Human chorionic gonadotropin is a special hormone that is part of the group of glycoproteins. Human chorionic gonadotropin was first studied by science at the beginning of the twentieth century, in 1920. Subsequent studies revealed that hCG in the female body begins to be produced during pregnancy. The hormone is a product of the synthesis of placental syncytiotrophoblast and is responsible for increasing the production of progesterone, the most important hormone responsible for maintaining pregnancy. Also, due to the action of the hormone, the body of a pregnant woman stops the processes that cause menstruation. Today, human chorionic gonadotropin can be measured through blood and urine tests. It is human chorionic gonadotropin that is taken into account as an indicator in a pregnancy test.
HCG is used in medical practice to induce ovulation in women. Laboratory and clinical practice shows that by extracting hCG from the urine of pregnant women, it is possible to produce drugs for the treatment of infertility.
When should you take a β-hCG test?
Indications for use:
- early diagnosis of pregnancy;
- monitoring pregnancy over time;
- menstrual irregularities or absence of menstruation (amenorrhea);
- fetal development screening examinations;
- threat of spontaneous abortion (miscarriage), ectopic or frozen pregnancy;
- diagnosis of placental insufficiency;
- comprehensive diagnosis of hCG-producing tumors;
- monitoring the effectiveness of artificial abortion.
results
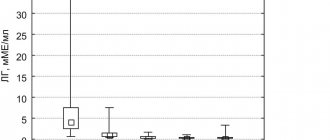
When studying the effect of HT prescribed in our study on the clinical outcomes of IVF, Menogon was used as a reference drug (playing the role of a control), with which the results of treatment using other inducers of folliculogenesis were compared. The choice of Menogon as a reference drug is justified by the fact that Menogon is the “oldest” (in terms of time of appearance on the pharmaceutical market) of those compared by G.T. It can also be recalled that other HT drugs were actually developed to improve the treatment results achieved with the use of Menogon and other first-generation menotropins. They tried to achieve this through better purification of the active components obtained from the urine of menopausal women, optimization of the composition of GT (pure FSH instead of the combination of FSH + LH) or by using alternative sources of their production (recombinant GT instead of human). In addition, Menogon was used as a reference drug also because in the cohort of patients included in our study, it was prescribed with the highest frequency - in 25.8% of all SCs (see Table 1).
Analysis of the therapeutic effectiveness of the HT drugs used showed that, in comparison with Menogon (control), none of them significantly improved, but did not worsen the results of IVF in terms of NNBSC (Table 2) and NNBPE (Table 3). It is noteworthy that an increase in the age of patients over 35 years was associated with an approximately 1.5-fold decrease in the indicators of NBISC and NNBPE, and this pattern manifested itself against the background of the use of not only the reference drug (i.e. Menogon), but also any other of the used GT.
Table 2. Clinical outcomes of IVF according to the NBSCC indicator when using the compared HT drugs Note. Here and in the table. 2-5: in parentheses - the absolute number of women out of the total number who took this drug.
Table 3. Clinical outcomes of IVF according to the NNTPE indicator when using the compared HT drugs
It can also be stated that the frequency of interruption of IVF treatment cycles at the pre-transfer stage when using Menogon and any of the HT drugs compared with it was not statistically significantly different (Table 4). This pattern was observed both in relatively young (<36 years) and older (36-42 years) women.
Table 4. Frequency of interruption of the IVF treatment cycle at the pre-transfer stage when using the compared HT drugs
When analyzing the reasons for interruption of IVF attempts at the pre-transfer stage, it was found that they had certain differences in patients of different age groups. Thus, if in patients under 36 years of age the threat of early OHSS accounted for 33.3% of the reasons for refusal of ET, then in the age group 36-42 years only 2.3% of cases of pre-transfer IVF interruption were associated with this reason ( p
<0.001).
Cases of failure to receive or lack of fertilization of oocytes, as well as the lack of oocytes suitable for ET due to defective embryogenesis, totaled 59.6% of the reasons for refusal of ET in patients under 36 years of age, while in women 36-42 years old their share increased to 91. 2% ( p
<0.001).
