Content
- 1 Gonadotropic hormones
- 2 Secretion of gonadotropic hormones 2.1 Regulation of GnRH secretion
- 2.2 Mechanism of action of GnRH
- 5.1 Diagnostic application
- 6.1 Pregnancy test
- 7.1 Female infertility
In what cases is a hCG injection recommended?
Doctors advise resorting to injections of the hormone after receiving test results for its levels. Typically, the introduction of effective drugs is recommended in the following cases:
- Dysmenorrhea,
- Problems with the ovaries
- Disadvantages of the ovulation process,
- Problems associated with the corpus luteum
- The prospect of miscarriage
- Inability of the body to bear a child,
- Therapy before in vitro fertilization,
- Formation of placental tissue.
Medicines containing hCG are used for reproductive procedures of various specifics, since the hormone has a positive effect on the functioning of the ovaries.
Gonadotropic hormones[edit | edit code]
The gonadotropic hormones of the pituitary gland include follicle stimulating hormone (FSH)
and
luteinizing hormone (LH)
.
Chorionic gonadotropin (CG)
also affects the gonads, but is synthesized by the placenta. These three hormones, together with thyroid-stimulating hormone (TSH), are similar in structure and form the family of glycoprotein hormones. All of them consist of two subunits: the α-subunit is the same for all, and the β-subunits differ and provide specific activity. Moreover, the β-subunits of all hormones are quite similar, with the exception of the β-subunit of hCG, which contains an additional section of 30 amino acid residues at the C-terminus and several additional carbohydrate residues. Carbohydrate residues increase the half-life (T1/2) of these hormones in serum and are also involved in their binding to receptors. In humans, the gene encoding the FSH β-subunit is localized in segment 11p13, and the LH β-subunit is located in segment 19ql2.32, adjacent to at least 7 genes encoding the hCG β-subunit. The gene encoding the α-subunit of these hormones is localized in the 6q21-q23 segment.
Side effects of gonadropine
DRAW YOUR ATTENTION!!! Never use gonadotropin on PCT. This medicine is perceived by the brain in the same way as your own LH and FSH - the result will be the inability of the hypothalamus-pituitary-testicular arc to restore normal activity. That is, the gonad not only does not restore your reproductive system, but VERY actively interferes with its restoration. This is a means of preventing problems with eggs, but not a remedy after a course of therapy. PCT uses ONLY selective estrogen receptor modulators: tamoxifen, Clomid and torymifene.
As for the side effects of gonadotropin, this is, first of all, aromatization. Simply put, the gonad easily provokes gynecomastia, the accumulation of fluid under the skin and fat gain. Being a glycoprotein, that is, a peptide, if you take too much of this medicine, antibodies to it can form. That is, the gonad, in this case, stops working. This applies to those who take this drug weekly along with steroids.
We recommend reading: Melatonin: instructions for use, benefits and harms, reviews
Well, in theory, abuse of gonadotropins can provoke tumors of the gonads. I repeat that the last two points apply ONLY to those who inject themselves with excessive amounts of this substance.
And finally. Human chorionic gonadotropin is much cheaper than menopausal gonadotropin and is usually more than enough for the average amateur. But sometimes you have to combine it with menopausal gonadotropin. As I said above, this is due to disorders of the reproductive system from progestins. So, if you fall in love with nandrolones or trenbolones, I strongly recommend keeping a stash in case you need to purchase menopausal gonadotropin.
Secretion of gonadotropic hormones[edit | edit code]
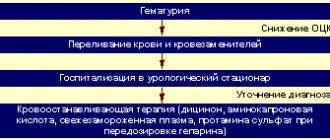
Figure 56.4.
Hypohalamic-pituitary-gonadal system The regulation of the secretion of gonadotropic hormones is described in detail in the article - sex hormones. LH and FSH are synthesized by gonadotropic cells, which make up about 20% of the secreting cells of the adenohypophysis. HCG, which is found only in humans, primates and horses, is synthesized by syncytiotrophoblast cells. The synthesis of FSH and LH is stimulated by gonadoliberin and is regulated by feedback by sex hormones (Fig. 56.4 and 58.2).
Figure 58.2. Neuroendocrine regulation of the secretion of gonadotropic hormones in women.
