Paroxysmal supraventricular tachycardia, abbreviated as PVT, is a type of arrhythmia. Accompanied by a heart rate (HR) from 140 to 220 or more beats per minute. It arises spontaneously and ends unexpectedly. The duration of PNT is at least three cardiac cycles, while maintaining a regular heart rhythm. The attack itself can last from a few seconds to several days.
PNT occurs due to disruption of the nervous regulation of cardiac activity or damage to other organs.
In the first case, excessive nerve stimulation leads to an increase in heart rate.
PNT can also occur in healthy people under the influence of certain factors:
- prolonged physical activity;
- stress;
- consumption of energy and stimulant drinks;
- bad habits.
In the case of organic damage, paroxysmal supraventricular tachycardia can be caused by:
- damage to the heart muscle due to ischemia, inflammation, intoxication;
- myocardial infarction;
- heart disease;
- pathology of the cardiac conduction system.
In addition to heart disease, other organs can affect paroxysmal supraventricular tachycardia. It is worth checking the functioning of the kidneys, lungs and gastrointestinal tract, especially if there are chronic or acute diseases.
What is paroxysmal tachycardia?
As a rule, attacks of paroxysmal tachycardia begin and end suddenly and have different durations.
They make the heart work uneconomically, reduce the efficiency of blood circulation, and lead to its failure. According to the mechanism of development and etiology, paroxysmal tachycardia resembles extrasystole. Therefore, cardiologists regard successive extrasystoles as a short attack of tachycardia.
Classification of paroxysmal tachycardia
1. Based on the location of ectopic impulses, doctors distinguish:
- atrial paroxysmal tachycardia;
- atrioventricular (atrioventricular) paroxysmal tachycardia;
- ventricular paroxysmal tachycardia.
In turn, atrioventricular and atrial tachycardia are combined into a supraventricular or supraventricular form.
2. Taking into account the nature of the course, the following types of paroxysmal tachycardia are distinguished:
- chronic (constantly recurrent);
- spicy;
- continuously relapsing (lasts for years, can cause circulatory failure and dilated, arrhythmogenic cardiomyopathy).
3. According to the characteristics of the development mechanism, paroxysmal supraventricular tachycardia is classified into:
- focal (ectopic);
- reciprocal (associated with the re-entry mechanism in the sinus node);
- multifocal (multifocal).
In children, paroxysmal tachycardia manifests itself in the same way as in adults.
Our doctors
Kedrinskaya Larisa Ivanovna
Experience 18 years / Doctor of the highest category, Candidate of Medical Sciences / General practitioner, cardiologist
Sign up
Vershuta Elena Vasilievna
More than 23 years of experience / Doctor of the highest category, Candidate of Medical Sciences / Cardiologist, therapist
Sign up
+
Causes of paroxysmal tachycardia
Supraventricular paroxysmal tachycardia occurs as a result of increased activation of the sympathetic nervous system. Ventricular is a consequence of necrotic, inflammatory, sclerotic or dystrophic damage to the heart muscle.
In the ventricular form, the focus of ectopic excitation is located in the His bundle, its legs and Purkinje fibers, that is, in the ventricular sections of the conductive nervous system. Most often, the pathology is diagnosed in elderly men who have suffered a myocardial infarction, coronary heart disease, or suffer from hypertension, myocarditis, or heart defects.
The main causes of the development of paroxysmal tachycardia also include:
1. The presence of additional innate impulse pathways in the myocardium. That is:
- Kent's bundle between the atria and ventricles, bypassing the atrioventricular node;
- Macheim fibers between the atrioventricular node and the ventricles.
2. The presence in the myocardium of additional impulse pathways resulting from myocardial damage (infarction, myocarditis, cardiomyopathy).
3. Additional pathways cause pathological movement of excitation throughout the myocardium.
Cardiology knows cases when longitudinal dissociation appears in the atrioventricular node, causing uncoordinated functioning of the fibers of the atrioventricular connection. Then some of the fibers function normally, while the other, on the contrary, conducts excitation in the retrograde (opposite) direction and acts as the basis for the circular circulation of impulses from the atria to the ventricles and along the opposite fibers back to the atria.