The reasons for refusal of IVF not related to the ongoing IVF attempt (acute or exacerbation of chronic diseases during the period of the SC, non-medical reasons that caused a change in the initial reproductive plans) accounted for approximately the same shares in the structure of all cases of pre-transfer interruption of IVF - 11.1% in patients under 36 years and 7.9% in patients 36–42 years old ( p
= 0.482).
In relation to what is presented in table. 5 of the material, it should be explained that these data characterize the cumulative (against the background of all 10 HT drugs used) structure of the causes of pre-transfer IVF interruption. It was not possible to carry out a similar analysis for each of the HT drugs used in our work due to the too small absolute number of cases of refusal of PE in the groups where the compared HT drugs were used. Nevertheless, it is logical to assume that the patterns identified in the analysis of the reasons for refusing PE in all patients who received one or another of the 10 compared HTs apply to any of the groups that were allocated taking into account the specific HT drug prescribed.
Table 5. Structure of reasons for interrupting the IVF treatment cycle at the pre-transfer stage in patients of different ages
Detailed description of the study
HCG, its structure and functions
Human chorionic gonadotropin (hCG) is a hormone that is an early indicator of pregnancy. It is secreted by the placenta and the outer membrane of the fetus - the chorion. It increases on the sixth to eighth days after conception and continues to increase in the first trimester of pregnancy.
According to the chemical structure, hCG is a protein-carbohydrate compound consisting of two parts (subunits): alpha (a) and beta (β). In the body of any person, both the whole hormone and its individual subunits are found.
In the body of a pregnant woman, human chorionic gonadotropin regulates the production of the most important hormones - progesterone and estrogens.
Progesterone contributes to the normal course of pregnancy. Since the embryo carries the father's genetic material, the woman's immune system perceives it as a foreign and potentially dangerous object and activates protective functions. Progesterone suppresses the immune response and reduces the activity of the smooth muscles of the uterus, preventing death and rejection of the fetus (miscarriage). For this reason, progesterone is often called the “pregnancy hormone.” In later stages, its level decreases, which leads to childbirth.
Estrogens are the general name for a group of hormones: estradiol, estrone and estriol. Estradiol and estrone regulate the reproductive functions of the female body and the menstrual cycle. Estriol is produced during pregnancy. It promotes active blood circulation in the placenta and supports the vital functions of the fetus.
In the first trimester of pregnancy, the level of hCG is especially important: its change can be used to judge the development of the embryo. Thus, too many hCG beta subunits in the blood may indicate chromosomal abnormalities of the fetus. A regular blood test for beta-hCG is included in the complex of periodic screening examinations.
In addition to “managing” pregnancy, hCG has other functions in the body, so small amounts of this hormone are also present in the blood of men and non-pregnant women. An abnormal increase in beta-hCG levels in such patients may indicate the development of certain diseases.
HCG in the diagnosis of pregnancy
Active synthesis of hCG begins immediately after fertilization of the egg. It can be detected in the blood within six to eight days. A blood test for beta-hCG is the most accurate method for determining pregnancy in the early stages.
In urine, unlike blood, the level of the hormone grows more slowly, varies depending on the volume of fluid consumed and is determined one to two days later. That is why rapid tests are recommended to be done a few days after a missed menstrual cycle. They are insensitive to low concentrations of hCG, and the result of such a test may depend on third-party factors: manufacturer, expiration date, storage conditions and the quality of the reagent on the test strip.
In gynecology, dynamic results of a blood test for hCG are also used to monitor the effectiveness of artificial termination of pregnancy (abortion).
HCG in pregnant women
The level of hCG in a woman’s blood begins to rise on the sixth to eighth day of the actual start of pregnancy. The concentration of the hormone reaches its maximum values in the eleventh - twelfth week, and then gradually decreases. Abnormal (both increased and decreased) beta-hCG values are possible both with incorrect determination of the gestational age and with various pathological processes.
When interpreting the results of the study, it is important to remember that the amount of hCG is estimated at the embryonic period - from the moment of last ovulation and conception. It is two to three weeks less than the obstetric period, which is calculated from the beginning of the last menstruation.