Regulation of GnRH secretion[edit | edit code]
Gonadotropin-releasing hormone and its analogues
Gonadotropin-releasing hormone is a hormone that stimulates the synthesis and secretion of FSH and LH by gonadotropic cells of the adenohypophysis. GnRH is formed as a result of proteolytic cleavage of a polypeptide containing 92 amino acid residues, which is encoded by a gene located in the 8p21 segment. GnRH itself is a decapeptide with an amide group at the C-terminus and a pyroglutamic acid residue at the N-terminus (Table 56.3). GnRH secretion occurs in impulses as a result of the synchronized rhythmic activity of a group of neurons located in the region of the infundibulum nucleus. The activity of these neurons begins before birth and continues for about a year after birth; then it decreases significantly, probably as a result of the inhibitory effect of the central nervous system. Shortly before the onset of puberty, the inhibitory effect of the central nervous system decreases, and the frequency and amplitude of GnRH secretion impulses increase, especially strongly during sleep. As puberty develops, GnRH secretion continues to increase until it reaches adult levels. The pulsed nature of GnRH secretion is necessary for the normal synthesis and secretion of gonadotropic hormones, the secretion of which also occurs pulsed. Constant administration of GnRH leads to desensitization and a decrease in the number of GnRH receptors on the gonadotropic cells of the adenohypophysis. This phenomenon underlies the clinical use of long-acting GnRH analogues, which suppress the secretion of gonadotropins (see below). After their administration, the secretion of LH and FSH increases briefly, but then receptor desensitization occurs and secretion decreases.
Mechanism of action of GnRH[edit | edit code]
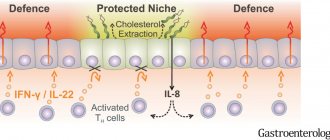
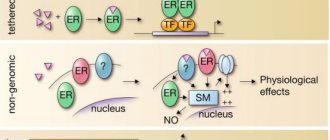
The GnRH receptor is a G-protein coupled receptor; its gene is located in segment 4q21. When GnRH or its analogues bind to the receptor, the Gq and GM proteins are activated, which, in turn, activate phospholipase C, which leads to an increase in intracellular calcium concentration. This ultimately stimulates the synthesis and secretion of LH and FSH. Although cAMP is not significantly involved in signal transduction from the GnRH receptor, activation of this receptor increases the activity of adenylate cyclase. GnRH receptors are also present in the ovaries and testes, but their physiological significance remains unknown.
Sex hormones also regulate the synthesis of LH and FSH, affecting the hypothalamus and, to a lesser extent, the pituitary gland. This regulation occurs differently in men and women and depends on age and the phase of the menstrual cycle. In women, low concentrations of estradiol and progesterone suppress the synthesis of gonadotropic hormones due to an opioid-mediated effect on neurons responsible for the impulse secretion of GnRH. However, a prolonged increase in estradiol concentration acts on the principle of positive feedback, leading to a preovulatory LH surge. In men, the synthesis of gonadotropic hormones is suppressed by testosterone, and this is partly due to its direct action, and partly due to its conversion to estradiol.
Inhibin is a peptide hormone produced in the gonads and plays an important role in regulating the secretion of gonadotropic hormones. It is synthesized by granular layer cells of the follicles in the ovaries and Sertoli cells in the testes in response to stimulation by gonadotropins and local growth factors. Inhibin acts directly on the pituitary gland, selectively suppressing the secretion of FSH, but not LG. Inhibin belongs to the same family of glycoproteins as transforming growth factor |3 and Müllerian duct regression factor.
Purpose
When should you take gonadotropin hormone? The answer to this question is also ambiguous. In Russia, it is a common practice for HGG to be injected after finishing a steroid course. I believe it would make more sense to start a course of HCG while tapering off the steroids. Let me explain: as soon as you begin to reduce your steroid intake, the body becomes increasingly testosterone deficient.
And, as a result, some loss of strength and muscle volume can be observed already at this stage, although the unique property of steroids is that they are anti-catabolic and even relatively small dosages are able to maintain muscle volume and strength even with a lack of calories, which is what they use Usually athletes are drying.
Does it make sense to conduct HGG courses in other situations? Yes, when it comes to very long steroid cycles, from three months or longer. In these cases, it is very advisable to take a two- to three-week break somewhere in the middle of the steroid course and conduct a blitz cycle of HGG. This will at least to some extent “encourage” the sex glands. Some athletes finish a steroid cycle only to give themselves a break and start a new cycle three weeks later.
Why do you need gonadotropin during a steroid cycle?
