Sore throat or acute tonsillitis is an inflammatory process that develops on the palatine tonsils, caused by an infectious infection. The main complaint with a sore throat is a sore throat. It occurs due to inflammation of the tissue of the pharynx, which leads to local swelling, which in turn compresses and irritates the nerve endings of the throat. A sore throat can also be a manifestation of acute pharyngitis and laryngitis. The difference between acute tonsillitis and these two diseases is that different tissues of the pharynx are involved in the process. In acute pharyngitis, the inflammatory process is observed in the area of the posterior wall of the pharynx. Laryngitis affects the tissues in the vocal cords area. And with tonsillitis - palatine tonsils. Only a doctor can diagnose the disease and select the correct treatment regimen, so if you experience symptoms of a sore throat, make an appointment with a pediatrician at our private medical clinic “Doctor Anna”.
Types of sore throat
There is a classification of angina according to external manifestations and forms of progression, among which the most common can be identified:
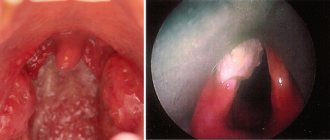
- Catarrhal. The tonsils are enlarged, red, and in places covered with mucus and pus. The tongue is covered with a white coating.
- Lacunar tonsillitis. It has similar manifestations to follicular, but is more severe. Both purulent spots and purulent plaque appear on the tonsils.
- Follicular. The symptoms are similar to the catarrhal form, but more pronounced. Yellowish-white purulent dots appear on the tonsils - this is what inflamed follicles look like.
- Phlegmonous. Purulent melting of the tonsils, which occurs with a weakened immune system, massive infection with microbes, or with improper treatment of milder forms of tonsillitis. Most often it is one-sided.
- Herpes sore throat. On the tonsils there are rashes in the form of blisters, redness, acute pain and fever. Develops when infected with the Coxsackie virus.
Follicular and lacunar forms refer to purulent tonsillitis. Pus accumulates in the tonsils, which is released when pressed.
Causes of sore throat
The root cause of this disease is viruses and bacteria. The most common of them are beta-hemolytic streptococcus and staphylococcus. They can enter the body from the environment or from sources of chronic infection within the body itself. The immune system of a healthy person should suppress pathogenic microorganisms, but there are provoking factors for the development of sore throat:
- smoking;
- deficiency of vitamins and balanced nutrition;
- hypothermia;
- throat trauma;
- the presence of other inflammatory processes.
Etiology and pathogenesis
Among the various possible microbial pathogens of sore throat (cocci, bacilli, viruses, spirochetes, fungi, etc.), in most cases the main etiological role belongs to group A b-hemolytic streptococcus (GABHS). This pathogen, according to a number of authors, is detected in sore throat in more than 80%, according to other sources - in 50–70% of cases. Much less frequently, acute tonsillitis is caused by group C and G streptococci, Arcanobacterium haemolyticum, Neisseria gonorrhoeae, Corynebacterium diphtheria (diphtheria), anaerobes and spirochetes (Simanovsky-Plaut-Vincent angina), and extremely rarely by mycoplasma and chlamydia. The cause of acute viral tonsillitis can be adenovirus, rhinovirus, coronavirus, influenza and parainfluenza viruses, Epstein-Barr virus, Coxsackie A virus and others. Penetration of an exogenous pathogen into the mucous membrane of the tonsils can occur through airborne droplets and alimentary routes, as well as through direct contact. In the occurrence of an endogenous pathogen, great importance is attached to chronic tonsillitis. As noted by B.S. Preob¬ra¬zhensky (1954), the frequency of sore throats in chronic tonsillitis is explained by the fact that in this disease there are usually up to 75% of cases of carriage of GABHS, vegetating in the crypts of the palatine tonsils.
In the pathogenesis of tonsillitis, a certain role can be played by a decrease in the body’s overall reactivity to cold, sharp seasonal fluctuations in environmental conditions (temperature, humidity, nutrition, intake of vitamins, etc.), trauma to the tonsils, constitutional predisposition to tonsillitis (for example, in children with lymphatic – hyperplastic constitution), the state of the central and autonomic nervous system. Factors predisposing to angina are chronic inflammatory processes in the mouth, nose and paranasal sinuses. The development of sore throat occurs according to the type of allergic-hyperergic reaction, which is a prerequisite for complications such as rheumatism, acute diffuse nephritis and other diseases of an infectious-allergic nature and associated with the GABHS antigen.
