Pharmacological properties of the drug Choline alfoscerate
Belongs to the group of neurometabolic stimulants and has a neuroprotective effect. Cholinomimetic with a predominant effect on choline receptors in the central nervous system. Excites cholinergic receptors, mainly central (has a cholinomimetic effect). The mechanism of action is based on the fact that when choline enters the body, alfoscerate is broken down by enzymes into choline and glycerophosphate: choline is involved in the biosynthesis of acetylcholine, one of the main mediators of nervous excitation; glycerophosphate is a precursor of phospholipids (phosphatidylcholine) in the neuron membrane. Stimulates cholinergic neurotransmission - improves the transmission of nerve impulses in cholinergic neurons, improves the plasticity of neuronal membranes and receptor function, activates cerebral blood flow, stimulates central nervous system metabolism and reticular formation. In patients with involutive or hereditary degenerative psychoorganic syndrome, it has a positive effect on cognitive and behavioral reactions, improves concentration, memorization and reproduction of information. Improves mood, helps eliminate emotional instability, irritability and apathy. Activates mental activity. In the acute period of traumatic brain injury in patients with preserved mechanisms of autoregulation of cerebral blood flow, choline alfoscerate causes an increase in the linear velocity of blood flow on the affected side, helps to normalize the spatiotemporal characteristics of spontaneous bioelectrical activity of the brain, regression of neurological symptoms and restoration of consciousness. When taken orally, an average of about 88% of the administered dose is absorbed. Easily penetrates the BBB, accumulates mainly in the brain (concentration in the brain reaches 45% of the level in the blood), lungs and liver. Elimination occurs primarily through the lungs in the form of carbon dioxide. Only 15% of the drug is excreted by the kidneys and intestines. Does not affect the reproductive cycle, does not have teratogenic or mutagenic effects.
Introduction
In recent decades, a large number of articles have appeared in the medical literature on pharmacotherapy methods to protect brain neurons from various factors of damage, including stroke, trauma, and inflammation [1]. In clinical practice, the most frequently used drugs are those that have a complex effect on the cerebrovascular unit, since pathology requires protection of not only neurons, but also astrocytes, oligodendrocytes, and microglia. The use of such drugs can increase the degree of adaptation of neurons to damage, increase their viability in unfavorable conditions and thereby ensure better recovery after the resumption of blood flow. This class of drugs is called “neuroprotectors” [2]. The list of pharmacological neuroprotectors is expanding every year, but the multicomponent nature of cerebral metabolic disorders, as well as the limitation of extrapolation of experimental data into clinical practice, lead to ambiguity of opinions about neuroprotective therapy [3], although this direction is one of the most promising. The mechanisms of cerebral ischemia are quite complex and include several key cascades of pathological reactions in the brain that develop at different points in time. For example, excitotoxicity occurs within minutes and peaks within hours as the first molecular mechanism of injury. This is followed by oxidative and nitrosative stress and inflammation, developing within a few hours and persisting for several days after ischemia. These processes work synergistically after cerebral ischemia, so the choice of first-line drug is always difficult. Because phospholipid molecules are an important constituent of cell membranes in all mammals, treatments aimed at protecting and restoring phospholipids are one of the most promising approaches in clinical neurology. Choline precursors are exogenous agents that are converted into choline in the body and provide support, restoration and synthesis of cell membrane phospholipids, as well as the neurotransmitter acetylcholine. Choline precursors include choline alfoscerate and citicoline. In the presence of similar properties, it is impossible to put an equal sign between them, since in citicoline the prevailing effect is associated with the effect on membranes, the effect on neurotransmission is somewhat less pronounced, and in choline alfoscerate the dominant effect is the effect on neurotransmission, with a weaker membrane-protective mechanism of action. An accurate understanding of the differences between these drugs is provided by an analysis of pharmacological features, mechanisms of action, and effectiveness for various nosologies from the perspective of evidence-based medicine.