Many athletes, after long-term use of anabolic steroids, experience a drop in sexual desire. The end of a course of steroids also leads to a natural decrease in strength indicators, loss of gained muscle mass, and deterioration in physical tone. The inclusion of human chorionic gonadotropin in the regimen prevents the negative consequences of discontinuation of anabolic drugs.
It is known that a long steroid cycle can lead to a decrease in testicular volume and atrophy. This is due to a decrease in the production of your own luteinizing hormone. The introduction of hCG in recommended quantities helps eliminate this problem. Taking gonadotropin is especially important when the course of steroids exceeds 6 weeks or large doses of anabolic steroids are used.
We recommend reading: Puberty in girls: signs of onset, features of the course, duration
Most experts recommend using human chorionic gonadotropin before starting post-cycle therapy, so as not to interfere with the full recovery of the body after completing a course of steroids. During this period, it is recommended to minimize exposure to medications.
I want to lose weight
Not very long ago, one scientist from England surprised everyone with the fact that the hormone that we are now discussing is good for weight loss. Especially for drying. According to the scientist, it directs the body to use fat.
But the muscles are not going anywhere. On the contrary, they will become even more prominent. Doctors do not recommend it for regular weight loss.
The scientist encourages the use of small dosages. It's safer for the body. But you need to go on a low-calorie diet - do not eat more than 500 kcal per day. Food must be saturated with proteins and vitamins. This method is widely used by weight loss centers.
Can the substance be used instead of an anabolic steroid?
The use of HCG as a replacement for steroids is not justified and is unsafe for health. Compared to anabolic drugs, the synthetic hormone is not effective enough both in terms of building muscle mass and improving athletic performance. To enhance the effect, it is necessary to take it in high dosages (more than 4000-5000 IU weekly), which leads to irreversible consequences on the hypothalamic-pituitary-testicular axis. Negative reviews of hCG courses are associated precisely with cases of administration of the drug for purposes other than its intended purpose in volumes significantly exceeding the recommended ones. After such therapy, the likelihood of developing side effects increases significantly.
Mechanism of action of gonadotropic hormones[edit | edit code]
LH and hCG bind to the LH receptor (the gene for this receptor is located in segment 2p21), and FSH binds to its receptor (the gene for this receptor is located on the long arm of the 2nd chromosome). Both receptors are G protein coupled and have a large extracellular glycosylated domain responsible for hormone recognition. When the receptor binds to the ligand, the G protein activates adenylate cyclase, which leads to an increase in the concentration of cAMP. At a high concentration of the ligand, the receptors also activate protein kinase C through the Gq protein and increase the calcium concentration due to the activation of phospholipase C. All or almost all effects of gonadotropic hormones can be reproduced by introducing cAMP analogues into the cell, therefore the importance of protein kinase C and Ca2+ in intracellular signal transmission remains unclear.
Physiological effects of gonadotropic hormones[edit | edit code]
LH and FSH were named according to their effects on the ovaries; the function of these hormones in men was studied later. In men, LH acts on Leydig cells, stimulating the synthesis of androgens, mainly testosterone. Testosterone ensures sexual desire, the development of secondary sexual characteristics and spermatogenesis in the convoluted seminiferous tubules. FSH acts on Sertoli cells, stimulating their production of proteins and nutrients necessary for sperm maturation.
In women, the effects of FSH and LH are more complex. FSH stimulates the growth and development of follicles and also induces expression of the LH receptor gene on thekocytes and granular layer cells in the ovaries. In addition, FSH activates aromatase in the cells of the granular layer, stimulating the synthesis of estradiol. LH acts on thekocytes, stimulating the formation of androstenedione in them, the main precursor of estradiol in the ovaries of women of childbearing age. LH is also necessary for the rupture of the follicle during ovulation and for the synthesis of progesterone by the corpus luteum. Finally, the binding of LH to its receptor on granular layer cells increases the expression of the FSH receptor gene, which enhances the effect of the latter.
The importance of gonadotropic hormones in the regulation of the functions of the genital organs is clearly revealed by mutations in the genes of the hormones themselves or their receptors (Achermann and Jameson, 1999). Women with mutations in the FSH receptor genes or the β-subunit of FSH itself experience primary amenorrhea and infertility, their follicles do not mature, there are no corpora lutea and the mammary glands do not develop. These data, as well as the effectiveness of FSH in some forms of infertility (see below), eloquently indicate the important role of FSH in the functioning of the ovaries. In men with the same mutations, testicular size is reduced and oligozoospermia is observed, although in some cases fertility is preserved.