Sore throat in children
Children, unlike adults, have a particularly difficult time with sore throat, which is accompanied by severe pain, high fever up to 39-40 degrees, difficulty swallowing and difficulty breathing. A child can become infected at school or kindergarten. The most dangerous form of the disease occurs in children under one year of age, so when it is diagnosed, the child is usually hospitalized. The disease begins with an increase in temperature, acute pain in the throat and the feeling of a lump when swallowing. Parents can palpate enlarged submandibular lymph nodes. Swelling of the airways causes difficulty breathing, which may cause the child to snore while sleeping. If a child has all the signs of a sore throat, self-medicating and using folk remedies is extremely dangerous, so you should definitely make an appointment with a pediatrician. For a speedy recovery, children should not only take all necessary medications and observe only bed rest, but also adhere to a special diet. It consists of eating a large amount of pureed and baked fruits and vegetables, soups, broths and a sufficient amount of liquid - fruit drink, tea, juice. It is recommended to exclude various seasonings and hot sauces, very hot foods, salty and fried foods.
Actions for sore throat
If you notice the first symptoms of the disease, you should consult a doctor. Under no circumstances should you self-medicate or try to overcome the disease with folk remedies. Sore throat is a serious disease that is dangerous to joke with.
If a sore throat is not treated or acted incorrectly, a number of complications can occur:
- chronic tonsillitis - in this case you will remain with this disease for life;
- laryngitis or bronchitis;
- abscess;
- rheumatism of the heart or joints;
- glomerulonephritis;
- pyelonephritis.
For a sore throat, a specialist prescribes antibiotics depending on the clinical picture and individual characteristics of the patient. Gargling is also prescribed every hour to remove suppuration and inflammation. To do this, use herbal decoctions, salt with soda, furatsilin, chlorhexidine. Do not eat or drink for half an hour after rinsing.
In addition to rinsing, the tonsils are irrigated with antimicrobial agents. If the temperature rises above 38 degrees, antipyretics are taken. Children are recommended to use wraps to relieve fever.
Antihistamines will help relieve swelling, and special lozenges will reduce pain.
It is important to ensure you drink plenty of fluids. In this case, warm fruit drinks will be most useful.
Food during illness should be dietary, soft and warm, so as not to irritate a sore throat.
Sore throat in adults
It is worth remembering that this disease is infectious in nature. Therefore, if treatment takes place at home, it is necessary to use individual cutlery and try to have less contact with others. In severe cases of acute tonsillitis, it is possible to place the patient in a hospital under the supervision of doctors. Every adult with a high degree of probability has suffered from a sore throat at least once. But, if it occurs frequently, the palatine tonsils increase in size, become looser, deformed, and their protective function—participation in the formation of immunity—is disrupted to such an extent that they themselves become a constant source of infection. In the tonsils, even without an exacerbation of the disease, pus, mucus and food waste begin to accumulate, and purulent plugs form, creating bad breath. All these manifestations are symptoms of chronic tonsillitis. This disease is dangerous because an inflammatory process constantly occurs in the tonsils, leading to frequent exacerbations. In this case, there is the greatest likelihood of complications for internal organs. A chronic process in the palatine tonsils reduces immunity, weakening the body and making it more susceptible to various infections.
Causes of acute tonsillitis
A sore throat can be caused by a fungus or a virus, but most often the cause of the disease is bacteria. The most common variant is streptococcus. Quite often, sore throat is a complication of ARVI. In such situations, they usually talk about the addition of a bacterial infection.
Sore throat is transmitted by airborne droplets. Transmission of infection through household items is less common.
Most often, elderly people and children and people with weakened immune systems become infected. Why? Tonsils are organs that are part of the body's immune system. Their function is to protect the body from pathogenic bacteria. In fact, they are a kind of barrier that does not allow the “enemy” into the body. However, in cases with weakened immunity, the tonsils are not able to cope with the task and do not protect the body from pathogenic microflora. As a result, microorganisms attack the tonsils, causing them to become inflamed.