In young children, essential (idiopathic) paroxysmal tachycardia of unknown etiology is sometimes diagnosed.
Symptoms of paroxysmal tachycardia
An attack of paroxysmal tachycardia always begins and ends suddenly. Its duration can range from several minutes to several days. The patient feels an incomprehensible “push” in the area of the heart. Then the heartbeat increases sharply and reaches 120-220 beats/min. The correct heart rhythm is maintained.
Paroxysm may be accompanied by:
- noise in the head;
- dizziness;
- a feeling of squeezing of the heart.
In some cases, neurological focal symptoms occur - hemiparesis, aphasia.
Paroxysm of supraventricular tachycardia is often manifested by autonomic dysfunction, which is characterized by:
- nausea;
- sweating;
- flatulence;
- low-grade fever.
When the attack ends, polyuria (increased urine production) is observed after a few hours. If paroxysmal tachycardia is prolonged, blood pressure may decrease, severe weakness, and fainting may occur.
If you notice similar symptoms, consult a doctor immediately. It is easier to prevent a disease than to deal with the consequences.
Expert advice
In the prevention of VT attacks, eliminating the cause plays an important role. Therefore, I strongly recommend that my patients quit smoking, limit their consumption of coffee and alcohol, and avoid extreme stress and excessive physical activity. It is also necessary to conduct an examination to identify a disease that could provoke the development of arrhythmia, and its proper treatment (IHD, CHF, diffuse toxic goiter, etc.). It is important to remember that tachycardia is either a normal reaction of the body to stress or a symptom of heart damage. For this, the fact of observing yourself and your rhythm is important. If you notice an increase in the frequency of attacks, make an appointment with your doctor, first noting for yourself in what conditions tachycardia appears.
In cases where there is no obvious connection, the doctor will recommend that you undergo examinations. The first step in solving the problem of pathological tachycardia will be to get rid of any factors that can cause it in a healthy person, that is, stress. Stay calm and take care of yourself is important advice in treating arrhythmias.
Diagnosis of paroxysmal tachycardia
Paroxysmal tachycardia is recognized by the typicality of the attack (sudden onset and sudden end) and data obtained from a cardiac examination. The supraventricular and ventricular forms differ in the degree of increase in heart rate:
- with ventricular tachycardia, the heart rate is up to 180 beats/min, tests with excitation of the vagus nerve are negative;
- with supraventricular tachycardia, the heart rate is about 220-250 beats/min, the attack is easily stopped by excitation of the vagus nerve.
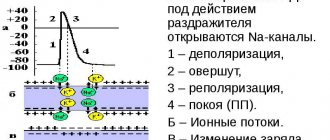
An ECG with paroxysmal tachycardia shows a change in the polarity and shape of the P wave, as well as a violation of its location in relation to the ventricular QRS complex. These signs allow us to judge what form of the disease we are talking about.
Thus, an ECG with atrial paroxysmal tachycardia shows the location of the positive/negative P wave in front of the QRS complex. If the paroxysm comes from the atrioventricular junction, a negative P wave is recorded, located behind/merging with the QRS complex. An ECG with ventricular paroxysmal tachycardia registers expansion and deformation of the QRS complex, and an unchanged P wave can also be recorded.
Paroxysmal tachycardia cannot always be detected using an ECG. Then cardiologists resort to daily ECG monitoring, which allows them to observe short episodes of attacks that are not subjectively felt by the patient.
In order to exclude organic cardiac pathology, the following are additionally carried out:
- MRI;
- Ultrasound of the heart;
- MSCT of the heart (layer-by-layer scanning of cardiac structures).
In some cases, an endocardial electrocardiogram is recorded by inserting electrodes into the heart.
Clinical case
A 34-year-old woman came to my clinic for an appointment with complaints of attacks of rapid heartbeat, accompanied by a feeling of lightheadedness and slight dizziness.
