Not to be confused with anticholinergic or cholinergic effects.
Chemicals that prevent the breakdown of acetylcholine and butyrylcholine.
Acetylcholine Sarin molecule, C4H10FO2P TERP molecule, C8H20O7P2
Cholinesterase inhibitors
(ChEIs), also known as
anti-cholinesterases
, are chemicals that prevent the breakdown of the neurotransmitter acetylcholine or butyrylcholine. This increases the amount of acetylcholine or butyrylcholine in the synaptic cleft, which can bind to muscarinic receptors, nicotinic receptors, and others. This group of inhibitors is divided into two subgroups: acetylcholinesterase inhibitors (AChEI) and butyrylcholinesterase inhibitors (BChEI). [1] [2] [3]
ChEIs can be used as drugs for Alzheimer's disease and myasthenia gravis, and as chemical weapons and insecticides. [4] [5] Side effects when used as medications may include loss of appetite, nausea, vomiting, loose stools, vivid dreams at night, dehydration, rash, bradycardia, peptic ulcers, seizures, weight loss, rhinorrhea, salivation, muscle cramps , and fasciculations. [6] [7]
ChEIs are indirectly acting parasympathomimetic drugs. [8]
During treatment at Berlin's Charité hospital for Russian dissident Alexei Navalny, a nerve agent known to belong to Novichok agents was revealed to be ChEI. [9]
Since November 2022, the ACheI group known as Novichoks
, are prohibited as agents of war under the Chemical Weapons Convention. [10] Novichok agents are neurotoxic organophosphates and are considered more potent than VX gas, also a neurotoxic organophosphate. [eleven]
Medical use[edit]
Further information: Donepezil § Medical uses
While 4 ChEIs are approved in the US, only three are commercially available. [6] The three available drugs are rivastigmine, donepezil and galantamine, but tacrine is not. [6] They are commonly used to treat Alzheimer's disease and dementia. [6] If improvement occurs, it is usually within the second or third month after onset. [6]
It is difficult to determine which ChEI has superior efficacy due to design flaws in direct comparison studies. [12]
How do they behave when they get into the blood?
Cholinesterase inhibitors, when absorbed into the blood, show the following effects - improvement of memory and learning, activation of motor skills, but at the same time inhibition of cardiac activity, lowering blood pressure, contraction of smooth muscles, and increased secretory function of the glands. A person may experience reflex shortness of breath, a release of adrenaline and norepinephrine, and an increase in skeletal muscle tone. Inhibitors individually affect the state of the body. If we talk about average symptoms, then most often they give a decrease in heart rate and pressure. However, sometimes they can cause the opposite - tachycardia and increased blood pressure.
What is tau protein and how is it related to Alzheimer's disease? More details
Binding affinity[edit]
Acetylcholinesterase inhibitors[edit]
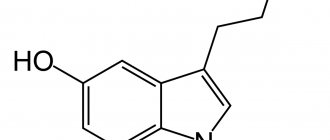
Donepezil, Phenserine, huperzine and BW284c51 are selective AChE inhibitors. [14] [12]
Butyrylcholinesterase inhibitor[edit]
Tetra(monoisopropyl) pyrophosphoramide (Iso-OMPA) and ethopropazine are selective BuChE inhibitors. [14]
AChE and BChE inhibitor[edit]
Paraoxon and rivastigmine are acetylcholinesterase inhibitors and butyrylcholinesterase inhibitors. [14] [12] [7]
In 2015, the US Food and Drug Administration's Adverse Event Reporting System database compared rivastigmine with other CEI drugs donepezil and galantamine and found that rivastigmine was associated with a higher incidence of death as an adverse event. [15]
Acetylcholinesterase inhibitors and nicotinic receptor modulator[edit]
See also: allosteric modulator and nicotinic receptor
Galantamine may be less well tolerated than donepezil and rivastigmine. [12]
Cholinesterase is an enzyme necessary for the normal functioning of the nervous system. It comes in two types: acetylcholinesterase, which plays a role in the transmission of nerve impulses, and pseudocholinesterase, which is found in the serum and cells of some internal organs and is involved in the processing and decomposition of chemicals that enter the body.
Synonyms Russian
Butyrylcholinesterase, pseudocholinesterase, BCHE, acetylcholinesterase.
English synonyms
CHS, AChE, RBC cholinesterase, red cell cholinesterase, BChE, plasma cholinesterase, pseudocholinesterase, PCHE, erythrocyte acetylcholinesterase, butyrylcholinesterase.
Research method
Kinetic colorimetric method.
Units
U/L (unit per liter).
What biomaterial can be used for research??
Venous blood.
How to properly prepare for research?
- Do not eat for 8 hours before the test; you can drink clean still water.
- Avoid physical and emotional stress and do not smoke for 30 minutes before the test.
General information about the study
Cholinesterase is an enzyme necessary for the functioning of the nervous system.