To make a diagnosis when the hCG level deviates from the norm, a series of comprehensive studies and an examination by a doctor are required.
Reduced hCG in the early stages may indicate a pathological pregnancy (frozen, ectopic), impaired placental function, or a threatened miscarriage.
The cause of elevated hCG in a pregnant woman can be multiple pregnancy, chronic diseases (diabetes mellitus), pathological pregnancy or abnormal fetal development.
In the diagnosis of chromosomal pathologies of the embryo, a free beta-hCG test is used.
HCG in the diagnosis of tumors and other pathologies
Increased hCG is observed when infected with pork tapeworm or the formation of hormone-producing tumors of internal organs: uterus, testicles, kidneys, gastrointestinal tract and lungs.
A separate cause of increased hCG in women can be not only a tumor disease, but also trophoblastic disease. It is provoked by the proliferation of trophoblast - the cells from which the outer membrane of the fetus is formed.
The development of the disease is associated with a failure of the fertilization process of the egg and the transformation of the fertilized egg into a neoplasm. Trophoblastic disease can cause the formation of a hydatidiform mole, a benign neoplasm, or choriocarcinoma, a malignant tumor prone to rapid metastasis.
To diagnose and monitor the effectiveness of treatment of tumor diseases, a free beta-hCG test is also used.
What is human chorionic gonadotropin in the male body?
The hormone is practically not present in a man’s body; high levels of gonadotropin in tests indicate a deviation from the norm or the use of appropriate medications. Basically, the use of human chorionic gonadotropin is used during the prevention of testicular atrophy during a course of anabolic steroids.
When using HCG independently, and not according to a doctor’s prescription based on tests, the following side effects are observed:
- estrogen levels increase;
- gynecomastia;
- acne;
- retention of water and salts in the body;
- sebaceous plugs;
- changes in water balance;
- completeness;
- During adolescence, bone growth stops.
The use of the hormone is prescribed strictly according to the indications of the attending physician. In this case, the doctor is obliged to inform the patient about the likelihood of the formation of oncological processes that can form during therapy in rare cases. Prescribing a course of gonadotropin is occasionally used to correct the balance of testosterone levels during menopause in men.
Problems with hCG are not uncommon. However, nowadays medicine has a sufficiently high level of development to provide assistance for such pathologies. By contacting the IVF Center clinic in Yekaterinburg, you will receive treatment from highly qualified specialists and examination using the most modern equipment.
References
- Handbook of Clinical Laboratory Testing During Pregnancy, edited by Ann M. Gronowski. Springer-Verlag LLC, New York, 2004. Prenatal Diagnosis in Obstetric Practice. MJJ Whittle, Blackwell Publishers 1995
- Laboratory and Diagnostic Tests. Joyce LeFever Kee - Pearson, Prentice Hall, 8th edition 2010
- Endocrinology of Pregnancy. Fuller W. Bazer, Humana Press 1998
- Clinical Chemistry. A Laboratory Perspective. Wendy L. Arneson, Jean M. Brickell, FADavis Company, 2007
Discussion
The results obtained allow us to note a number of obvious patterns.
First, it must be recognized that in a non-selective population of infertile patients under 42 years of age, the treatment results observed with the use of the “old” menotropin Menogon do not improve at all when prescribing the following “newer” original HT drugs:
— menotropins, characterized (according to the manufacturers) by a higher purity of active ingredients (Menopur);
- highly purified urinary FSH (Bravel),
- recombinant FSH, used alone (Gonal-F, Puregon) or in combination with recombinant LH (Pergoveris).
From this pattern it follows that all attempts by manufacturing companies to create a new original HT drug that can reliably improve the IVF results achieved when used in the non-selective population of Menogon have so far led to nothing. On the other hand, the fact that the “newer” original HT drugs were not inferior to Menogon in terms of achieved IVF effectiveness indicators indicates a completely justified possibility of using any of them at the stage of ovarian stimulation. Obviously, in such a situation, the drug of choice for SC should be exactly the one of the original HT drugs that will be offered by manufacturing companies at the most affordable price.
