was also shown in a clinical trial to reduce the risk of nephropathy or progressive worsening of nephropathy.
In patients with baseline macroalbuminuria, it was found that JARDINS® resulted in sustained normo- or microalbuminuria significantly more often than placebo (hazard ratio 1.82, 95% CI 1.40, 2.37).
Jardines
Oral hypoglycemic drug. Empagliflozin is a reversible, highly active, selective and competitive inhibitor of sodium glucose transporter type 2 with a concentration required to inhibit 50% of enzyme activity (IC50) of 1.3 nmol. The selectivity of empagliflozin is 5000 times greater than the selectivity of sodium-dependent glucose transporter type 1, responsible for the absorption of glucose in the intestine.
In addition, empagliflozin was found to be highly selective for other glucose transporters responsible for glucose homeostasis in various tissues.
Sodium-dependent glucose transporter type 2 is the primary transport protein responsible for the reabsorption of glucose from the glomeruli back into the bloodstream.
Empagliflozin improves glycemic control in patients with type 2 diabetes mellitus by reducing renal glucose reabsorption. The amount of glucose excreted by the kidneys through this mechanism depends on the blood glucose concentration and GFR. Inhibition of sodium-dependent glucose transporter type 2 in patients with type 2 diabetes mellitus and hyperglycemia leads to the excretion of excess glucose by the kidneys.
In clinical studies, it was found that in patients with type 2 diabetes mellitus, renal glucose excretion increased immediately after the first dose of empagliflozin; this effect lasted for 24 hours. The increase in glucose excretion by the kidneys persisted until the end of the 4-week treatment period, amounting to an average of about 78 g/day when using empagliflozin at a dose of 25 mg 1 time/day. In patients with type 2 diabetes mellitus, an increase in renal glucose excretion led to an immediate decrease in plasma glucose concentrations.
Empagliflozin reduces plasma glucose concentrations both when taken on an empty stomach and after meals.
The mechanism of action of empagliflozin does not depend on the functional state of pancreatic β-cells and insulin metabolism. A positive effect of empagliflozin on surrogate markers of β-cell functional activity, including the HOMA-β index (homeostasis model assessment) and the proinsulin-to-insulin ratio, was noted. In addition, additional excretion of glucose by the kidneys causes a loss of calories, which is accompanied by a decrease in the volume of adipose tissue and a decrease in body weight.
Glucosuria observed during the use of empagliflozin is accompanied by a slight increase in diuresis, which may contribute to a moderate decrease in blood pressure.
In clinical studies using empagliflozin as monotherapy; combination therapy with metformin; combination therapy with metformin in patients with newly diagnosed type 2 diabetes mellitus; combination therapy with metformin and sulfonylurea derivatives; combination therapy with pioglitazone +/- metformin; combination therapy with linagliptin in patients with newly diagnosed type 2 diabetes mellitus; combination therapy with linagliptin added to metformin therapy; combination therapy with metformin compared with glimepiride (data from a 2-year study); combination therapy with insulin (regimen of multiple insulin injections) +/- metformin; combination therapy with basal insulin; Combination therapy with a dipeptidyl peptidase-4 (DPP-4) inhibitor, metformin +/- another hypoglycemic oral drug has been shown to produce a statistically significant decrease in glycosylated hemoglobin (HbA1c), a decrease in fasting plasma glucose concentrations, as well as a decrease in blood pressure and body weight.
Pharmacokinetics
The pharmacokinetics of empagliflozin have been extensively studied in healthy volunteers and in patients with type 2 diabetes mellitus.
Suction
After oral administration, empagliflozin is rapidly absorbed, the Cmax of empagliflozin in the blood plasma is reached after 1.5 hours. Then the concentration of empagliflozin in plasma decreases in a biphasic manner. The average AUC value during the period of steady-state plasma concentration was 4740 nmol×h/l, and the Cmax value was 687 nmol/l. Food intake does not have a clinically significant effect on the pharmacokinetics of empagliflozin.
The pharmacokinetics of empagliflozin in healthy volunteers and in patients with type 2 diabetes mellitus were generally similar.
Distribution
Vd during the period of steady-state plasma concentration is approximately 73.8 l. After oral administration of labeled empagliflozin [14C] to healthy volunteers, plasma protein binding was 86%. When using empagliflozin 1 time/day, Css in blood plasma was achieved after the fifth dose.
Metabolism
The main metabolic pathway of empagliflozin in humans is glucuronidation with the participation of uridine-5′-diphospho-glucuronosyltransferases UGT2B7, UGT1A3, UGT1A8 and UGT1A9. The most commonly identified metabolites of empagliflozin are three glucuronic conjugates (2-O, 3-O and 6-O glucuronide). The systemic effect of each metabolite is small (less than 10% of the total effect of empagliflozin).
Removal
T1/2 is approximately 12.4 hours. After oral administration of labeled empagliflozin [14C], approximately 96% of the dose was excreted in healthy volunteers (41% through the intestines, 54% through the kidneys). Through the intestines, most of the labeled drug was excreted unchanged. Only half of the labeled drug was excreted unchanged by the kidneys.