Citicoline (cytidine 5'-diphosphocholine)
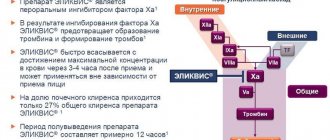
Citicoline (Ceraxon, Recognan) - cytidine 5'-diphosphocholine or CD-choline - is an endogenous nucleoside that participates as an intermediate in three main metabolic pathways, being an essential substance in the synthesis of phosphatidylcholine, the phospholipid synthesis pathway (Kennedy pathway) [4]. Citicoline is a natural metabolite of biochemical processes in the body; it is not a foreign chemical compound - a xenobiotic, like most drugs.
Consists of cytidine and choline linked by a diphosphate bridge. Cytidine is a nucleotide (component of RNA) formed when cytosine joins ribose via a β-N1 glycosidic bond. Choline is a substrate for the formation of acetylcholine, stimulates the activity of tyrosine hydroxylase and the secretion of dopamine [5].
The study of the pleiotropic effects of the drug deserves attention. It has been proven that the effect of Citicoline is more multifaceted than just its effect on various stages of the ischemic cascade [6]. It has been proven that a decrease in glutamate excitotoxicity leads to a decrease in the size of the ischemic focus [7]. The results of the use of Citicoline in clinical practice confirm the experimental data: the drug, by enhancing the inhibition of glutamate-induced apoptosis, stimulates a tendency to reduce the size of the lesion in patients with acute cerebrovascular accident (ACVA) [5]. Citicoline leads to the mobilization of endothelial progenitor cells from the bone marrow. An increase in the content of endothelial progenitor cells in peripheral blood is associated with a better functional outcome in patients who have suffered acute ischemic stroke [8].
Citicoline, being a source of choline, is involved in the synthesis of the neurotransmitter acetylcholine, stimulates the activity of tyrosine hydroxylase, increases the levels of norepinephrine (in the cortex and hypothalamus), dopamine (in the striatum), serotonin (in the cortex, striatum and hippocampus) [9]. Dopamine plays an important role in cognitive activity. Activation of dopaminergic transmission is necessary in the process of switching cognitive processes from one to another [10]. The role of norepinephrine is to maintain a state of active wakefulness. It is assumed that increased activity of the noradrenergic system is associated with better memory of emotionally charged events compared to emotionally neutral events [11].
Choline in combination with cytidine stimulates the secretion of normal neurotrophic amyloid precursor protein by rat brain cells [5]. The use of neurotrophic factors (for example, basic fibroblast growth factor) improves cognitive function in a model of ischemic encephalopathy by increasing the number of cholinergic neurons in the SA region of the hippocampus [11, 12]. Citicoline is able to reduce beta-amyloid deposition in the brain, and also, probably, stimulate the redistribution of the main glutamate transporter EAAT2 into microdomains of lipid rafts, which leads to increased glutamate uptake and is clinically manifested in improved integral indicators of cognitive functions [11].
The antiplatelet mechanism of action of the drug is a new subject for studying pleiotropic effects associated with the role of phospholipids in hemocoagulation processes [13]. Intravascular fibrin formation is characterized by profound disorders of the blood coagulation system with a simultaneous violation of the ratio between neutral (NPL) and acidic (APL) classes of phospholipids [14]. The process of transformation of fibrinogen into fibrin, accompanied by a decrease in the content of CPL and an increase in the level of NFL, introduces significant shifts in the relationships between these groups of phospholipids. It is characterized in each specific case by changes in their pro- or anticoagulant activity, which can manifest as a stimulating or inhibitory effect on prothrombin time, thromboplastic activity, blood clotting time, fibrinogen amount and fibrinolytic activity [15, 16].