Secondly, our data very clearly demonstrated that Menogon’s therapeutic effectiveness in IVF cycles was not inferior to generics classified as drugs:
- highly purified urinary FSH + LH (Merional, Humog);
— highly purified urinary FSH (Alterpur).
Only with the use of the generic Follitropa, which is a generic preparation of the recombinant FSH Gonal-F (α-follitropin), there was a noticeable deterioration in treatment results in absolute values of NNBSC and NNBPE. However, even in this case, the differences in the determined indicators of the therapeutic effectiveness of IVF between patients who received treatment at S.C. Menogon and Follitrope, strictly speaking, were not reliable ( p
>0.05). It should be emphasized that the relatively small number of SCs we have performed using Follitrope does not yet allow us to come to a final conclusion about the degree of its therapeutic comparability with Menogon and other HT drugs.
The fact that IVF results are comparable when using Menogon and other original GT drugs with their generics indicates the justified possibility of prescribing reproducible drugs in the SC, i.e. Merional, Humog or Alterpur instead of their originals. As for the advisability of using generic Follitrope in the SC, this question should still be considered open until more factual material is obtained.
There is no doubt that when choosing a specific generic drug for SC, one should be guided by exactly the same principle as when choosing one or another of the original GT drugs for a similar purpose, i.e. solely by its price. This statement is based on our observations, according to which there was no statistically significant improvement (or deterioration) in the indicators of CNBSC and CNBPE when prescribing any of the original or generic HT drugs included in our study, used as an alternative to Menogon, which acted as a reference drug. Based on this pattern, in our opinion, it is completely justified when choosing GT for SC in a non-selective population to give preference to Humogu, since this particular drug is offered today in the pharmacy chain at the lowest price.
In application to the selection of HT for use in SC in “selectively” selected (by age, the presence of an increased risk of OHSS or poor response) infertility patients, it can be recalled that to date it has not been possible to prove the advisability of prescribing instead of menotropins containing a combination of urinary FSH and LH, any other types of G.T. Thus, the initially prevailing idea about the benefit of prescribing pure (recombinant or urine) FSH in the center instead of FSH + LH-containing menotropins to women with polycystic ovary syndrome, high levels of PH and the risk of OHSS was not subsequently confirmed [6, 7]. All these observations lead to the idea that in any “selectively” isolated group of infertile patients, as well as in a non-selective population, it is quite justified to prescribe menotropins (urinary FSH + LH), and not drugs of pure (urinary or recombinant) FSH or combination of recombinant FSH + LH (Pergoveris). At the same time, it makes sense to give preference to generic rather than original menotropins, i.e. Humog rather than Menogon or Menopur, since Humog provides the best price/quality ratio, taking into account its cost and the provided indicators of CNBSC and CNBPE in IVF cycles.
Separately, it should be noted that when using any of the HT drugs, there is still a possibility of cancellation of an ongoing IVF attempt at the pre-transfer stage with a frequency of approximately 10-20% of the number of S.C. If in women under 36 years of age the threat of early OHSS occupies a prominent place in the structure of the causes of such a complication, then in older patients the likelihood of discontinuation of PE is associated almost exclusively with disorders of follicle and early embryogenesis. These observations once again confirm the well-known from the literature [9, 10] provisions that the age factor (age over 36 years) worsens the ability of the ovaries to respond to gonadotropin stimulation, oocyte fertilization and early embryogenesis, but at the same time reduces the risk of early OHSS .
conclusions
1. Prescription in stimulated cycles of Menogon, Menopur, Merional, Humog, Bravel, Alterpur, Gonal-F, Puregon, Follitrope and Pergoveris is accompanied by significantly non-different IVF results in terms of NNBSC and NNBPE in a non-selective population of infertile patients no older than 42 years.
2. Of the 10 GT drugs tested in IVF programs, in terms of price/quality, the winner is Humog, which is classified as a generic that copies the original menotropins such as Menogon and Menopur.
3. Relatively less effective according to the analyzed IVF effectiveness criteria (in comparison with other HT drugs used) is Follitrop, a generic copying Gonal-F (α-follitropin).
There is no conflict of interest.