Sore throat can occur due to the following reasons:
- hypothermia, both of the throat and general;
- lack of vitamins;
- chronic tonsillitis is a sluggish inflammatory process in the tonsil area, which can result from untreated tonsillitis;
- poor air ecology - inhalation of polluted air in industries, etc.;
- foci of infection in the nasopharynx - caries, adenoids, sinusitis, etc.
Symptoms of a sore throat
There are a number of signs by which you can independently suspect the disease:
- sore throat when swallowing, may radiate to the ears;
- feeling of dry throat, sore throat;
- increased body temperature from slight to 39-40 degrees, impaired general condition, weakness, drowsiness, chills, headache;
- enlarged lymph nodes;
- changes in tonsils.
Even if the patient knows how to treat a sore throat, it is under no circumstances possible to squeeze out purulent plugs on your own, because with mechanical impact on the tonsil, it is possible to extract only a small fraction of the contents, the bulk remains inside, which sinks deeper under pressure, which is fraught with complications (abscess , edema, phlegmon of the neck, sepsis).
Publications in the media
Secondary tonsillitis is an acute inflammation of the components of the lymphatic pharyngeal ring (usually the palatine tonsils), caused by a systemic disease: infectious or hematological pathology.
SONGINS IN INFECTIOUS DISEASES
Sore throat with measles • Damage to the mucous membrane of the pharynx occurs in the prodromal period and the period of rashes • Belsky-Filatov-Koplik spots are found on the mucous membrane of the cheeks • Measles enanthema • Characteristic skin rash • Pharyngoscopic picture varies from catarrhal tonsillitis to a necrotic process.
Diphtheria sore throat (diphtheria of the throat) is the most common form of diphtheria.
• Clinical picture •• Acute onset •• General intoxication - headache, malaise, loss of appetite, adynamia, increased body temperature •• Pale skin •• Enlarged regional lymph nodes •• Severe sore throat, usually worsening on the 2nd day diseases.
• Pharyngoscopy •• Swelling of the palatine tonsils and arches, mild hyperemia with a cyanotic tint •• In the depths of the lacunae (island form) and/or on the surface of the tonsils (membranous form), plaque is found in the form of films of grayish-yellow or yellow-white color, plaque appears by the end of 2 days of illness. The films are thick, difficult to remove, leaving a bleeding surface, do not rub on a glass slide, and sink in water. After removing the film, new plaques form in its place •• Plaques on the tonsils persist after body temperature normalizes and symptoms of intoxication disappear (important for the retrospective diagnosis of untreated diphtheria and the prevention of complications - myocarditis, paresis of the soft palate, etc.).
• In cases of sore throat accompanied by the formation of plaque, it is necessary to first suspect diphtheria of the pharynx. Negative results of a bacteriological test for diphtheria are not considered sufficient grounds to cancel the clinical diagnosis of diphtheria.
Sore throat with scarlet fever • Clinical picture •• Inflammation of the mucous membrane of the pharynx from catarrhal to necrotic •• Characteristic is the appearance of scarlet fever enanthema already at the end of the prodromal period, i.e. before scarlet fever exanthema •• Typical appearance of the patient - “scarlet fever mask”: bright blush, pallor of the nasolabial triangle •• Regional lymph nodes are enlarged, painful • Pharyngoscopy •• Severe widespread hyperemia of the palatine tonsils and hard palate with distinct boundaries •• Swollen and hyperemic palatine a tongue that looks like a “crushed cranberry” •• The palatine tonsils are sharply enlarged, hyperemic, their changes correspond to follicular or catarrhal tonsillitis. Grayish-yellowish plaques appear on the tonsils, sometimes merging and covering the entire tonsil. The plaques are tightly fused to the surface of the tonsil, but do not rise above it.
