Early ventricular repolarization syndrome does not belong to any arrhythmias according to the clinical and functional classification of cardiologists. The electrocardiographic phenomenon has a typical picture, recorded graphically, but is not considered a disease. Sometimes changes are not considered a pathology at all. They are characteristic of healthy people and do not require treatment.
The danger lies in the unpredictability of further physiological abnormalities in the heart muscle, as well as in the combination of early ventricular repolarization syndrome with serious heart pathology. Therefore, its detection on an ECG requires careful examination by a cardiologist and observation.
What changes in the heart cause the syndrome?
Normal repolarization is caused by the process of the predominant exit of potassium from the cell over the entry of sodium ions into the cell. Due to this, a positive charge appears on the outside and a negative charge on the inside. This mechanism for stopping the excitation of one fiber spreads in the form of an impulse to neighboring areas like a chain reaction; it corresponds to the diastole phase.
Repolarization prepares the myocardium for the next systole and ensures the excitability of muscle fibers. The contraction (depolarization) phase of the heart depends on its quality and duration. These electrical changes have their own direction. They begin in the septum between the ventricles, then spread to the myocardium, first of the left, then of the right ventricle.
Premature repolarization disrupts the balance of electrolyte metabolism and changes the conduction of impulses along conductive pathways
Existing hypotheses explain early repolarization by the presence of three types of cells with different electrophysiological potentials. They are named by their location in the layers of the heart wall:
- epicardial,
- endocardial,
- M cells.
Experimental data have been obtained on the creation of prerequisites for re-excitation in these structures. The role of the endings of the autonomic nervous system in early repolarization (sympathetic and vagus nerve fibers) cannot be ruled out. The activating effect of the sympathetic nerve on the repolarization of the anterior wall and apex zone is shown.
Pathogenesis
Contraction of the chambers of the heart occurs as a result of changes in the electrical charge in myocardial cells - cardiomyocytes . As a result, sodium, calcium and potassium ions move into the intercellular space and back. The process is carried out in alternating main phases:
- depolarization – contraction;
- repolarization is relaxation before a new contraction.
Early repolarization of the ventricles is formed as a result of improper conduction of the impulse through the conduction system of the heart from the atria to the ventricles. To transmit the electrical impulse, abnormal conduction pathways . The development of the phenomenon is due to an imbalance between repolarization and depolarization in the basal regions and apex of the heart. Characterized by a significant reduction in the period of myocardial relaxation. On the ECG, along with the SRRS, a disturbance of repolarization processes in the myocardium is often recorded, in particular, a violation of the repolarization of the lower wall of the left ventricle.
What meaning do clinicians attach to the syndrome?
No typical symptoms and complaints of patients with the syndrome have been identified. However, the signs identified on the ECG cannot be safely attributed to the manifestations of the norm. The syndrome of early ventricular repolarization is known for “simulating” the picture of myocardial infarction, making it difficult to diagnose hypertrophy and dystrophic changes.
In patients, it can be detected simultaneously with rhythm disturbances such as:
- paroxysmal supraventricular tachycardia,
- attacks of atrial fibrillation,
- extrasystoles.
The danger lies in the transition of an attack of fibrillation into ventricular fibrillation with a fatal outcome.
This causes special attention in clinical monitoring of patients with ECG changes such as early repolarization syndrome.
Classification
In children and adults, early ventricular repolarization syndrome can have 2 development options:
- without damage to the cardiovascular system;
- with defeat.
According to the nature of the flow, they are distinguished:
- transitory form;
- permanent form.
Depending on the location of the ECG signs of SRGC, they are divided into 3 types.
- I characteristic signs are observed in a healthy person. ECG signs are recorded only in chest leads V1, V2. The likelihood of complications developing is extremely low.
- II ECG signs are recorded in the inferolateral and lower sections, leads V4-V6. The risk of complications is increased.
- III ECG changes are recorded in all leads. The risk of complications is the highest.