Summarizing the above, we can distinguish the following mechanisms of action of Citicoline [5]:
1) maintaining normal levels of cardiolipin (the main component of mitochondrial membranes) and sphingomyelin;
2) activation of phosphatidylcholine biosynthesis;
3) stimulation of glutathione synthesis and weakening of lipid peroxidation processes (antioxidant effect);
4) normalization of Na+-K+-ATPase activity;
5) decreased activity of phospholipase A2;
6) activation of energy processes in neurons;
7) activation of neuronal mitochondrial cytochrome oxidases (normalization of tissue respiration processes);
 inhibition of glutamate-induced apoptosis;
inhibition of glutamate-induced apoptosis;
9) increased synthesis of acetylcholine and tyrosine hydroxylase activity, secretion of dopamine, increased levels of norepinephrine and serotonin.
When used in clinical practice, the pharmacological characteristics of Citicoline should be taken into account. The drug, when administered exogenously (both orally and intravenously), has 100% bioavailability [17]. After absorption, it breaks down into choline and cytidine, which easily penetrate the blood-brain barrier (BBB) and are distributed in the structures of the brain with the rapid introduction of choline into structural phospholipids and cytidine into cytidine nucleotides and nucleic acids. Citicoline is well absorbed when taken orally. After administration, the concentration of choline in the blood plasma increases significantly. The drug is metabolized in the intestines and liver with the formation of choline and cytidine. At the same time, only 15% of the administered dose is excreted from the human body: less than 3% by the kidneys and through the intestines, about 12% with exhaled CO2.
Citicoline increases the effects of levodopa drugs, which makes it possible to prescribe it to patients with neurodegenerative diseases, including Parkinson's disease, to reduce the dose of levodopa-containing drugs. Recommended treatment regimen: 1000 mg intravenously, intramuscularly or orally as a drinking solution once a day for 1-2 months.
Two important circumstances make a review of the properties of this neuroprotective and neuroreparative agent particularly timely. Firstly, starting in 2004, Citicoline began to be used in the USA [5]. Currently, Citicoline as a prescription drug is sold in more than 50 countries, including Europe (Spain, France, Russia), America (Mexico, Brazil, Argentina), Africa and the Middle East (Algeria, Jordan, Iraq) and Asia (Japan, China, South Korea). Secondly, there are few drugs developed for the treatment of neurological diseases that have such an evidence base both in experiment and in clinical practice: the total number of patients included in various studies of its effectiveness is about 12 thousand [18]. According to the results of a pooled analysis of data from 1372 patients participating in four clinical trials conducted in the United States, the use of Citicoline within 24 hours of the onset of stroke leads to regression of neurological deficits and functional recovery [18]. Compared with placebo, patients with an NIH score >8 points in the acute period of ischemic stroke who received Citicoline more often experienced complete recovery (Barthel index ≥95): placebo - 21%, citicoline - 33% (p = 0.05) [19]. Citicoline was well tolerated, with more side effects reported in the placebo group than in the active treatment group. Among all the studies on the effectiveness of the drug in patients with stroke, study C010 (Citicoline 010) is the first in which the dynamics of the infarction zone was assessed using magnetic resonance imaging [19]. As part of a pilot double-blind randomized study conducted at 4 Spanish academic hospitals involving 38 patients with intracerebral hematoma, who were prescribed the drug at a dosage of 2000 mg/day for 2 weeks within 6 hours after the onset of the disease, data on safety and effectiveness were obtained therapy [20]. The same conclusion was obtained in a large 6-center study in the Philippines [21]. A Cochrane review, including 14 studies involving 884 elderly patients with a variety of disorders, from memory impairment to mild vascular cognitive and senile dementia, noted a clear positive effect of the drug [22]. The duration of the studies ranged from 20 to 30 days, 1 study lasted for 6 weeks, 4 studies - 2-3 months, 1 study - 12 months. Multiple drug dosages, inclusion criteria, and outcome measures were used. The results demonstrated the effectiveness of Citicoline in improving memory and behavior, but not attention. There was a significant improvement in cognitive function compared to the placebo group. In elderly patients, taking Citicoline for 6 weeks led to a significant increase in the content in the frontal lobe (anterior cingulate cortex) of phosphocreatine (+17%), β-nucleoside triphosphates, in ATP (+14%), as well as the phosphocreatine ratio to inorganic phosphate (+32%) according to magnetic resonance spectroscopy [23]. In addition, a significant increase in phospholipid content in cell membranes was demonstrated. A number of studies in which the drug was administered to patients with Alzheimer's disease reported similar but moderate improvements in memory and behavior [24].