Angina in tularemia occurs in its tonsillar-bubonic form • Clinical picture •• The first 2 days of changes in the tonsils are catarrhal in nature, from the 3rd day - membranous or necrotic •• Regional lymphadenitis - posterior cervical and submandibular lymph nodes increase in size within 1– 3 days, merge to form a tularemic bubo (the size of a nut to a goose egg) •• The conglomerate of lymph nodes is not fused with the surrounding tissues, is not painful, is prone to suppuration and the formation of fistulas •• The process is usually one-sided •• Healing is slow, from 2 –3 weeks to 3–6 months, with the formation of a keloid scar • Pharyngoscopy: the tonsils are enlarged in size, covered with a grayish-white coating. In the necrotic form, the plaque has a dirty gray color, is clearly demarcated and is located below the level of healthy tissue • Diagnosis: detection in smears taken from areas of necrosis and in the lymph nodes of Francisella tularensis.
Sore throat with typhoid fever • Clinical picture •• As an initial symptom of the disease, sore throat occurs in 50–70% of cases •• In the prodromal period - a rise in body temperature •• Moderate pain in the throat •• Lymph nodes are enlarged on the affected side, painful on palpation • Pharyngoscopy : at the beginning of the disease there is a picture of catarrhal tonsillitis, then in the 2nd week a unilateral painless ulcerative-necrotic lesion of the tonsil may occur with the formation of small round ulcers with smooth red edges and a grayish bottom, spreading to the palatine arches. After 4 weeks, areas of granulation tissue appear, followed by epithelization.
Monocytic tonsillitis (angina with infectious mononucleosis) is an acute infectious disease characterized by monocytosis in the blood and typical changes in the pharynx • Etiology: primary infection with the Epstein-Barr virus in adolescence or older • Clinical picture •• Acute onset with chills, headache and a sharp rise in body temperature to 40 °C and above •• Sore throat •• Enlargement (usually symmetrical) and tenderness of the submandibular, cervical and occipital lymph nodes •• At the height of lymphadenitis, changes appear in the pharynx. In the initial stages, the changes are in the nature of catarrhal or follicular tonsillitis, later they resemble diphtheria tonsillitis (in two thirds of cases of monocytic tonsillitis, diphtheria is mistakenly diagnosed) •• Severe swelling of the mucous membrane of the pharynx and lymphadenoid ring occurs, incl. and nasopharyngeal tonsil, which leads to difficulty in nasal breathing, nasal sound, a feeling of stuffiness in the ears •• The liver is enlarged, protrudes from under the edge of the costal arch, may be slightly painful on palpation •• The spleen is enlarged, dense, painless •• Plaques on the tonsils persist for a long time (up to several weeks and even months), sometimes recur • Laboratory signs - leukocytosis 10–20´109/l or more with a predominance of atypical mononuclear cells (up to 60–80%).
ANGINA IN DISEASES OF THE BLOOD SYSTEM
Sore throat with agranulocytosis • Clinical picture •• Increased body temperature to 39–40 °C with chills, intoxication, severe general condition •• Severe sore throat •• Drooling •• Putrid breath •• At the height of the disease, hemorrhagic syndrome develops: bleeding gums, nosebleeds, skin hemorrhages •• Stomatitis, gastrointestinal lesions • Pharyngoscopy. Changes in the pharynx are often localized on the tonsils, are ulcerative-necrotic in nature and spread to the mucous membrane of the pharynx, gums, and larynx. In the blood, the number of all forms of leukocytes (up to hundreds of cells in 1 μl), platelets and reticulocytes is sharply reduced. The number of plasma cells is increased.
Sore throat in leukemia • Clinical picture - signs of sore throat that appear on the 3-5th day of acute or exacerbation of chronic leukemia • Pharyngoscopy. Changes in the tonsils first correspond to catarrhal tonsillitis, later hemorrhagic, ulcerative-necrotic or gangrenous lesions occur. Necrosis spreads to the mucous membrane of the mouth, gums and pharynx. The plaque formed on the surface of necrotic areas has a dirty gray or brown color; when it is rejected, a bleeding, eroded surface is exposed. Regional lymph nodes are enlarged.
TREATMENT • Sore throats due to infectious diseases - hospitalization in an infectious diseases hospital. Etiotropic, pathogenetic and symptomatic therapy. Therapeutic and disinfectant rinses • For diseases of the blood system, treatment is carried out in a therapeutic or specialized hematology department.