Only one case of a loss-of-function mutation of the LH β-subunit gene has been described: a 46-year-old man had no sexual development, Leydig cell hypoplasia and infertility were observed. His external genitalia were developed according to the male type, which is apparently explained by the synthesis of androgens under the influence of hCG during intrauterine development. Manifestations of loss-of-function mutations in the LH receptor gene in a male karyotype range from male hypogonadism to female-type development of the external genitalia and lack of sexual development. Probably, virilization of the external genitalia does not occur due to disruption of the action of both LH and hCG during intrauterine development. In women homozygous for mutant alleles of the LH receptor gene, primary amenorrhea or oligomenorrhea and infertility are observed, and histological examination reveals multiple ovarian cysts.
Mutations leading to permanent activation of the LH receptor occur predominantly in men and are inherited in an autosomal dominant manner. They lead to premature sexual development due to uncontrolled testosterone synthesis in the prenatal and prepubertal periods. Some of these mutations have a high risk of testicular tumors.
SHBG (SEX HORMONE BINDING GLOBULIN)
Most of the testosterone entering the blood binds to a specific transport protein - SHBG. A decrease in SHBG synthesis leads to disruption of the delivery of hormones to target organs and the performance of their physiological functions. In men, SHBG secretion increases with age. This can lead to a decrease in active testosterone and an increase in the effects of estrogen, which is manifested by gynecomastia (enlargement of the mammary glands in men) and redistribution of fatty tissue according to the female type. In women, the SHBG content is almost twice as high as in men, since estrogens increase the level of SHBG synthesis in the liver, and androgens, on the contrary, reduce its production. Indications for the analysis: In both sexes: clinical signs of an increase or decrease in androgen levels with normal testosterone levels, baldness, acne, oily seborrhea. In women: hirsutism, anovulation, amenorrhea, polycystic ovary syndrome, prediction of the development of preeclampsia (SHBG is reduced). In men: male menopause, chronic prostatitis, impaired potency, decreased libido. An increase in SHBG levels can be observed with thyrotoxicosis, liver cirrhosis, taking estrogens and oral contraceptives. A decrease in SHBG levels can occur with hypothyroidism, obesity, acromegaly, Cushing's syndrome, hyperprolactinemia, polycystic ovary syndrome, and after taking androgens. Preparation for the study: on an empty stomach.
The use of GnRH and its analogues[edit | edit code]
In table 56.3 lists synthetic analogues of GnRH used in the clinic. Synthetic GnRH is called gonadorelin. Substitution of the amino acid residue at position 6 protects GnRH analogues from proteolysis, and substitution of the C-terminal residue increases affinity for the receptor. Such analogues have greater activity and a longer action compared to native GnRH, whose T1/2 is only 2-4 minutes.
GnRH antagonists, unlike their long-acting analogues, do not cause a transient increase in serum gonadotropin levels. Modern GnRH antagonists do not appear to lead to local and systemic histamine release and anaphylactic reactions, which limited the use of the first drugs in this group. Two GnRH antagonists, gairelix and cetrorelix, are used in in vitro fertilization to suppress the LH surge during ovarian stimulation. Ganirelix is available in the US, while Cetrorelix is only available in Europe. Theoretically, rapid suppression of LH surge allows for better control of ovarian stimulation (see below) and thereby shortens the artificial insemination cycle. However, the practical value of these drugs in artificial insemination remains to be clarified in clinical trials.
Diagnostic application[edit | edit code]
One of the gonadorelin preparations (gonadorelin hydrochloride) is used for the differential diagnosis of pituitary and hypothalamic lesions in secondary hypogonadism. Serum LH levels are measured before administration of gonadorelin at a dose of 100 μg subcutaneously or intravenously and within 2 hours (15, 30, 45, 60 and 120 minutes) after administration. An increase in LH secretion indicates the presence of functioning gonadotropic cells of the adenohypophysis. With prolonged deficiency of GnRH, the sensitivity of gonadotropic cells to it may decrease, so a low LH level during a test with GnRH does not necessarily indicate damage to the pituitary gland. The GnRH test can also be used to differentiate between true (associated with GnRH secretion) and false precocious puberty.