The effectiveness of Citicoline in patients with chronic cerebral ischemia (dyscirculatory encephalopathy) has also been confirmed by a number of clinical studies [25-30]. In this category of patients, not only a decrease in cognitive impairment was recorded, but also a decrease in the severity of symptoms of disorders of the extrapyramidal nervous system, gait disturbances, and postural instability. The effect is especially significant in clinical practice in the treatment of ischemic cochleovestibular syndromes. In 2010, an open-label study examined the therapeutic efficacy of Citicoline in patients with central vertigo of vascular etiology [31]. It is interesting that the drug was prescribed to young patients and healthy individuals [32, 33]. The use of Citicoline (Recognan) in a dose of 10 ml for 30 days contributed not only to the correction of cognitive, asthenic, but also emotional and autonomic disorders, and increased stress resistance [34]. The resulting positive effect persisted through the 2nd month of observation. Citicoline 500 mg improves attention scores in healthy female subjects compared to placebo [35]. A drink containing citicoline (250 mg) and caffeine improved short-term memory and attention in young healthy volunteers compared to placebo [36].
Choline alphoscerate
Choline alfoscerate (Gliatilin, Cereton) is a compound containing 40% choline and is converted in the body into a metabolically active form - phosphorylcholine, which can penetrate the BBB and activate the biosynthesis of acetylcholine in the presynaptic membranes of cholinergic neurons. It has a cholinomimetic effect, stimulates predominantly central cholinergic receptors, and according to its mechanism of action it is a centrally acting parasympathomimetic [37]. In the body it is broken down into choline and glycerophosphate. Provides the synthesis of acetylcholine and phosphatidylcholine of neuronal membranes, improves the functions of receptors and membranes in cholinergic neurons. The drug activates cerebral blood flow, stimulates the metabolism of the central nervous system (CNS), and stimulates the reticular formation. Improves mood, mental activity, concentration, memorization and the ability to reproduce received information, optimizes cognitive and behavioral reactions, eliminates apathy.
Currently, three main mechanisms of action of choline alfoscerate have been established [38]:
1) being a donor of acetylcholine, it helps restore neurotransmission;
2) carries out repair of neuronal membranes;
3) reduces the degeneration of free fatty acids.
Choline alfoscerate counteracts the biochemical and functional deficit of the cholinergic system affected by ischemia, which justifies its use in stroke [39]. Another mechanism of its action is the anabolic effect, manifested in the stimulation of membrane and glycerolipid synthesis due to the formation of membrane phospholipid precursors.
Animal experiments have shown that drugs of this series prevent induced cholinergic deficiency, prevent the development of dementia, and facilitate learning and memory processes by increasing the synthesis and release of acetylcholine in brain structures [40]. The psychophysiological role of acetylcholine is to ensure stability of attention, and acetylcholinergic deficiency leads to increased distractibility and rapid loss of received information.
The neuroprotective effects of exogenous choline sources in ischemic injury have been demonstrated for choline precursors in both preclinical and clinical studies. Most studies emphasize the effectiveness and dose-dependence of therapeutic effects [39].
After oral administration, absorption is 88%. Easily penetrates the BBB, accumulates mainly in the brain (concentration reaches 45% of the level in blood plasma), lungs and liver. Up to 85% of choline alfoscerate is excreted by the lungs in the form of carbon dioxide, the remaining amount (15%) is excreted by the kidneys and through the intestines.
Recommended treatment regimen: 1000 mg per day intramuscularly or intravenously for 10-15 days, once every 6 months, followed by switching to oral administration of 400 mg 3 times a day for 3 months. Nausea is possible during therapy, but may be a consequence of dopaminergic activation. During the treatment period, care should be taken when driving vehicles and performing work that requires increased attention, speed of mental and motor reactions [37]. No drug interactions have been established.