ICD-10 • J03.8 Acute tonsillitis caused by other specified pathogens
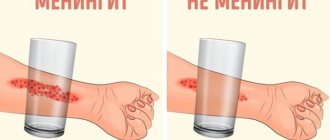
Complications
It is necessary to take angina very seriously, since this disease can cause serious complications on the heart and joints in the form of rheumatism, the kidneys can be affected and glomerulonephritis occurs. If you ignore the problem, sore throat may develop into a chronic form, which is called chronic tonsillitis. Lack of timely treatment can lead to abscess of the retropharyngeal space, sinusitis and sinusitis, and otitis media. Purulent inflammation of the neck and inflammation of the mediastinal organs are very dangerous conditions, often resulting in death. Also characteristic are autoimmune lesions of the heart and kidneys, meningitis, sepsis, and rheumatoid arthritis.
Diagnostics
You can independently suspect a disease in yourself or a child, first of all, by a sore throat and painful swallowing. Often the causes of pain are a cold or an acute respiratory viral infection, which lead to pharyngitis. If the pain is acute, this is a manifestation of a sore throat, but only a doctor can say for sure. There are different criteria for making a diagnosis. One of them is anapestic or collection of data, the causes of the disease, possible contacts with infected people, the presence of throat diseases in relatives. Next, a visual examination is carried out, during which the doctor evaluates the pharynx, tonsils, and performs pharyngoscopy. In order to identify the disease, the doctor takes swabs from the throat to determine the type of bacteria, as well as to determine sensitivity to various antibiotics. 2 hours before taking a smear, it is prohibited to consume food and various drinks. In addition, a general blood test, urine test and an electrocardiogram are performed to monitor treatment and monitor sudden complications. If leukocytosis and a neutrophilic shift are detected in the blood, this indicates a bacterial origin of the disease, and if there is a higher level of monocytes and eosinophils, we can speak of a viral infection.
Treatment of sore throats
Treatment of vulgar tonsillitis.
The rational treatment of sore throats is based on adherence to a certain gentle regimen, local and general therapy. Bed rest is mandatory in the first days of the disease, and then at home without physical activity. Prescribe a non-irritating, soft, nutritious diet, mainly vegetable and dairy, vitamins, and drinking plenty of fluids is beneficial.
Patients with angina, regardless of the severity of the condition and the period of the disease (even after the fever subsides), require antibacterial treatment to prevent the subsequent development of the described metatonsillar diseases.
GABHS are highly sensitive to penicillins and cephalosporins. β-lactams remain the only class of antibiotics to which GABHS has not developed resistance. The main problem is resistance to macrolides, which in Russia is 13–17%. At the same time, the M-resistance phenotype, characterized by resistance to macrolides and sensitivity to lincosamides (lincomycin and clindamycin), has become widespread. Resistance to tetracyclines and sulfonamides of GABHS in Russia exceeds 60%. In addition, tetracyclines, sulfonamides, co-trimoxazole do not provide eradication of the pathogen, and therefore they should not be used for the treatment of acute streptococcal tonsillitis caused even by strains sensitive to them in vitro.
Given the high sensitivity of GABHS to b-lactams, the first-line (drug of choice) for the treatment of acute streptococcal tonsillitis is penicillin (phenoxymethylpenicillin). More reliable, due to the possible resistance of the pathogen, is the use of amoxicillin clavulanate and sulbactam. Oral cephalosporins are rarely used. In patients allergic to b-lactams, macrolides or lincosamides should be used. Recommended medications, doses and dosage regimens are presented below.
Antibacterial therapy for acute streptococcal tonsillitis
Penicillins
- amoxicillin 750 mg in 3 doses 10
- amoxicillin/clavulanate 625 mg in 3 divided doses 10
- amoxicillin/sulbactam
Cephalosporins
- Cefadroxil 30 mg/kg in 1 dose 10
Macrolides (prescribed
for β-lactam intolerance)
- azithromycin 12 mg/kg in 1 dose 5
- Clarithromycin 15 mg/kg in 2 divided doses 10
- midecamycin 50 mg/kg in 2 divided doses 10
- roxithromycin 5 mg/kg in 2 divided doses 10
- spiramycin 3 million units in 2 doses 10
Lincosamides (prescribed
with intolerance to β-lactams and macrolides)
- lincomycin 30 mg/kg in 3 doses 10
- clindamycin 20 mg/kg in 3 divided doses 10
In severe cases of the disease, the patient is treated in an infectious diseases hospital. Here it is rational to use parenteral administration of an antibiotic. To prevent candidiasis on an individual basis, it is necessary to prescribe antifungal drugs. It is also advisable to prescribe a hyposensitizing drug (diphenhydramine, chloropyramine, mebhydrolin, loratadine, etc.).