Infertility treatment[edit | edit code]
Another gonadorelin drug (gonadorelin acetate) is used for reproductive disorders associated with GnRH deficiency. The drug is administered intravenously using a special infusion pump in a pulse mode that simulates physiological secretion, 2.5 mcg every 60-90 minutes. If ovulation does not occur, the dose administered per pulse can be gradually increased to 10 mcg. The principles of administration and dosage are specified in the manufacturer's instructions. Gonadorelin is less likely than gonadotropic hormones to cause multiple pregnancies. When treating with gon-dorelin, it is not necessary to so carefully monitor the level of estrogen in the serum and perform ultrasound of the ovaries. Adverse reactions occur rarely; most often phlebitis develops at the injection site. When treated with gonadorelin, the physiological secretion of sex hormones is restored in women, the menstrual cycle is established and ovulation occurs. However, due to technical complexity, this treatment method is used only in specialized clinics (Hayes et al., 1998).
In case of infertility in men, gonadorelin can be used to achieve testicular growth, normal secretion of sex hormones and spermatogenesis. However, the method is relatively expensive and requires constant wearing of an infusion pump. In addition, gonadorelin is not approved by the FDA for the treatment of male infertility. Therefore, preference is usually given to gonadotropic hormones.
Long-acting GnRH analogs are also used for ovulation induction. These drugs suppress the preovulatory LH surge and prevent luteinization of the nonovulating follicle. Several treatment regimens have been developed in which GnRH analogs are administered long-term or short-term together with gonadotropic hormones that ensure follicle maturation (see below), and then hCG is prescribed to induce ovulation (Lunenfeld, 1999).
Suppression of the secretion of gonadotropic hormones[edit | edit code]
As already mentioned, long-acting GnRH analogues lead to desensitization of GnRH receptors, as a result of which the secretion of gonadotropic and, accordingly, sex hormones is sharply reduced. This “medical castration” has proven to be very convenient in cases where it is necessary to reduce the production of sex hormones. An obvious indication for such treatment is true precocious puberty in children, in which long-term administration of GnRH analogues is very effective and is almost not accompanied by adverse reactions.
Long-acting GnRH analogs are used for the palliative treatment of hormone-dependent tumors (for example, prostate or breast cancer); Since at the beginning of treatment these drugs sharply increase the secretion of sex hormones, at the same time drugs are prescribed that disrupt the synthesis or block the action of sex hormones. In addition, long-acting GnRH analogs are used for other hormone-dependent diseases (endometriosis, uterine fibroids and acute intermittent porphyria). Finally, for medical castration in mental disorders such as pedophilia, when the risk of non-compliance with medical prescriptions is very high, goserelin is especially convenient, which is administered at a dose of 10.8 mg subcutaneously once every 3 months.
Long-acting GnRH analogues are generally well tolerated and cause quite predictable side effects due to disruption of the synthesis of sex hormones: hot flashes, vaginal dryness, atrophic vaginitis, decreased bone density. In this regard, for diseases such as endometriosis and uterine fibroids, treatment is usually continued for no more than 6 months or additional estrogens are prescribed to maintain bone density.
Rules for taking human chorionic gonadotropin during and after completion of the course
You can purchase human chorionic gonadotropin without any prescription at the pharmacy. It is produced in the form of injections for administration subcutaneously or intramuscularly. The drug is first diluted using a special liquid included with it inside the ampoule. The injections are injected into the muscles. The substance dissolves very quickly and lasts for at least five to six days.
We recommend reading: Estrogen tablets for women: reviews and how much do the drugs cost?
Dosage regimen
If we talk about how much hCG should be administered, then I can only give rough recommendations. For example, the well-known Bill Phillips advises taking 4000 IU (International Units) per week for two to three weeks. However, there are other recommendations according to which the use of hCG should be approached individually, based on how long the steroid course was, how high the dosage was and what drugs were used. And if, for example, the basis of your steroid menu was “methane” and sustanon, then in this case the dosage of HGG should be higher.
Another question concerns how often to give gonadotropin injections. One of the favorite models of Russian bodybuilders is the option in which 1000-1500 IU of gonadotropin is administered every second day. On the other hand, according to research by scientists, a single injection of hCG of approximately 1500 IU increases plasmatestosterone levels by 250-300% and this level lasts for several days (up to five to six). Therefore, it is possible that more infrequent injections, say once every five days, would be more appropriate. If we talk about the period during which one should “sit” on gonadotropin, then almost all sources are unanimous: no more than three, maximum four weeks.
Otherwise, the testicles will react very poorly to injections of hCG and even to their own release of luteinizing hormone, which can lead to hypofunction of the gonads. At the same time, the pauses between courses of gonadotropin, according to the same Phillips, should be at least six months, although for a bodybuilder. If you are on steroids for eight to ten months a year, this condition is difficult to achieve.