There are two types of cholinesterase in the body: acetylcholinesterase, present in red blood cells, as well as in the lungs, spleen, nerve endings and gray matter of the brain, and pseudocholinesterase (butyrylcholinesterase), found in the blood serum, liver, muscle, pancreas, heart and white matter of the brain. . Acetylcholinesterase is involved in the transmission of nerve impulses by breaking down acetylcholine, a chemical that transmits signals through the endings of nerve cells. Decreased acetylcholinesterase activity leads to the accumulation of acetylcholine in nerve endings. This, in turn, leads to over-irritation of nerve cells.
Pseudocholinesterase is necessary for the breakdown and metabolization of toxins and drugs.
What is the research used for?
- To test a patient who has been exposed to pesticides containing organophosphates - they may inhibit cholinesterase and pseudocholinesterase activity. Symptoms appear abruptly in cases of acute poisoning or may occur gradually over chronic exposure to these substances. Insecticides can enter the body through inhalation, ingestion, or skin contact.
- To identify hereditary pseudocholinesterase deficiency. Sometimes enzyme deficiency can be inherited due to genetic variations in the enzyme. Pseudocholinesterase is necessary for the body to inactivate succinylcholine, a muscle relaxant commonly used during surgery. In patients with low activity or a defective form of pseudocholinesterase after anesthesia, the effect of medications may be delayed, threatening prolonged muscle paralysis and suffocation.
When is the study scheduled?
- Periodically for patients using organophosphorus substances in agriculture or the chemical industry.
- When assessing acute poisoning from harmful substances that may cause neuromuscular damage. Symptoms of poisoning vary depending on the substance, its quantity and method of entry into the body: headache, dizziness, nausea, increased tearing and salivation, sweating. In very severe poisoning, additional symptoms appear: vomiting, diarrhea, darkening or blurred vision due to constriction of the pupils, muscle weakness, convulsive twitching, poor coordination of movements, slow breathing leading to respiratory failure and the need for artificial ventilation.
- Before surgery, if close relatives of the patient have ever had prolonged paralysis and suffocation after using succinylcholine.
What do the results mean?
Reference values
| Floor | Reference values |
| Female | 4260 - 11250 U/l |
| Male | 5320 - 12920 U/l |
When pesticide poisoning is detected
After poisoning with organophosphorus substances, the activity of acetylcholinesterase and pseudocholinesterase can become 80% less than normal, and when the drop is more than 40%, symptoms become severe.
A significant decrease in cholinesterase activity usually indicates excessive absorption of organophosphates by the body.
When testing for sensitivity to succinylcholine
In 3% of people, pseudocholinesterase activity is reduced due to heredity, and if administered the muscle relaxant succinylcholine, they will experience its effects for a longer period of time than necessary. In such patients, low pseudocholinesterase activity indicates an increased risk of prolonged muscle relaxant action.
In addition, cholinesterase activity may be decreased in chronic liver disease and malnutrition, pregnancy, kidney failure, shock, and some types of cancer.
Further reading[edit]
- Institute, National; (UK), Care Excellence (2019-12-27). "Cholinesterase inhibitors and memantine in dementia". NCBI Bookshelf
. Retrieved December 27, 2022. - Parsons, Chris J.; Danish, Wojciech; Dekundi, Andrzej; Pulte, Irena (05/09/2013). "Memantine and cholinesterase inhibitors: complementary mechanisms in the treatment of Alzheimer's disease". Neurotoxicity Study
.
Springer Science and Business Media LLC. 24
(3): 358–369. doi:10.1007/s12640-013-9398-Z. ISSN 1029-8428. PMC 3753463. PMID 23657927. - Meng, Yan-Hong; Wang, Pan Pan; Song, Ya - Xue; Wang, Jian-Hua (03/01/2019). "Cholinesterase inhibitors and memantine for the treatment of dementia in Parkinson's disease and dementia with Lewy bodies: a meta-analysis". Experimental and Curative Medicine
.
17
(3):1611–1624. DOI: 10.3892/etm.2018.7129. ISSN 1792-0981. PMC 6364145. PMID 30783428. Retrieved December 27, 2022.
Treatment of mental disorders (cholinesterase inhibitors)
Cholinesterase inhibitors are also called acetylcholinesterase (AChE) inhibitors or anticholinesterases. They are a group of drugs that block the normal breakdown of acetylcholine (ACh) into acetate and choline and thereby increase both the levels and duration of action of acetylcholine in the central and peripheral nervous system. Acetylcholinesterase inhibitors are most often used in the treatment of neurogenerative diseases such as Alzheimer's disease, Parkinson's disease and Lewy body dementia. Various physiological processes in these degenerative disorders destroy cells that produce ACh and thereby reduce cholinergic transmission in different brain regions. Cholinesterase inhibitor drugs inhibit AChE activity and maintain ACh levels by decreasing the rate of its breakdown.
In addition, cholinesterase inhibitors are often used in patients with myasthenia gravis. Increased levels of acetylcholine at the neuromuscular junction therefore lead to increased activation of ACh receptors found on postsynaptic membranes, resulting in improved muscle activation, contraction and strength. At the end of therapy, cholinesterase inhibitors, most commonly neostigmine, are administered to reverse the effects of nondepolarizing muscle agents such as rocuronium.