In addition to general therapy, rinsing (slightly warm) with a solution of furacillin, miramistin, calendula tincture, and chamomile decoction is prescribed locally; apply a warm compress to the submandibular area. During febrile periods, drinking plenty of fluids is recommended.
Antipyretics (paracetamol-containing: paracetamol, ketaprofen, ibuprofen, etc.) are indicated at a body temperature of 38°C and above.
In the acute period of the disease and in the first days of normal body temperature, bed rest is necessary, then semi-bed rest and home rest (until the 7th day of normal body temperature). At this time, taking multivitamins is indicated.
Health indicators after a sore throat are normal body temperature for 5 days, absence of sore throat and pain on palpation of the maxillary lymph nodes, normal blood tests, urine tests and electrocardiogram.
- Atypical tonsillitis should first of all include Simanovsky-Versan tonsillitis (ulcerative-necrotic), as well as tonsillitis that occurs with systemic blood diseases and leukemia, herpetic and fungal tonsillitis.
- Treatment of ulcerative-necrotic sore throat of Simanovsky-Vincent (symbiosis of the spindle-shaped rod (B. fusiformis) and spirochete (Spirochaeta buccalis) of the oral cavity) is carried out by an otolaryngologist and consists of lubricating the ulcerated mucous membrane of the pharynx with a 10% solution of novarsenol in glycerin , 2% solution of methylene blue, 1% solution of boric acid, 10% solution of copper sulfate. Gargling with a 0.1% solution of ethacridine lactate, 0.1% solution of potassium permanganate. In severe cases of the disease, amoxicillin clavulanate (625 mg x 3 times) and intravenous infusion of novarsenol (0.3–0.4 g at intervals of 1–2 days) are recommended.
- Treatment of patients suffering from secondary acute tonsillitis due to infectious diseases is carried out in an infectious diseases hospital. Etiotropic and pathogenetic therapy is used. Disinfecting rinses are used locally.
- Treatment of patients with secondary acute tonsillitis due to diseases of the blood system is carried out in a therapeutic or specialized hematology department according to the rules for the treatment of the underlying disease.
- Fungal tonsillitis (pharyngomycosis) occurs mainly in young children and is caused by yeast-like fungi of the genus Candida albicans in 95% and Leptotryx buccalis in 5%.
Treatment of mycotic tonsillitis should be comprehensive. It includes oral use of antifungal antibiotics for 10–14 days (levorin, nystatin, decalinium chloride, mycoheptin, amphoglucamine B, ketoconazole, fluconazole), ascorbic acid, antihistamines and B vitamins. Rinses and inhalations are prescribed locally. For inhalation use amphotericin B, sodium salt of levorin, fluconazole, for rinsing - an aqueous solution of 3% boric acid, gramicidin 1:10000, potassium permanganate 1:10000, 1% quinosol.
Treatment
Treatment of sore throat is the responsibility of a therapist; you should contact him at the first suspicion of this disease, and in no case should you self-medicate. Different types of sore throat require different approaches to treatment; there is no universal cure. Many unqualified doctors for any throat disease, even mild sore throat, prescribe antibiotics to the patient, despite the fact that frequent use of these drugs leads to resistance and causes great harm to the body.