These symptoms began to bother the patient about 2 months ago. The woman also noted that she had recently become irritable and her sleep had worsened. General examination revealed an irregular pulse and an enlarged thyroid gland. The patient underwent an ECG, which showed no pathological changes. The patient was referred for consultation to a cardiologist and endocrinologist. The cardiologist performed Holter ECG monitoring, which revealed paroxysms of monomorphic atrial tachycardia with a heart rate of up to 160/min. Ultrasound and thyroid hormones prescribed by the endocrinologist showed signs of autoimmune thyroiditis - diffuse enlargement of the thyroid gland, decreased TSH levels, high concentrations of T4 and antibodies to TPO.
A diagnosis of Hashimoto's thyroiditis, thyrotoxic phase, paroxysmal PT was made. Beta blockers were prescribed to reduce heart rate, and further observation by an endocrinologist was indicated to monitor hormonal levels and replacement therapy.
Treatment of paroxysmal tachycardia
The treatment regimen for paroxysmal tachycardia depends on:
- forms of arrhythmia (ventricular, atrial, atrioventricular);
- reasons that caused the disease;
- duration and frequency of paroxysms;
- presence/absence of complications.
Attacks of paroxysmal tachycardia require emergency hospitalization (with the exception of idiopathic variants with a benign course, which are easily stopped by administering an antiarrhythmic drug to someone).
For the treatment of the supraventricular form, complicated by cardiovascular or heart failure, patients are hospitalized in the cardiology department. Planned hospitalization is carried out if attacks recur more often than 2-3 times a month. Then the question of the relevance of surgical intervention is decided.
Emergency care for paroxysmal tachycardia includes intravenous administration of antiarrhythmic drugs (Propranolol, Aymalin, Rytmodan, Quinidine, Ethmozin, Cordarone, Isoptin, etc.). If the attack is prolonged and cannot be controlled with medications, electropulse therapy is performed. Then the patient undergoes outpatient cardiological treatment, during which effective antiarrhythmic drugs are selected.
To relieve paroxysmal tachycardia, doctors often use vagal maneuvers - techniques that have a pronounced mechanical effect on the vagus nerve. These include:
- straining;
- Aschner's test (moderate and uniform pressure on the inner upper corner of the eyeball);
- Valsalva maneuver (vigorous exhalation with the mouth and nasal cavity closed);
- irritating the root of the tongue to trigger a gag reflex;
- Chermak-Hering test (uniform pressure on the carotid sinuses in the area of the carotid artery).
If attacks of paroxysmal tachycardia occur several times a month, the patient is prescribed long-term anti-relapse therapy:
- quinidine preparations (Disopyramide, Kinylentine, Amiodarone, Verapomil, etc.);
- cardiac glycosides (Celanide, Digoxin).
The selection of an effective dosage is carried out taking into account the patient’s well-being and ECG results.
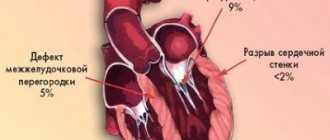
Surgical treatment of paroxysmal tachycardia is used only if the disease is severe and cannot be controlled with medications. Among the most common surgical methods are:
- mechanical, laser, electrical, cryogenic, chemical destruction of additional impulse pathways or ectopic foci of automatism;
- RFA;
- implantation of a pacemaker;
- implantation of an electrical defibrillator.
If a patient wants to treat paroxysmal tachycardia using traditional methods, he should first consult with a cardiologist, since failure to take prescribed antiarrhythmic drugs can lead to serious complications.
Diet for paroxysmal tachycardia
Patients with paroxysmal tachycardia should monitor blood sugar and cholesterol levels and maintain normal body weight. It is recommended that they take food in small portions 4-5 times a day. This is explained by the fact that overeating leads to irritation of the nerve receptors that are responsible for the functioning of the heart, and this is fraught with attacks of tachycardia.
You can't eat late at night. The last meal should be no later than 2-3 hours before going to bed. Exclude from the diet:
- coffee Tea;
- products containing large amounts of sugar, starch;
- sweets, baked goods;
- fatty foods (lard, mayonnaise, fatty meat, butter).