Diagnostic use of gonadotropic hormones[edit | edit code]
Pregnancy test[edit | edit code]
HCG is present in large quantities in the blood and urine of pregnant women, so immunochemical detection of the β-subunit of hCG can be used as a pregnancy test. Qualitative determination of the β-subunit of hCG in urine is the basis of home pregnancy tests sold over the counter in the United States. These tests can quickly detect pregnancy within a few days after a missed period.
Quantitative determination of the concentration of hCG in plasma for clinical and scientific purposes is carried out using RIA. This is usually done to assess the progression of pregnancy, or if an ectopic pregnancy, hydatidiform mole or choriocarcinoma is suspected.
Determining the time of ovulation[edit | edit code]
Ovulation occurs 36 hours after the onset of the LH surge and 10-12 hours after its peak concentration is reached. Therefore, the concentration of LH in the urine can predict the time of ovulation. Kits are produced for home use that allow semi-quantitative assessment of LH levels in urine using specific antibodies. The test is performed every 12 or 24 hours starting from the 11th day of the cycle (with a 28-day cycle) and the expected time of ovulation is determined by the increase in LH levels. This makes it possible to increase the likelihood of conception by choosing the right time for sexual intercourse.
Diagnosis of reproductive function disorders[edit | edit code]
Quantitative measurement of FSH and LH levels in plasma using the RIA method (based on the level of β-subunits) is used to diagnose certain reproductive disorders. Low or undetectable levels of FSH and LH indicate secondary hypogonadism and damage to the pituitary gland or hypothalamus. In primary hypogonadism, the levels of these hormones, on the contrary, are high. With amenorrhea in women or delayed puberty in men and women, determining the level of FSH and LH makes it possible to distinguish damage to the gonads from damage to the hypothalamic-pituitary system.
The level of FSH on the 3rd day of the menstrual cycle can be used to judge fertility. Even with a normal menstrual cycle, an FSH level of 15 IU/ml or more indicates low fertility, and the success of artificial insemination is unlikely (see below).
The hCG test is used in men to assess the function of Leydig cells based on the degree of stimulation of testosterone synthesis. This test is used if there is a suspicion of dysfunction of Leydig cells (for example, with delayed sexual development). Serum testosterone levels are determined after several injections of hCG. Reduced secretion of testosterone indicates a pathology of Leydig cells, and normal secretion indicates damage to the hypothalamic-pituitary system.
PROGESTERONE
Progesterone is a female sex hormone produced in the corpus luteum of the ovaries and adrenal glands. Outside of pregnancy, progesterone secretion begins to increase in the preovulatory period, reaching a maximum in the middle of the luteal phase, returning to its original level at the end of the cycle. The content of progesterone in the blood of a pregnant woman increases, doubling by 7-8 weeks, and then gradually increasing until 37-38 weeks. After ovulation - the release of an egg from the follicle - a corpus luteum is formed in its place in the ovary - a gland that secretes progesterone. It exists and secretes this hormone during 12-16 weeks of pregnancy until the moment when the placenta is fully formed and takes over the function of hormone synthesis. If conception does not occur, the corpus luteum dies after 12-14 days, and menstruation begins. Progesterone is determined to assess ovulation and the viability of the corpus luteum. With a regular cycle - a week before menstruation, when measuring rectal temperature - on the 5-7th day of its rise; with an irregular cycle - several times. A sign of ovulation and the formation of a full-fledged corpus luteum is a tenfold increase in progesterone levels. Indications for the analysis : identifying the causes of menstrual irregularities, infertility, dysfunctional uterine bleeding, assessing the condition of the placenta in the second half of pregnancy, differential diagnosis of true post-term pregnancy. An increase in progesterone levels is observed with adrenal hyperplasia, corpus luteum cyst, pregnancy, and delayed maturation of the placenta. The analysis will show a decrease in progesterone levels in the absence of ovulation, insufficiency of the corpus luteum, true postmaturity, placental insufficiency, intrauterine growth restriction, or threatened abortion. Preparation for the study: the analysis is carried out on the 22-23rd day of the menstrual cycle, unless other dates are indicated by the attending physician. Blood is taken in the morning on an empty stomach, that is, when 8-12 hours pass between the last meal and blood collection. You can drink water.