If the process is chronic, doctors suggest solving the problem radically by removing the tonsils. However, these approaches are incorrect, since an experienced specialist must first examine the patient and select a competent treatment regimen for him, trying in every possible way to avoid surgical intervention. You should turn to antibiotics as a last resort and only as prescribed by a doctor, because their prolonged and frequent use leads to a decrease in immunity. Also, many throat diseases are caused not by bacteria, but by viruses, against which antibiotics are powerless. Tonsils or tonsils should be removed only as a last resort, when the inflammation is very severe and no other treatment methods help. After all, the tonsils are the body’s protective gates, protecting it from any infections. Also, immune cells are produced in the tonsils; without them, immunity decreases and, if they are removed, the chances of contracting a particular infection increase. After such an operation, you can get quite serious problems with the heart and kidneys, and various allergic diseases can develop. Instead, the doctor may prescribe the use of Iodinol. This drug has a low cost in pharmacies and is much more effective than many expensive medications. With its help, it is recommended to prepare a solution with which to gargle regularly. But “Iodinol” has contraindications due to the fact that it affects the thyroid gland, therefore it is not suitable for autoimmune thyroiditis, pregnant women and nursing mothers. In this case, you can use inexpensive antiseptics such as Chlorhexidine and Miramistin. To treat tonsillitis, they also use a relatively inexpensive and very effective device for home use - a quartz ultraviolet irradiator with special throat attachments.
An important contribution to treatment is increasing immunity and drinking enough fluids. It is recommended to remove sweets and sugary, carbonated drinks from the diet, as sugar is a breeding ground for the development of microorganisms. In case of chronic illness, you should check the health of your teeth, because throat diseases often occur against the background of the fact that there is an infection in the oral cavity.
Hexoral against purulent sore throat
For acute tonsillitis, all drugs from the HEXORAL® line can be used.
You can treat the throat with a sore throat (acute tonsillitis) using HEXORAL® spray based on hexethidine. It allows you to evenly cover the surface of the mucous membrane of the tonsils and pharynx, which contributes to a more effective fight against infection8. A solution of HEXORAL® with hexethidine and a combination of essential oils7 may be suitable for gargling.
The use of hexetidine preparations is prescribed in clinical guidelines for the treatment of acute tonsillopharyngitis2. Hexetidine is an antiseptic that is active against most bacteria, herpes simplex viruses type 1, influenza A, PC virus that affects the respiratory tract, and fungi. In addition, it has a mild analgesic effect7.
Both HEXORAL® spray and solution are approved for use for local treatment of tonsillitis in adults and children over three years of age7,8.
Lozenges with a neutral mint flavor HEXORAL® TABS based on chlorhexidine and benzocaine have antiseptic properties and analgesic properties. They are approved for use in adults and children aged 4 years and older9.
For adults and children over 6 years old, HEXORAL® TABS CLASSIC is available with the flavors of orange, black currant, lemon and honey. It is based on a combination of the antiseptics amylmetacresol and dichlorobenzyl alcohol, which help in the fight against tonsillitis pathogens10.
HEXORAL® TABS EXTRA may be suitable for children over 12 years of age and adults. In addition to the antiseptic component, it contains lidocaine, which can relieve even severe sore throat11.
The information in this article is for reference only and does not replace professional advice from a doctor. To make a diagnosis and prescribe treatment, consult a qualified specialist.
Up to contents
Literature
- Dergachev V. S. Angina. Clinic, diagnosis and treatment algorithm. Choice of local antibacterial therapy // Regular issues of “RMZh” / No. 18. – 2007. – P. 1350.
- Clinical recommendations Acute tonsillopharyngitis // National Medical Association of Otorhinolaryngologists / 2016.
- Kunelskaya N.L., Turovsky A.B., Kudryavtseva Yu.S. Sore throats: diagnosis and treatment // General Medicine / No. 3. – 2010. – P. 4-9.
- Krasnova E.I., Khokhlova N.I. Differential diagnosis and treatment tactics for acute tonsillitis (tonsillitis) at the present stage // Attending physician / No. 11. – 2022. – P. 58-63.
- Shcherbakova M. Yu., Belov B. S. A-streptococcal tonsillitis: modern aspects // Pediatrics / Volume 88. - No. 5. – 2009. – P. 127-135.
- Instructions for use of the drug HEXORAL® solution // Reg. number P N014010/02 //
- Instructions for use of the drug HEXORAL® aerosol // Reg. number P N014010/01 //
- Instructions for use of the drug HEXORAL® TABS // Reg. number LSR-002626/07 //
- Instructions for use of the drug HEXORAL® TABS CLASSIC // Reg. number P N015976/01 //
- Instructions for use of the drug HEXORAL® TABS EXTRA // Reg. number LSR-004122/09 //
Up to contents