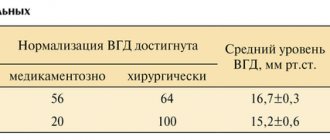
The available literature reviews 13 published clinical studies, involving 4054 patients, that primarily evaluated the use of choline alfoscerate in various forms of dementia, disorders of degenerative, vascular or combined origin, such as dementia of the Alzheimer's type or vascular dementia, and in acute cerebrovascular diseases ( transient ischemic attack and stroke) [41]. The administration of choline alfoscerate significantly improved the clinical condition of patients, especially the effect on the reduction of cognitive impairment (memory, attention). There have been 3 uncontrolled studies of choline alfoscerate in stroke and transient ischemic attack. The largest multicenter study of the effectiveness of choline alfoscerate in patients with ischemic stroke (without placebo control) was carried out in Italy with the participation of 2058 patients. The results of these studies indicate that this drug can contribute to the functional recovery of patients with cerebral stroke; the fact of the activating effect of choline alfoscerate is especially significant [42, 43]. In the Russian Federation, a multicenter study was conducted on the effectiveness of the use of choline alfoscerate in the treatment of patients with acute ischemic stroke, as a result of which the effectiveness and safety of the drug were confirmed [38]. A meta-analysis of the use of choline alfoscerate [44] documented the maximum effectiveness of the drug in relation to cognitive dysfunction, and choline alfoscerate is characterized by an effect on all types of memory. A multicenter, double-blind, randomized, placebo-controlled study in 2003, which assessed the effectiveness of the drug (400 mg 3 times a day for 180 days), made it possible to use choline alfoscerate for a long time without fear of side effects and complications [45]. In the ASCOMALVA study (Effect of association between a ChE-I and choline alphoscerate on cognitive deficits in Alzheimer's disease associated with cerebrovascular injury - "Effect of a combination of acetylcholinesterase inhibitors and choline alphoscerate on cognitive impairment in Alzheimer's disease associated with cerebrovascular disease"), in which 300 patients took part and were prescribed (depending on group allocation) a combination of donepezil and choline alfoscerate or donepezil alone for 12 months [46]. It has been established that combinations of donepezil and choline alfoscerate have advantages over donepezil alone [46]. It should be noted that choline alfoscerate has a dose-dependent effect; earlier administration of high doses of the drug is recommended to achieve maximum results of therapy [43].
Comparative analysis of the effectiveness of Citicoline and choline alfoscerate in pathologies associated with neurotransmitter dysfunction
Modern neurophysiology identifies several types of neurotransmitters that are significant for the implementation of adaptive processes in the brain. As factors controlling synaptic plasticity, most of them also appear to be involved in various types of cerebral pathology. The cholinergic system plays an important role in the pathogenesis of Alzheimer's disease, disorders of dopaminergic activity - Parkinson's disease, the glutamate system - in the pathogenesis of ischemic and traumatic brain lesions, the neurotransmitter function of serotonin turns out to be significant for depressive and other forms of mental disorders. In all these cases, we are talking about an inversion of the signaling function of neurotransmitters: their insufficient or, on the contrary, excessive activity causes disorganization of synaptic processes, therefore the use of Citicoline and choline alfoscerate is justified for various pathologies associated with neurotransmitter dysfunction. The drugs have a number of similar effects; they restore cell membranes, stimulate the synthesis of acetylcholine, have high bioavailability, are safe, and are effective in clinical practice. However, of the listed agents, it is Citicoline that has the greatest neuroprotective and neuroreparative potential.