Risk factors and causes
The reasons for extraordinary repolarization, in addition to additional bypass paths of the impulse, are considered:
- neuroendocrine diseases (most common in childhood);
- increased manifestations during sleep and when the influence of the vagus nerve predominates, indicates the importance of the autonomic nervous system;
- excessive physical activity;
- hypercholesterolemia in the blood;
- the use of drugs from the group of α2-adrenergic agonists in the treatment of patients (Gemiton, Clonidine, Catapresan, Clonidine);
- hypertrophic type cardiomyopathy;
- congenital or acquired heart defects (including impaired structure of the conduction system);
- changes in the structure of connective tissue in systemic diseases.
Prevalence
Typically observed in athletes, cocaine users, hypertrophic obstructive cardiomyopathy, and ventricular septal defects. Prevalence varies from 3% to 24% of the general population.
Young people, especially those predisposed to vagotonia, men, African Americans, and athletes are subpopulations that have a higher prevalence.
J-point elevations >0.2 mV are associated with significant mortality from cardiac arrhythmia.
Types and criteria of premature ventricular repolarization
The main criteria for the ECG picture in diagnosing the syndrome are:
- Shift upward of the ST interval. Usually it does not have a strictly horizontal direction and smoothly passes into the ascending knee of the T wave. A sharp rise indicates the process of necrosis during a heart attack, severe dystrophy, digitalis intoxication, and pericarditis. Accelerated repolarization gives an increase in the interval by no more than 3 mm.
- Tall T wave with a wide base (to be distinguished from hyperkalemia, ischemia).
- “Notch” on the descending section of R.
ECG signs do not always include all elements of the syndrome
In functional diagnostics, it is customary to distinguish two variants of the syndrome:
- with the participation of other manifestations of heart pathology;
- without cardiac signs of damage.
According to the duration of manifestations, the syndrome can be:
- transient,
- permanent.
A. Skorobogaty’s classification provides for the connection of types of premature repolarization with chest leads on the ECG:
- pronounced signs in V1-V2;
- changes predominate in V4-V6;
- without any patterns in the leads.
Tests and diagnostics
The main changes are recorded precisely on the electrocardiogram. Some patients simultaneously experience clinical symptoms of cardiovascular diseases, but most often patients feel absolutely healthy and do not notice any changes.
Early ventricular reoplarization syndrome on ECG:
- elevation of the ST segment above the isoline;
- the convexity when raising the ST segment is directed downwards;
- an increase in the R wave with a parallel decrease in the S wave or its complete disappearance;
- point J is located above the isoline, at the level of the descending knee of the R wave;
- expansion of the QRS complex on the ECG;
- a “notch” is recorded on the descending limb of the R wave.
Who has similar disorders?
Premature repolarization is characterized by manifestation against the background of:
- overload of the left ventricle during hypertensive crisis, acute circulatory failure;
- ventricular extrasystole;
- supraventricular tachyarrhythmia;
- ventricular fibrillation;
- in adolescence with active puberty of the child;
- in children with problems of placental circulation during pregnancy, congenital malformations;
- in people involved in sports for a long time.
The absence of any influence of the syndrome of premature repolarization of a pregnant mother on the development of the fetus and the gestation process has been proven, unless other serious arrhythmias occur.
Symptoms
Clinical symptoms are observed only in the form of the disease that is accompanied by disturbances in the functioning of the cardiovascular system:
- loss of consciousness, fainting ;
- rhythm disturbances ( tachyarrhythmia , extrasystole , ventricular fibrillation );
- vagotonic, hyperamphotonic, tachycardial, dystrophic are formed under the influence of humoral factors on the hypothalamic-pituitary system;
- systolic and diastolic dysfunction of the heart caused by its hemodynamic disorders ( pulmonary edema , hypertensive crisis , shortness of breath , cardiogenic shock ).
Features of the syndrome in an athlete
Observations of athletes who train four hours a week or more showed the development of adaptive thickening of the wall of the left ventricle and the predominance of vagal influence. These changes are considered normal in sports medicine and do not require treatment.
80% of trained people have a heart rate of up to 60 per minute (bradycardia).