Therapeutic use of gonadotropic hormones[edit | edit code]
Initially, gonadotropic hormones for clinical use were obtained from human pituitary glands (cadaveric material) and from the urine of women. Pituitary preparations are not currently used due to the risk of transmission of the causative agent of Creutzfeldt-Jakob disease. Several drugs are obtained from urine. HCG, which is similar in action to LG, is obtained from the urine of pregnant women. The drug menotropin is obtained from the urine of postmenopausal women, which contains approximately equal amounts of LH and FSH, as well as other urine proteins. Since menotropin is relatively poorly purified, it is administered intramuscularly to avoid allergic reactions. Another drug, urofollitropin, is purified FSH obtained by removing LH by immunological methods. Ultra-highly purified urofollitropin is obtained using monoclonal antibodies to FSH. It is purified so much that it can be administered subcutaneously.
Using genetic engineering methods, a mammalian cell line was obtained that synthesizes the a- and p-subunits of FSH. The resulting recombinant FSH is close in the nature of glycosylation to native FSH. Today, two recombinant FSH preparations are produced - follitropin A and follitropin P; their carbohydrate structures are slightly different. Both of these drugs are administered subcutaneously because they are much purer than urine-derived drugs and are much better standardized. Recombinant drugs are much more expensive than native ones, but there is no evidence yet that they are more effective or less likely to cause adverse reactions such as ovarian hyperstimulation syndrome. It is likely that in the future, using genetic engineering methods, it will be possible to obtain analogues of gonadotropic hormones with a longer action and with higher activity.
Female infertility[edit | edit code]
About 10% of married couples of childbearing age suffer from infertility. Gonadotropin hormones are increasingly used to treat infertility (Vollenhoven and Healy, 1998); They are often used for artificial insemination. Although the main indication for their use is chronic anovulation as a result of secondary hypogonadism (group 1 according to the WHO classification), gonadotropic hormones are also used to induce ovulation in polycystic ovary syndrome (group II according to the WHO classification) in cases where clomiphene is ineffective (Chapter 58 ). In addition, gonadotropic hormones are used for infertility against the background of normal ovulation, although in these cases treatment with clomiphene is first tried. Doctors with sufficient experience in treating infertility and endocrine disorders should prescribe gonadotropic hormones.
In chronic anovulation, administration of FSH alone induces ovulation in most cases. Typically, FSH is prescribed at a dose of 75 IU/day during the first 6-7 days of the cycle, after which the number and size of maturing follicles are assessed using vaginal ultrasound. Ultrasound is usually performed every 2-3 days. Follicle maturation is considered adequate if a follicle with a diameter of 18 mm is detected. If three or more follicles with a diameter of more than 16 mm are detected, FSH is discontinued due to the risk of ovarian hyperstimulation syndrome (see below) and barrier methods of contraception are used to prevent multiple pregnancies. The concentration of estradiol is also determined, which should be in the range of 500-1500 pg/ml. Lower values indicate insufficient ovarian stimulation, while higher values indicate the risk of ovarian hyperstimulation syndrome. If ovarian stimulation is insufficient, the dose of FSH can be increased to 150 IU/day.
To complete follicle maturation and induce ovulation, hCG is prescribed the day after FSH is discontinued at a dose of 5,000–10,000 IU. When treated with gonadotropic hormones, multiple pregnancies develop in 10-20% of cases, which is associated with the development of several tertiary follicles and the release of several eggs.
Gonadotropic hormones are used in artificial insemination, including in vitro fertilization and microinjection of sperm into the cytoplasm of the egg. With the help of FSH, the development of follicles is stimulated, and for their final maturation, hCG is prescribed, after which mature eggs are surgically removed from the tertiary follicles. Then, in vitro fertilization of the resulting eggs is performed using sperm or microinjection of sperm into the cytoplasm of the egg. The embryos are transferred into the uterus or fallopian tube. With artificial insemination, the risk of multiple pregnancy depends on the number of embryos transferred.
In addition to multiple pregnancies and its possible complications, the main side effect of gonadotropins is ovarian hyperstimulation syndrome. This syndrome is characterized by rapid accumulation of fluid in the peritoneal cavity, pleural cavity and even the pericardium. It is believed that the cause of this syndrome is the release of a substance by the ovaries that increases vascular permeability. Ovarian hyperstimulation syndrome is characterized by bloating, abdominal pain, nausea, vomiting, diarrhea, severe ovarian enlargement, shortness of breath and oliguria. Ovarian hyperstimulation syndrome can be complicated by hypovolemia, fluid and electrolyte disturbances, hemoperitoneum, ARDS, thromboembolism and liver dysfunction. If the development of this syndrome is suspected, hCG is not prescribed.