Citicoline, thanks to its components (choline and cytidine), has a large number of mechanisms of action in cerebral ischemia, allows you to stabilize disturbed metabolic processes in the vascular wall and neurons, pathological processes in cell membranes (synthesis of more than 80% of phospholipids can be stimulated by changing the concentration of Citicoline) [5 ]. The drug inhibits the growth of the lesion when prescribed in the acute period in patients with ischemic stroke by reducing the active synaptic concentration of glutamate and reducing the degeneration of free fatty acids, causing blocking of special cellular channels, which directly correlates with a decrease in the size of the ischemic lesion and an increase in the level of ATP in the cortex and striatum. Along with this, it leads to a decrease in water content in brain structures during a major stroke. In hemorrhagic stroke, Citicoline prevents the increase in secondary ischemia in the absence of a pronounced stimulating effect associated with a balanced neurotransmitter effect (not only an increase in the release of acetylcholine, but also stimulation of dopamine and serotonin receptors). This property of Citicoline may make it possible to use it already at the pre-hospital stage in patients with stroke before verification of the nature of the lesion, including hemorrhagic stroke. It should be especially noted that the administration of the drug in recommended doses does not increase the threshold of seizure activity. The drug not only reduces the release of glutamate, but also promotes its reuptake, affecting the level of Na+ K+ ATPase, stabilizing the cell membrane, preventing the pathological flow of calcium into the cell. Cytidine, a precursor to the nucleotide uridine (a factor necessary for optimal synaptic transmission and neuronal communication), is itself a powerful nootropic. It acts as an additional factor in neurogenesis, since individual peptides with a short amino acid sequence and specific receptors (and therefore, pathways that modulate signaling processes), activating neurotrophic factors in the brain, presumably increase the activity of angio- and neovasculogenesis. Stimulation of these processes is an important element of neurorepair, therefore, clinically improves the rehabilitation of patients, especially with motor disorders [5].
In recent years, the role of neuroinflammation in the genesis of neurological diseases has been actively discussed. Focal ischemia causes a powerful inflammatory response within a few hours of its onset. Inflammation after ischemic stroke is part of reperfusion injury and is an important part of the damage to the neurovascular unit. Disturbances in metabolic and protein synthetic processes in the vascular wall and neurons underlie subsequent morphological damage - vascular or neurodegenerative, which are the basis for the further development and manifestation of a particular disease. Neurological disorders, as a rule, occur against the background of severe somatic pathology and are often accompanied by decompensation of the “old” lesion, especially in elderly patients, so priority is given to prescribing drugs that affect phospholipids and their metabolic products. Since phospholipids are the main structural component of all cell membranes, numerous cell functions directly depend on them. The more pronounced the hypoxia, the greater the consumption of phosphotidylcholine. Depletion of its pool exceeding 20% is accompanied by membrane death. Donation of a source of phosphotidylcholine can replenish its reserves, but not eliminate the cause of the disease, therefore Citicoline should primarily be considered as a universal membrane protector capable of preserving the matrix properties of biological membranes in patients with severe somatic pathology during the acute and recovery periods of stroke and traumatic brain injury with severe motor deficits, patients with Parkinson's disease, hypertensive encephalopathy with severe cognitive impairment.
Insufficient blood supply during stroke provokes the development of coagulation cascades that induce damage to endothelial cells. Expression of adhesion molecules such as P-selectin on platelets and endothelial cells increases as early as 15 min after the onset of ischemia, and a proinflammatory cascade is then rapidly initiated. In this regard, it should be noted the anti-inflammatory mechanism of action of Citicoline due to a decrease in the level of arachidonic acid, the phenomena of a “cytokine storm”. The drug can act as an agonist of dopamine receptors, therefore it is effective in the complex treatment of Parkinson's disease. Citicoline can delay the onset of the “dose wasting phenomenon” in the early stages of the disease, as well as reduce or maintain constant doses of levodopa in patients already receiving this specific therapy [47]. For chronic cerebral ischemia, Citicoline is the first-line drug in patients with postural disorders, including ischemic cochleovestibular syndromes, given the fact that dizziness is one of the most common complaints, including with venous discirculation [48].
This detailed analysis of the mechanisms of action, including use in young patients and healthy individuals to improve general status, is supported by the largest evidence base of any neuroprotective agent used. Citicoline is not only a source of choline. It is a supplier of cytidine, a precursor to the nootropic compound uridine.