Early repolarization syndrome is determined, according to various sources, in 35–90% of athletes
Sudden cardiac arrest associated with early repolarization
METHODS. We reviewed data from 206 patients at 22 centers who were resuscitated from cardiac arrest due to idiopathic ventricular fibrillation and assessed the prevalence of electrocardiographic early repolarization. The latter was defined as an increase in the QRS-ST junction of at least 0.1 mV from baseline in the inferior or lateral lead, manifested as a QRS wander or notch. The control group included 412 patients without heart disease who were matched for age, sex, race, and physical activity level. Follow-up data, which included implantable defibrillator monitoring results, were obtained for all patients.
RESULTS. Early repolarization was more common in subjects with idiopathic ventricular fibrillation than in control subjects (31% vs. 5%, p < 0.001). Among study subjects, those with early repolarization were more likely to be male and have a history of syncope (fainting) or sudden cardiac arrest during sleep than patients without early repolarization. In eight subjects, the origin of ectopia, which initiated ventricular arrhythmias, was located in areas corresponding to the localization of repolarization anomalies. During a mean (±SD) follow-up of 61±50 months, defibrillator monitoring showed a higher rate of recurrent ventricular fibrillation in patients with repolarization abnormality than in patients without such pathology (odds ratio, 2.1, 95% confidence interval, 1. 2 to 3.5, P = 0.008).
CONCLUSIONS. Among patients with a history of idiopathic ventricular fibrillation, there is an increased prevalence of early repolarization.
Sudden cardiac arrest remains . A major public health problem that accounts for approximately 350,000 deaths annually in the United States. Despite advances in emergency medical care, only 3-10% of patients who experience cardiac arrest outside of hospital are successfully resuscitated. Most of these sudden cardiac arrests are caused by ventricular tachyarrhythmias, which occur in 6% to 14% of cases in individuals without structural heart disease. Some of the latter cases are associated with well-recognized electrocardiographic abnormalities that affect ventricular repolarization (eg, long or short QT intervals or Brugada syndrome), while other cases with no signs during sinus rhythm are described as idiopathic ventricular fibrillation. Early repolarization is a common electrocardiographic finding that affects 1 to 5% of people. Although this condition is generally considered benign, its potential arrhythmogenicity has been suggested by experimental studies. However, there is no supporting clinical evidence. We conducted a case-control study of 206 patients with idiopathic ventricular fibrillation to assess the prevalence of early repolarization and assess its potential association with any observed arrhythmias and subsequent outcome monitored by implantable defibrillators.
Methodology.
POPULATION STUDY. Cases of the disease in people under the age of 60 were recorded in 22 territorial centers dealing with arrhythmias. All patients diagnosed with idiopathic ventricular fibrillation in this age group were selected from databases of patients who had received an implantable defibrillator; All patients aged 60 years or older were excluded to minimize the risk of subclinical structural heart disease. Verbal informed consent was obtained from all enrolled patients.
We assessed baseline electrocardiograms for the presence of early repolarization, which was defined as an increase in the QRS-ST junction (J point) in at least two leads during defibrillator implantation. The J-point height amplitude had to be at least 1 mm (0.1 mV) above baseline, either as a QRS blur (a smooth transition from the QRS segment to the ST segment) or a notch (a positive J deflection inscribed on the S wave ) in the inferior lead (II, III and aVF), lateral lead (I, aVL and V4 to V6) or both. Anterior chest leads (V1 to V3) were excluded from the analysis to avoid inclusion of patients with right ventricular dysplasia or Brugada syndrome.
Based on published guidelines, patients were classified as having idiopathic ventricular fibrillation if they had no structural heart disease as demonstrated by normal echocardiographic biventricular dimensions and function, no evidence of ischemic coronary artery disease on coronary angiography or stress testing, and no evidence of any repolarization anomalies. Patients were excluded if they had a heart rate-corrected QT interval (QTc) of less than 340 ms (short QT interval) or more than 440 ms (long QT interval) at baseline and before the arrhythmia. Patients with Brugada syndrome, defined by right branch block and ST segment elevation (>0.2 mV) in precordial leads V1-V3 without intervention or after sodium channel blocker (antiarrhythmic) infusion, were also excluded. In addition, patients with catecholaminergic arrhythmias, defined as arrhythmias during catecholamine infusion or exercise testing, were excluded.