Some studies have suggested that gonadotropins increase the risk of ovarian cancer, but this remains unproven. It is important to note that ovarian stimulation with FSH and menotropin does not increase the risk of malformations in children born from stimulated eggs.
Male infertility[edit | edit code]
Treatment with gonadotropic hormones can be effective if the cause of infertility is their deficiency. Since gonadotropic hormones are relatively expensive, and long-term use can lead to resistance to them, sexual development is usually stimulated with androgens, and gonadotropins are used later to achieve fertility itself.
Treatment, as a rule, begins with the administration of hCG in a dose of 1000-5000 IU intramuscularly 3 times a week until the synthesis of sex hormones is normalized, as judged by clinical signs and plasma testosterone levels. After this, the dose of hCG is reduced to 2000 IU 2 times a week and menotropin is additionally administered at a dose of 75-150 IU LH and FSH 3 times a week. The most common side effect of gonadotropins is gynecomastia; it occurs in almost every third patient and is probably associated with increased production of estrogen: It takes approximately 6 months for the testicles to mature, and to establish full spermatogenesis, treatment must be continued for up to 2 years. After the onset of spermatogenesis or its resumption (in case of secondary hypogonadism that occurs after puberty), maintenance therapy with hCG is sufficient for sperm production. As already mentioned, recombinant gonadotropins are likely to play an increasingly important role in the treatment of infertility.
Cryptorchidism[edit | edit code]
With cryptorchidism, one or both testicles do not descend into the scrotum. In full-term newborn boys, it occurs in 3% of cases, but with age its prevalence decreases markedly. With cryptorchidism, spermatogenesis is disrupted and the risk of testicular germ cell tumors increases. Therefore, it is believed that the removal of the testicle into the scrotum should be done as early as possible, usually at the age of one year and in any case before 2 years. Since testicular descent is stimulated by androgens, hCG can be used in the absence of an anatomical obstruction. Usually 6 injections of hCG, 500 IU/m2 IM, are prescribed every other day. If such treatment is ineffective, orchiopexy is performed.
PROLACTIN
Prolactin is a hormone produced in the anterior pituitary gland; a small amount is synthesized in peripheral tissues, and during pregnancy it is also produced in the endometrium. This hormone plays an extremely important role in many processes occurring in the body, in particular, in ensuring the normal functioning of the reproductive system. Prolactin also contributes to the formation of sexual behavior. It regulates water-salt metabolism, delaying the excretion of water and sodium by the kidneys, stimulates calcium absorption, and has a modulating effect on the immune system. In general, prolactin activates anabolic processes in the body. The daily secretion of prolactin has a pulsating character. During sleep, its level increases. After waking up, the concentration of prolactin decreases sharply, reaching a minimum in the late morning hours. After noon, the hormone level increases. In the absence of stress, daily fluctuations in levels are within normal values. During the menstrual cycle, prolactin levels are higher in the luteal phase than in the follicular phase. From the 8th week of pregnancy, prolactin levels increase, reaching a peak at 20-25 weeks, then decrease immediately before childbirth and increase again during lactation. During pregnancy, prolactin supports the existence of the corpus luteum and the production of progesterone, stimulates the growth and development of the mammary glands and milk formation. An increase in prolactin levels is one of the common causes of infertility. Indications for the analysis: galactorrhea, cyclical pain in the mammary gland, mastopathy, anovulation, oligomenorrhea, amenorrhea, dysfunctional uterine bleeding, infertility, diagnosis of sexual infantilism, chronic inflammation of the internal genital organs, severe menopause, obesity, decreased libido and potency (men) , gynecomastia (men), osteoporosis. The analysis shows an increase in prolactin levels in diseases of the hypothalamus, pituitary gland, primary hypothyroidism, polycystic ovary syndrome, chronic renal failure, cirrhosis of the liver, adrenal insufficiency and congenital dysfunction of the adrenal cortex; tumors that produce estrogen and other conditions. The level of prolactin in the blood is usually reduced in case of pituitary insufficiency, true post-term pregnancy. Preparation for the study: Avoid sexual intercourse and heat exposure (sauna) 1 day before, smoking 1 hour before. Since prolactin levels are greatly influenced by stressful situations, it is advisable to exclude factors that influence the research results: physical stress (running, climbing stairs), emotional arousal. Therefore, before the procedure you should rest for 10-15 minutes and calm down.