Meningococcal infection
Treatment should be started immediately . The first medical aid to the patient must be provided by the doctor who first suspected or diagnosed meningococcemia. The patient needs to be administered chloramphenicol succinate 25 mg/kg IU (single dose) + prednisolone 2-3 mg/kg. It is preferable to administer these drugs intravenously, since if microcirculation is impaired, intramuscular administration of antibiotics and hormones is not effective. If there are signs of ITS, the main treatment is the use of massive doses of corticosteroids from 5 to 20 mg/kg, replenishment of the circulating blood volume (administration of drugs only intravenously).
It is necessary to hospitalize the patient as quickly as possible. Patients with generalized forms of meningococcal infection or with suspicion of them are subject to emergency hospitalization in a specialized department of an infectious diseases hospital by an emergency medical team. If there are signs of ITS - by the resuscitation team.
With a progressive deterioration of the patient’s condition, hospitalization to the nearest intensive care unit is indicated, and only after stabilization of the patient’s condition, transfer to a specialized hospital.
Patients with generalized forms of MI or suspected of them are subject to mandatory hospitalization. On an outpatient basis, only patients with localized forms can be treated: meningococcal carriers and nasopharyngitis with a mild and short-term course in the absence of preschool children or childcare workers in the family.
Treatment of patients in a hospital is carried out according to the protocol (Order of the Ministry of Health of Ukraine No. 354 of July 9, 2004 “On the approval of protocols for the diagnosis and treatment of infectious diseases in children”):
I. Nasopharyngitis Antibacterial therapy: – rifampicin – 10 mg/kg per day for 3-5 days or macrolides (erythromycin, spiramycin, azithromycin), or levomycin.
II. Meningococcal carriage - rifampicin - 2-3 days.
III. Purulent meningitis Prehospital stage of treatment: – ensuring venous access; – antibacterial therapy – chloramphenicol succinate – 25 mg/kg (single dose); – glucocorticoids – 1-3 mg/kg for prednisolone; – infusion therapy with saline and colloid solutions; – antipyretics; – furosemide – 1-2 mg/kg; – for convulsions – diazepam (inpatient stage of treatment); – antibacterial therapy: benzylpenicillin – 300-500 mg/kg administered 6 times a day (reserve antibiotics: ceftriaxone – 100 mg/kg per day, cefotaxime – 200 mg/kg per day; if there are signs of ITS – chloramphenicol succinate – 100 mg/ kg per day; - detoxification therapy for moderate forms using glucose-saline solutions; - diacarb + asparkam. The dose is selected depending on the severity of the hypertension syndrome; - syndromic therapy; - during the period of convalescence: nootropics, B vitamins.
IV. Meningococcemia Prehospital stage of treatment: – ensuring venous access; – antibacterial therapy; – chloramphenicol succinate – 25 mg/kg (single dose) intravenously; – glucocorticoids – prednisolone, hydrocortisone or dexazone – 2-3 mg/kg for prednisolone – without ITS (for ITS grade 1 – 5 mg/kg, 2nd – 10 mg/kg, 3rd – 15-20 mg/kg kg); – infusion therapy with saline solutions or rheopolyglucin to stabilize the bcc; – inotropes (dopamine) – to maintain hemodynamics (inpatient stage of treatment); – depending on the severity of the condition, hospitalization of the patient in the intensive care unit or in the department of neuroinfections of an infectious diseases hospital; – antibacterial therapy: in the presence of ITS, the drug of choice is chloramphenicol succinate at a dose of 100 mg/kg per day (when removing a patient from ITS, penicillin 200 mg/kg per day or cephalosporins 100 mg/kg per day are prescribed). In severe cases and the need to protect against nosocomial infection, 3rd generation aminoglycosides are additionally used - amikacin - up to 20 mg/kg per day, netilmicin - 1.5-2.0 mg/kg every 8 hours; – detoxification therapy for moderate forms is carried out with glucose-salt solutions, taking into account the daily fluid requirement and pathological losses; – syndromic therapy – according to the appropriate treatment protocols. Patients are discharged based on clinical recovery after normalization of laboratory parameters of the cerebrospinal fluid and general blood test. A control swab from the nasopharynx is taken in the hospital no earlier than three days after antibacterial treatment.
Consequences of generalized forms of meningococcal infection Clinical and laboratory studies have shown that upon discharge from the hospital, the majority of patients have not yet achieved complete restoration of all impaired functions. Children who have had purulent meningitis must be registered with a neurologist for 2-3 years.
It is advisable not to send children to child care institutions during the first 2-3 weeks after discharge.
The most common consequence of meningococcal infection is cerebrasthenic syndrome, manifested by increased fatigue, sleep disorders, appetite, decreased academic performance, and changes in behavior. For younger children, emotional instability, motor disinhibition, absent-mindedness, and sometimes aggressiveness are more typical.
If cerebrovascular disease is detected, the child must be provided with a gentle regime, proper organization of work and rest, limiting the time of watching TV and working with the computer to a minimum, increasing the time of sleep and spending time in the fresh air, and restorative therapy. During the recovery period, nootropics, multivitamins, and vascular medications are prescribed under the control of Dopplerography of cerebral vessels.