We assessed the prevalence and amplitude of early repolarization in a control group of 412 subjects. This group was composed of health care professionals with normal echocardiographic biventricular dimensions and function and no history of syncope (fainting). The following factors were used for matching (age, gender, race, and physical activity level).
Data collection.
We collected the following clinical data: history of syncope, sudden cardiac arrest, family history of sudden death (age <60 years), physical activity level (>10 hours or ≤10 hours of activity per week), averaged by electrocardiographic signals (both standard amplification and high amplification) and the results of pharmacological testing and invasive electrophysiological testing. Electrocardiographic parameters were measured using automated online software and verified manually. The QTc interval was calculated after heart rate correction using the Bazett formula.
ELECTROPHYSIOLOGICAL STUDY. We performed electrophysiological studies using multielectrode catheters inserted percutaneously through the femoral vessels. Programmed ventricular pacing was performed using a maximum of two or three ventricular extrastimulations from two separate ventricular sites. Ventricular fibrillation was considered inducible if it lasted more than 30 seconds or required electrical cardioversion. No patient had inducible monomorphic ventricular tachycardia.
For subjects with recurrent ventricular fibrillation despite administration of antiarrhythmic drugs, catheter ablation targeting the initiating ventricular ectopy was performed as previously described. Such ectopia was localized by mapping the earliest electrical activity, either Purkinje or myocardial, relative to the onset of the QRS complex. Ablation was performed using radiofrequency energy.
THERAPY AND FOLLOW-UP. All patients with episodes received an implantable defibrillator, which provided accurate information about the recurrence of ventricular fibrillation. Patients were followed regularly every 6–12 months for clinical examination and device testing or, as needed, in the event of symptoms or device battery depletion. In subjects with recurrent arrhythmias, the choice of antiarrhythmic drugs was made by the treating physicians.
STATISTICAL ANALYSIS. Continuous variables were reported as mean ± SD or median (with 25th and 75th percentiles), as appropriate. Comparisons between the two groups were performed with the Student's t test or nonparametric Wilcoxon test, as appropriate, and with the Student t test for paired data. Categorical variables were compared with Fisher's exact test. The prevalence of early repolarization was compared between study subjects and controls using logistic regression analysis (reported as odds ratios with 95% confidence intervals) and adjusted for matching variables. The number of recurrences of ventricular fibrillation was compared using the Wilcokinson test, and the recurrence rate was estimated using actuarial curves. Hazard ratios from Cox proportional hazard models were used to estimate the relative risk associated with early repolarization. All tests were two-sided, and a P value of less than 0.05 was considered statistically significant.
RESULTS.
EARLY REPOLARIZATION.
In the group of patients with idiopathic ventricular fibrillation, there were 123 men and 83 women with a mean age of 36 ± 11 years. The control group included 412 subjects who were matched for age (36 ± 12 years), sex (270 men and 142 women), race (380 whites, 27 Asians, and 5 blacks), and physical activity (44 subjects engaged in more than 10 hours of activity per week ).
Early repolarization occurred in 64 patients (31%) compared with 21 controls (5%, P < 0.001) and was greater in magnitude in study subjects than in control subjects (J-point Height 2.0 ± 0.9 mm vs. 1.2 ± 0.4 mm, P < 0.001). After adjusting for age, sex, race, and physical activity level, the odds ratio for the presence of early repolarization in study subjects compared with control subjects was 10.9 (95% confidence interval [CI], 6.3–18.9).
Cases with early repolarization were more likely to be male, had a history of unexplained syncope or sudden cardiac arrest during sleep, and had a shorter QTc interval than those without early repolarization.