The presence of a drinking solution, a dosing regimen of 1 time per day, and the absence of a dose-dependent effect suggest high patient adherence to Citicoline therapy. This fact is especially relevant for elderly (reduced risk of polypharmacy) and young (lack of complex regimens with rapid onset of effect) patients.
Since 2015, the citicoline drug Recognan has been used in the Russian Federation, which is available in 2 forms: 1) solution for intramuscular and intravenous administration 500 mg/4 ml, 1000 mg/4 ml; 2) oral solution 100 mg/ml in the form of: a bottle with a pipette of 30 ml of the drug; and sachets of 10 ml of the drug. In the acute period of ischemic stroke, Recognan (injection form) is prescribed according to the following regimen: 1000 g every 12 hours from the first day after diagnosis; 3-5 days after the start of treatment, if swallowing function is preserved, it is possible to switch to the oral form of the drug Recognan. The duration of treatment is at least 6 weeks. Recognan dosage regimen (oral solution): 500-2000 mg per day (5-10 ml 1-2 times a day or 1 sachet (1000 mg) 1-2 times a day), before use the drug can be diluted in 1 /2 glasses of water. The dosage and duration of administration depend on the severity of the patient's condition. When prescribing the drug to elderly patients, no adjustment of the treatment regimen is required [49].
At the same time, stimulators of acetylcholine synthesis (choline alfoscerate) are advisable to use when stabilizing life-supporting functions in any critical condition with damage to the central nervous system. They are the most active of the choline-containing phospholipids in increasing acetylcholine levels in the brain [50]. The fundamental difference between choline alfoscerate is its ability to normalize the level of acetylcholine in an acute situation; it has a pronounced awakening effect in patients in comatose states, but this limits its use in patients with an increased threshold for convulsive activity [51].
Thus, despite the differences, both drugs (Citicoline and choline alfoscerate) are effective and promising for the treatment of various neurological diseases. Priority use of Citicoline is recommended for patients:
— with severe somatic pathology in the acute period of stroke (especially with severe motor impairment), with possible use at the prehospital stage, with a normal or increased threshold of convulsive activity;
— in the recovery period of acute stroke, especially with severe motor disorders;
— in the complex treatment of neurological complications of hemostasis diseases, including thrombophilia and antiphospholipid syndrome;
— with chronic forms of cerebral ischemia in the presence of postural disorders, dizziness, signs of impaired venous outflow, cognitive impairment, predominantly mild or moderate severity (especially with impaired concentration);
— in complex therapy of Parkinson’s disease;
- elderly patients to reduce the risk of polypharmacy (single oral administration);
- young patients, taking into account high adherence to therapy.
Priority administration of choline alfoscerate is recommended for patients:
- with cerebral infarction in a comatose state, without an increased threshold of convulsive activity;
— in the recovery period of stroke, especially with severe cognitive impairment;
— with cognitive impairment of any severity, including in complex therapy of dementia. However, repeated administration and the use of high doses somewhat limits the use in geriatric patients.
It should be noted that after taking one drug, after a certain time (1-3 months) you can switch to another if certain symptoms prevail.
Indications for use of the drug Choline alfoscerate
- in the acute and recovery period of severe traumatic brain injury with a predominantly brain stem level of damage (impaired consciousness, coma, focal hemispheric symptoms, symptoms of brain stem damage);
- degenerative or involutional brain psychoorganic syndromes and consequences of cerebrovascular insufficiency, such as primary and secondary disorders of mental function in the elderly, characterized by memory impairment, confusion, disorientation, decreased motivation and initiative, decreased ability to concentrate;
- ischemic stroke;
- dementia of various origins (including Alzheimer's disease);
- changes in the emotional and behavioral sphere: emotional instability, irritability, decreased interest;
- senile pseudomelancholia.