Pharmacokinetics in special groups of patients
In patients with mild, moderate, or severe renal impairment (30< GFR <90 mL/min/1.73 m2) and in patients with end-stage renal disease, empagliflozin AUC values increased by approximately 18%, 20%, 66%, and 48% respectively, compared with patients with normal renal function. In patients with moderate renal impairment and in patients with end-stage renal disease, the plasma Cmax of empagliflozin was similar to that in patients with normal renal function. In patients with mild to severe renal impairment, empagliflozin plasma Cmax was approximately 20% higher than in patients with normal renal function. Data from a population pharmacokinetic analysis showed that the total clearance of empagliflozin decreased as GFR decreased, resulting in increased drug exposure.
In patients with mild, moderate, and severe hepatic impairment (Child-Pugh classification), empagliflozin AUC values increased by approximately 23%, 47%, and 75%, respectively, and Cmax values increased by approximately 4%, 23%, and 48%, respectively ( compared to patients with normal liver function).
BMI, gender, race, and age did not have a clinically significant effect on the pharmacokinetics of empagliflozin.
The pharmacokinetics of empagliflozin have not been studied in children.
Jardines, 30 pcs., 10 mg, film-coated tablets
Jardins® is not recommended for use in patients with type 1 diabetes mellitus or for the treatment of diabetic ketoacidosis.
Diabetic ketoacidosis.
Rare cases of diabetic ketoacidosis have been reported with the use of sodium-glucose transporter type 2 inhibitors, including empagliflozin. In some of these cases, the manifestations were atypical and were expressed in a moderate increase in blood glucose concentration (not more than 14 mmol/L (250 mg/dL).
The risk of developing diabetic ketoacidosis should be taken into account in the event of the appearance of nonspecific symptoms such as nausea, vomiting, lack of appetite, abdominal pain, severe thirst, difficulty breathing, disorientation, unmotivated fatigue or drowsiness.
If such symptoms develop, patients should be promptly evaluated for ketoacidosis, regardless of blood glucose concentration. Use of Jardins® should be discontinued or temporarily suspended until a diagnosis has been established.
Patients who may be at higher risk of developing diabetic ketoacidosis include those on a very low-carbohydrate diet (in which case this drug combination may further increase ketone production in the body), patients with severe dehydration, and patients with ketoacidosis. history or patients with low secretory activity of pancreatic beta cells. In such patients, Jardins® should be used with caution. Caution should be exercised when reducing the insulin dose.
Jardins® contains 162.5 mg of lactose at a dosage of 10 mg, and 113 mg of lactose at a dosage of 25 mg, so the drug should not be used in patients with rare hereditary disorders such as lactase deficiency, lactose intolerance, glucose-galactose malabsorption.
Clinical studies have shown that treatment with empagliflozin does not increase cardiovascular risk.
The use of empagliflozin at a dose of 25 mg does not lead to prolongation of the QT interval.
When using Jardins® together with sulfonylureas or insulin, a reduction in the dose of sulfonylureas/insulin may be required due to the risk of hypoglycemia.
Unstudied combinations of hypoglycemic drugs
Empagliflozin has not been studied in combination with GLP-1 analogues.
Monitor kidney function.
The effectiveness of Jardins® depends on kidney function. Therefore, it is recommended to monitor renal function before prescribing it and periodically during treatment (at least once a year), as well as before prescribing concomitant therapy that may adversely affect renal function.
For patients with renal failure (GFR less than 45 ml/min/1.73 m2), the drug is not recommended.
Elderly patients.
Patients aged 75 years and older have an increased risk of dehydration, so Jardins® should be administered with caution to this category of patients. These patients receiving empagliflozin were more likely to experience adverse reactions due to hypovolemia (compared to patients receiving placebo).
Experience with empagliflozin in patients over 85 years of age is limited, and therefore it is not recommended to prescribe Jardins® to patients over 85 years of age.
Use in patients at risk of developing hypovolemia.
According to the mechanism of action, taking the drug Jardins™ can lead to a moderate decrease in blood pressure. Therefore, the drug should be used with caution in cases where a decrease in blood pressure is undesirable, for example in patients with cardiovascular diseases, patients taking antihypertensive drugs (with a history of arterial hypotension), as well as in patients over 75 years of age.
If a patient taking Jardins® develops conditions that may lead to fluid loss (for example, gastrointestinal diseases), the patient's condition, blood pressure, and hematocrit and electrolyte balance should be carefully monitored. It may be necessary to temporarily stop taking the drug until water balance is restored.
Urinary tract infections.
The incidence of side effects such as urinary tract infections was comparable with empagliflozin 25 mg and placebo, and higher with empagliflozin 10 mg.
Complicated urinary tract infections (including serious urinary tract infections such as pyelonephritis and urosepsis) were reported at comparable rates in patients treated with empagliflozin and placebo. If complicated urinary tract infections develop, temporary discontinuation of empagliflozin therapy is necessary.
Laboratory urine analysis.
According to the mechanism of action, glucose is detected in the urine in patients taking Jardins®.
Impact on the ability to drive vehicles and machinery.
Clinical studies on the effect of empagliflozin on the ability to drive vehicles and operate machinery have not been conducted. Patients should be careful when driving vehicles and machinery, because When using the drug Jardins® (especially in combination with sulfonylurea derivatives and/or insulin), hypoglycemia may develop.