At the initial stage, early repolarization was present in the anterior leads in 28 subjects, in the lateral leads in 6 subjects, and in the inferior and basal leads in 30 patients. This pattern was considered a repolarization rather than a late depolarization because of its slower recording, spontaneous fluctuation in morphologic pattern or amplitude before sustained QRS complexes, and amplitude varying concurrently with the ST segment. The absence of late potentials on high-amplification electrocardiography further supported the repolarization pattern. This pattern occurred in isolation or was accompanied by negative T-wave elevation or discrete ST-segment elevation (horizontal or upward curvature). Electrocardiograms that were obtained several weeks before sudden cardiac arrest were available for 22 subjects and showed a pattern of early repolarization (as described above).
Electrocardiography was performed during the arrhythmic period (including incidence of ventricular ectopy and episodes of ventricular fibrillation) in 18 subjects, all studies showing a consistent increase in early repolarization amplitude compared with baseline. J-point amplitude increased from 2.6 ± 1 mm to 4.1 ± 2 mm (P < 0.001). In most cases, ectopia had a positive QRS morphological pattern in leads V1 to V2, indicating origin from the left ventricle and a short interaction interval initiating ventricular fibrillation (mean, 326 ± 41 ms, range 260 to 400).
Exercise testing or isoproterenol infusion consistently reduced or eliminated early repolarization. Isoproterenol administered to two subjects during repeated episodes of ventricular fibrillation eliminated all arrhythmias when the sinus node heart rate was increased by more than 120 beats per minute. In contrast, beta blockers increased repolarization abnormalities. Their ineffectiveness has led to attempts at catheter ablation of ventricular premature contractions, which resulted in ventricular fibrillation in some subjects.
CORRECTION OF ECTOTIA IN EARLY REPOLLARIZATION. Mapping was performed in eight patients. In two cases, mapping of both ventricles showed no findings during ventricular depolarization that coincided with wide terminal QRS abnormalities, confirming that the latter was associated with repolarization. A total of 26 ectopic patterns were mapped to either ventricular myocardium (16 patterns) or Purkinje tissue (10 patterns). In six patients with early repolarization recorded only in the lower parts, the entire ectopia arose from the lower wall of the ventricle. In two patients with widespread early repolarization, which was recorded by both low and lateral lines, the ectopia arose from multiple regions. Catheter ablation eliminated all ectopia in five subjects and did not eliminate the condition in three subjects.
RELATIONSHIP OF SUBJECTS. Table 2 summarizes results over a mean period of 61 ± 50 months (median, 51 months; interquartile range, 19 to 90) after the initial event, with no subjects losing control. Arrhythmic relapses were more frequent in subjects with early repolarization than in subjects without such repolarization (41% vs. 23%). The hazard ratio for relapse was 2.1 (95% CI, 1.2 to 3.5; P = 0.008), even after adjustment for sex. The three patients with the highest J-point level (>5 mm) had more than 50 episodes of ventricular fibrillation, resulting in death in one case. Quinidine was prescribed to four patients with multiple episodes, which reduced repolarization abnormalities and eliminated recurrent arrhythmias.
DISCUSSION. Sudden cardiac arrest from arrhythmia can occur in individuals who do not have structural heart disease or obvious electrocardiographic abnormalities during sinus rhythm. In our study, such study subjects had a significantly higher prevalence of early repolarization than control subjects, whose prevalence was similar to that of healthy subjects in previously reported studies. In nearly a third of the patients, electrocardiograms obtained before cardiac arrest were available and showed early repolarization, which indicated that this abnormality could not be the result of trauma following sudden cardiac arrest, resuscitation, or the drugs used for resuscitation.
It is unlikely that this anomaly is more common among survivors of cardiac patients than among non-survivors, since the single most important factor determining successful resuscitation is access to rapid defibrillation. This electrocardiographic pattern has also been associated with an increased rate of recurrent ventricular arrhythmias during defibrillator monitoring.