Choline bitartrate
The simplest and cheapest form of choline. The problem is the almost complete lack of subjective sensation from taking it, especially when not combined with racetams. There are literally 4 cases in which taking choline bitartrate is justified. Let's sort them all out.
Kholin
329 rub.
- Pramiracetam. Due to the strong activation of choline uptake by neurons, ordinary choline bitartrate fully reveals itself only with pramiracetam. But even in this case, taking choline bitartrate alone is not entirely justified; the ideal combination for a pramiracetam course is: choline bitartrate + dmae bitartrate in a 1:1 ratio, since they are not completely interchangeable, and will complement each other as much as possible in this particular combination.
- Oxiracetam. Due to the mechanism of action of oxiracetam (increasing the release of acetylcholine by cholinergic neurons), additional intake of choline bitartrate in such a course is justified. But the combination of choline bitartrate + dmae bitartrate is more advantageous, which will be justified below.
- Inducing lucid dreams. To provoke lucid dreams, in addition to following the appropriate practices, additional intake of choline over long courses, up to several months, is essential. But even in this case, additional intake of DMAE is extremely desirable, due to their synergy.
- Liver protection. Since choline is a substance necessary for the synthesis of cell membranes, taking choline bitartrate is very, very reasonable, especially in combination with DMAE. Since only phosphatidylcholine is synthesized from choline, and phosphatidylethanolamine is also synthesized from DMAE. This combination can comprehensively help restore liver cell membranes.
Pramiracetam
3749 rub.
Oxiracetam
RUR 3,099
Conclusions and advice
The main conclusion: the combination of either choline bitartrate or Alpha GPC with DMAE, due to their synergistic action, is highly desirable.
It is not recommended to begin your acquaintance with nootropics with choline bitartrate, due to the almost complete absence of subjectively significant effects from this form of choline, so as not to be disappointed in the effectiveness of nootropics.
And I wanted to end with an unobvious, but important thing. To increase the synthesis of trimethylglycine from choline and dmae, it is necessary to increase the body's ability to methylate molecules, since the synthesis of trimethylglycine requires many methyl groups. And our body spends half of the methyl groups on the synthesis of creatine, and the conclusion suggests itself. Taking sources of choline will be very synergistic with taking creatine 2.5-5g per day, which will also provide nootropic and neuroprotective effects. And the increased synthesis of trimethylglycine will provide an additional stimulating and generally beneficial effect for the body, taking the effects of choline preparations to a fundamentally new level.
#nootropics
Citicoline (CDP - choline)
As a source of choline, citicoline is the most questionable solution. It was developed exclusively for intravenous administration; its large molecule is directly and instantly included in the so-called. Kennedy cycle (synthesis of neuronal membranes). It is designed to dramatically repair neuronal membranes in severe and acute conditions. But when taken orally, its large molecule disintegrates in the gastrointestinal tract and no longer has such a serious healing effect on neuronal membranes. In addition, the mass fraction of choline itself in citicoline is the smallest, and taking into account the cost of this drug, it is absolutely not suitable for inclusion in nootropic courses.
DMAE
DMAE or dimethylaminoethanol is a choline molecule lacking a methyl group. This gives it greater ability to penetrate the brain, through the blood-brain barrier, and also gives it antioxidant abilities. DMAE enters our body in three ways. From it, a membrane molecule is directly synthesized - phosphatidylethanolamine, which improves the so-called. membrane fluidity. For example, receptor complexes across the membrane are able to move at higher speeds, which also affects the functioning of the brain as a whole.
DMAE
399 rub.
DMAE is methylated to choline and subsequently acetylcholine is synthesized from it - a memory molecule so necessary for all people who want to increase their cognitive abilities, but also phosphatidylcholine - a membrane phospholipid, a necessary molecule, like phosphatidylethanolamine for absolutely all cells.
But the trimethylglycine (betaine) molecule is also synthesized from DMAE, which is actively used in sports nutrition and is responsible for cell hydration and endurance. The stimulating effect of DMAE on the psyche is associated with an increase in the synthesis of this molecule.