Cholinesterase inhibitors are also required for use when anticholinergic poisoning is suspected. Symptoms of anticholinergic poisoning include vasodilation, anhidrosis, mydriasis, delirium, and urinary retention. Other less common indications for cholinesterase inhibitors include the treatment of patients diagnosed with certain mental disorders, such as schizophrenia, and the treatment of glaucoma by relieving aqueous humor pressure.
Cholinesterase inhibitors function by inhibiting cholinesterase from hydrolyzing acetylcholine to its acetate and choline components, thereby increasing the availability and duration of action of acetylcholine at the neuromuscular junction. The enzyme cholinesterase has two active sites: an anionic site formed by tryptophan and an esteractic site formed by serine. Cholinesterase inhibitors, such as organophosphates, prevent the cleavage of cholinesterase by acetylcholine by interacting with the esteractic site. As a result, acetylcholine will continue to accumulate and activate associated receptors.
Cholinesterase inhibitors are classified as reversible, irreversible or pseudoreversible. Reversible cholinesterase inhibitors are commonly used for therapeutic purposes. In contrast, irreversible and pseudo-reversible inhibitors are often used in pesticides and biological warfare (nerve agents).
Cholinesterase inhibitors come in different forms for administration. Many available cholinesterase inhibitors are administered intramuscularly, intravenously, or orally. Different forms may be available for different types of cholinesterase inhibitors. For example, neostigmine is in a solution form used to counteract the muscle relaxant at the end of surgery. For patients with myasthenia gravis, an oral form of neostigmine is available for treatment. Rivastigmine, used in patients with dementia, comes in a transdermal patch form that is also often used.
Cholinesterase inhibitors increase the total amount of acetylcholine available. Thus, symptoms of overstimulation of the parasympathetic nervous system may be present, such as hypersensitivity, hypersecretion, bradycardia, miosis, diarrhea, and hypotension.
A major concern when prescribing cholinesterase inhibitors or exposure to organophosphates is potentially the development of cholinergic crisis, also known as SLUDGE syndrome ( S:
salivation;
L:
lacrimation;
U:
urination;
D:
diaphoresis;
G:
gastrointestinal disorders;
E:
emesis). Temporary side effects when patients are prescribed cholinesterase inhibitors include headache, insomnia, and minor gastrointestinal problems. Other more important effects include weakness and weight loss. Prolonged muscle contraction may also be a characteristic feature in patients exposed to cholinesterase inhibitors. Cholinesterase inhibitors, such as neostigmine, used postoperatively to reverse neuromuscular blockade may result in potential residual neuromuscular blockade.
Because of the ability to increase vagal tone through activation of the parasympathetic nervous system, caution should be exercised when prescribing cholinesterase inhibitors to individuals suffering from bradycardia or cardiac conduction diseases such as sick sinus syndrome. These people are at risk of fainting and falling. Caution is also recommended in patients taking antihypertensive drugs due to the possibility of severe hypotension. In addition, cholinesterase inhibitors are also contraindicated in patients with gastric ulcers due to the increased risk of gastrointestinal bleeding. Patients with urinary retention should also not receive cholinesterase inhibitors due to the risk of increased retention. This effect is particularly noticeable in patients being treated for dementia and Alzheimer's disease, since urinary incontinence is a common clinical feature in these patients. Administration to patients with previous allergies or hypersensitivity to cholinesterase inhibitors and its derivatives is also contraindicated.
References
- Kamyshnikov, V.S. Handbook of clinical and biochemical laboratory diagnostics. Minsk, 2000. -T. 2. - P. 258¬260.
- Starostina, V.K., Degteva, S.A. Cholinesterase: methods of analysis and diagnostic value. Information and methodological manual. Novosibirsk, 2008.
- Bajgar, J., Bartosova, L., Kuca, K. et al. Changes of cholinesterase activities in the rat blood and brain after sarin intoxication pretreated with butyrylcholinesterase. Drug Chem. Toxicol., 2007. - Vol. 30. - No. 4. - R. 351-359.
- Ghebremedhin, E., Thal, D., Schultz, C. et al. Homozygosity for the K variant of BCHE gene increases the risk for development of neurofibrillary pathology but not amyloid deposits at young ages. ActaNeurophatol., 2007. - Vol. 114. - No. 4. - P. 359–363.
- Giacobini, E. Cholinesterases: new roles in brain function and in Alzheimer's disease. Neurochem. Res., 2003. - Vol. 28. - No. 3–4. — P. 515–522.
- Girard, E., Bernard, V., Minic, J. et al. Butyrylcholinesterase and the control of synaptic responses in acetylcholinesterase knockout mice. Life Sci, 2007. - Vol. 80. - No. 24–25. — P. 2380–2385.



![Table 1. Side effects of PPIs [1, 4–7] (end) Table 1. Proton-pump inhibitors side effects [1, 4–7]](https://laram-halal.ru/wp-content/uploads/tablica-1-pobochnye-effekty-ipp-1-4-7-okonchanie-table-330x140.jpg)