Our results show an association between early repolarization and sudden cardiac arrest, a finding that contradicts the seemingly benign nature of this common phenomenon. First, this finding may be related to the definition of early repolarization, since we specifically included abnormalities in the inferolateral leads, whereas the broad traditional definition of early repolarization included electrocardiographic patterns of varying amplitude, configuration, and extent, most often in the right chest leads. Second, few of the study subjects in our study were from subgroups that have a high prevalence of early repolarization (eg, athletes and blacks), suggesting that cofactors influence the association with sudden cardiac arrest. Third, the beneficial nature of early repolarization is challenged by experimental evidence suggesting that a form of transmural electrical heterogeneity can be dramatically enhanced under certain conditions (use of specific drugs and varying levels of autonomic tone and electrolytes), leading to malignant arrhythmias. Potential arrhythmogenicity thus depends on defective modulation of repolarization, which corresponds to the dynamic changes temporally associated with the arrhythmias that we observed in our case.
The relationship between this electrocardiographic pattern and malignant arrhythmias is supported by increased repolarization before the onset of arrhythmia in study subjects and the occurrence of trigger contractions in the region of early repolarization. Quinidine, which has been shown to restore transmural electrical homogeneity and abolish arrhythmic activity in this condition, reduced the electrocardiographic pattern and eliminated recurrent arrhythmias in four subjects.
Finally, although to our knowledge no multicenter study has examined the association between early repolarization and sudden cardiac arrest, anecdotal reports (mostly from Southeast Asia) have described patients in whom sudden cardiac arrest was associated with abnormal J waves. A repolarization abnormality that is detected in the anterolateral region may be a marker of underlying electrical vulnerability that increases the risk of fatal arrhythmias in the conditions that need to be investigated. These conditions include the presence of genetic defects associated with cardiac ion channels, as evidenced by the fact that 10 of our patients had a family history of sudden cardiac arrest.
These results are potentially important for the evaluation of patients with syncope (fainting) or a family history of sudden death. Arrhythmias associated with repolarization abnormalities may be responsible for a proportion of unexplained deaths, predominantly in young men, as previously reported. Such arrhythmias may also be responsible for some undiagnosed causes of syncope, which have been reported to increase the risk of premature death.
The results of our study, which require confirmation by other researchers, have several limitations. Although the cohort included subjects with well-defined common features, data collection was uneven among centers. In our study population, we did not have subjects with structural heart disease and did not have many athletes or blacks, so the results may not apply to these subgroups. Most importantly, although our results suggest that early repolarization is a marker of malignant arrhythmia disorder, studies predict a favorable course for most of these patients. Further research is needed to identify factors that modulate underlying arrhythmogenicity and predict which patients are at risk.
In conclusion, this multicenter study showed a higher than expected prevalence of early repolarization in patients younger than 60 years of age who had idiopathic ventricular fibrillation that caused syncope and sudden cardiac arrest.
How to identify the syndrome?
Diagnosis is based on an ECG examination. For unstable symptoms, Holter monitoring is recommended throughout the day.
Drug tests can provoke or eliminate typical ECG changes. They are carried out only in a hospital under the supervision of the attending physician.
The most acceptable test for a clinic setting is physical activity. It is prescribed to identify hidden pathology and the degree of adaptability of the heart. Squats, treadmills, and walking on stairs are used.
Such a test is considered mandatory when deciding on military service, joining the police, special forces, or when applying for a medical certificate for military educational institutions.
Isolated premature repolarization is not considered a contraindication in these cases. But the accompanying changes may be regarded by the military medical commission as an inability to work in a difficult sector or serve in special forces.
A complete examination is necessary to exclude cardiac pathology. Appointed:
- biochemical tests (lipoproteins, total cholesterol, creatine phosphokinase, lactate dehydrogenase);
- Ultrasound of the heart or Doppler sonography.
Differential diagnosis necessarily requires the exclusion of signs of hyperkalemia, pericarditis, dysplasia in the right ventricle, and ischemia. In rare cases, coronary angiography is necessary for clarification.
Does the syndrome need to be treated?
Uncomplicated early repolarization syndrome requires the following:
- refusal of increased physical activity;
- changing the diet to reduce the proportion of animal fats and increase fresh vegetables and fruits rich in potassium, magnesium, and vitamins;
- It is necessary to maintain a healthy routine, get enough sleep and avoid stress.
It is not recommended to burden your child with additional activities
Drug therapy includes, if necessary:
- in the presence of cardiac pathology, specific drugs (coronary lytics, antihypertensive drugs, β-blockers);
- antiarrhythmic drugs that slow down repolarization if accompanied by rhythm disturbances;
- some doctors prescribe drugs that increase the energy content in heart cells (Carnitine, Kudesan, Neurovitan), you should pay attention to the fact that these drugs do not have a clear evidence base confirming their effectiveness;
- B vitamins are recommended as coenzymes in the processes of restoring the balance of electrical activity and impulse transmission.
Surgery is used only for severe cases of arrhythmias contributing to heart failure.
By inserting a catheter into the right atrium, additional pathways of impulse propagation are “cut” by radiofrequency ablation.
If there are frequent attacks of fibrillation, the patient may be offered a defibrillator-cardioverter to eliminate life-threatening attacks.
Treatment
The ER pattern is a benign incidental finding, without any specific signs or symptoms. There is no risk stratification strategy for asymptomatic patients with the ER pattern. It is generally accepted that these people do not require special investigations or therapeutic interventions.
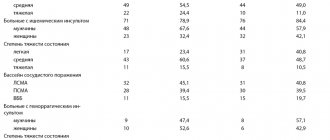
Among surviving patients with SCD, the relapse rate is 22-37% within two to four years. Because there is no structural heart disease, they have an excellent prognosis for long-term survival with treatment. The best treatment strategy is an implantable pacemaker (ICD). Recommendations for therapeutic interventions are given in Table 3.
Table 3 Therapy
| Expert recommendations for early repolarization therapy | ||
| Class I | 1 | ICD implantation is recommended for people diagnosed with ER syndrome who have experienced cardiac arrest |
| Class IIa | 2 | Isoproterenol infusion is useful in suppressing electrical storms |
| 3 | Quinidine in addition to ICD is useful for secondary prevention of VF | |
| Class IIb | 4 | ICD implantation may be considered for symptomatic family members of patients with a history of ER syndrome in the presence of elevation >1 mm. 2 inferior, lateral leads |
| 5 | ICD implantation may be considered in asymptomatic individuals who demonstrate a high-risk ECG (high amplitude J-wave, horizontal, descending) in the presence of a family history of juvenile unexplained sudden death with or without a pathogenic mutation | |
| Class III | 6 | ICD implantation is not recommended for asymptomatic cases and isolated ECG patterns. |
ER: early repolarization; ICD: implantable cardioverter defibrillator.
People with VF repolarization had a higher relapse rate over five years of follow-up than those with VF without ER (43 vs. 23%,). In terms of long-term therapy, relapses have been shown to be effectively suppressed by quinidine therapy.
Promising results were shown by a study by Gurabi et al, which demonstrated that in addition to quinidine cilostazol, milrinone suppressed hypothermia-induced VT/VF.
Between the two ends of the spectrum there is a gray area where there are no clear guidelines. Examples include patients with syncope who may have a “malignant” ER pattern or a significant family history of sudden cardiac death.
Current guidelines suggest that ICD implantation is considered for individuals at high risk for unexplained syncope.
What does the forecast say?
Modern cardiology is aimed at preventing all pathologies that affect fatal complications (sudden cardiac arrest, fibrillation). Therefore, it is recommended to observe patients with impaired repolarization, compare ECG dynamics, and look for hidden signs of other diseases.
Athletes must be examined at physical education clinics. Check before and after intense training and competitions.
There are no clear indications of the transition of the syndrome to a typical pathology. The risk of death is much greater with alcoholism, smoking, and overeating fatty foods. However, if a doctor prescribes a comprehensive examination, it should be completed to exclude possible hidden abnormalities. This will help avoid problems in the future.
Clinical signs
The clinical picture is divided into two main groups. The first includes those that exhibit recognized symptoms. For example, people at high risk of fainting who have survived cardiac arrest. This group very rarely has recurrent cardiac events. The Haissaguerre study showed a 41% recurrence rate of arrhythmia at 51 months.
The second, most common group is asymptomatic people. They have an ER pattern on their ECG. This group is less likely to have adverse cardiac events. The challenge is to distinguish people at risk for sudden cardiac death from those who may have a benign course of the disease.