Meningococcus is not only in Africa
This infection is widespread throughout the world. And in Africa there is even a so-called “meningitis” or “meningococcal belt”:
However, this disease does not only exist somewhere far away, on other continents; unfortunately, it is also close to us. Outbreaks of meningococcal infection are recorded every now and then in different regions of Russia.
For example, in Novosibirsk in 2022, 25 cases of the disease were registered in less than two weeks. And this is very characteristic of this infection: usually long periods of well-being (10-15 years) are interrupted by sharp increases in incidence, which have a focal outbreak nature.
The increase in incidence can be explained by the widespread carriage of meningococcal bacteria. As the number of susceptible individuals increases, the number of cases increases. And declines are ensured by an increase in the immune layer as a result of latent immunization as bacterial carriage spreads among the population of a given territory.
You need to understand that during recession years the infection does not disappear: 50% of diseases occur in children under 5 years of age; 20% - for children aged 6-14 years. As age increases, incidence rates decrease, but carriage rates increase. The age group of 15-20 years is also subject to a high degree of susceptibility, because its representatives - students, military personnel - communicate intensively in schools, dormitories, barracks, etc. First of all, those who come from remote areas get sick, i.e. not previously in contact with the pathogen.
Why are doctors sometimes unable to identify meningococcal infection in the early stages of the disease and provide timely assistance? The fact is that the first symptoms of the disease are similar to the onset of a regular acute respiratory viral infection, and later medicine turns out to be powerless against the lightning-fast course of the disease. Moreover, during periods of prosperity, cases of the disease are so rare that the alertness of even experienced doctors, not to mention young novice doctors, gradually decreases.
One of the features that can also be canceled is that meningococcal infection is characterized by a winter-spring seasonality with the maximum number of diseases in February – April.
There are many real stories about how this can happen, here is one of them (a video from our partners - Sanofi Pasteur):
Clinical signs and symptoms
Depending on the pathogen, the incubation period can vary and for bacterial meningitis range from two to 10 days. Since bacterial meningitis is often accompanied by sepsis, the described clinical signs and symptoms apply to both pathologies.
Clinical signs and symptoms:
- severe headaches
- stiff neck or neck pain
- severe increase in body temperature
- photophobia
- confusion, drowsiness, coma
- convulsions
- rash
- joint pain
- cold extremities
- vomit
Infants may have the following symptoms:
- loss of appetite
- drowsiness, lethargy, coma
- irritability, crying when moving
- difficulty breathing, wheezing
- elevated body temperature
- stiff neck muscles
- swollen fontanel
- characteristic high-pitched scream
- convulsions
- vomit
- rash
- pale or blotchy skin
Disease Prevention
Post-infectious immunity. After an illness, a strong immunity develops that protects against re-infection. However, it occurs only in the serogroup of bacteria that caused the disease. In total, there are 12 types of meningococcal groups.
- Vaccination. 3 types of vaccines have been developed:
- Polyvalent polysaccharides (invented 30 years ago).
- Mono- and polyvalent conjugate vaccines (used since 1999).
- New monovalent conjugate vaccine MenA (developed in 2010-2011).
As much as possible, the drug can cover only 4 serogroups: A, C, Y and W. Unfortunately, such a vaccine has not yet been developed to protect against all types of infection.
The meningococcal vaccine is not included in the childhood vaccination schedule. You can only get vaccinated yourself. It should be carried out before traveling to countries at risk and for epidemiological reasons, i.e. during an epidemic when the serotype is known.
How does infection occur?
The causative agent of meningococcal infection is the bacterium Neisseria meningitides. There are 12 varieties of it, six of which lead to severe forms of the disease. The bacterium is covered with a special capsule, which makes it especially resistant to immune cells.
In most cases, carriage of meningococcus on the mucous membrane does not cause noticeable health problems. And only 10-15% of cases this leads to the development of inflammation.
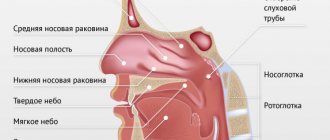
The route of transmission is airborne. The bacterium enters a healthy body through the mucous membrane of the mouth and nasopharynx during close contact with a sick person or carrier.
ON A NOTE! According to WHO statistics, asymptomatic carriers of Neisseria meningitides are from 10 to 20% of the population.
Through the mucous membrane, the pathogen enters the bloodstream and, quickly multiplying, spreads throughout the body, leading to sepsis (blood poisoning), inflammation of the internal organs, and the membranes of the brain. The first signs may appear after 24-48 hours. In general, the incubation (hidden) period can last from a day to 10 days.
ON A NOTE! The disease is classified as a “war” infection, since the increase in incidence is directly correlated with wars, as well as major disasters and accidents. Almost any situation that leads to stress, as well as significant crowding of people in poor living conditions, leads to the occurrence of meningococcal infection. It has been proven that if the number of meningococcal carriers in a team reaches 20% or more, then clinically pronounced forms of the disease appear.
Who is at risk?
Meningitis affects people of all ages, but young children are most at risk. Newborns are at greatest risk of infection with group B streptococcus, and young children with meningococcus, pneumococcus and haemophilus influenzae. Adolescents and young adults are at greater risk for meningococcal disease, while older adults are at greater risk for pneumococcal disease.
Residents of all regions of the world are at risk for meningitis. The greatest disease burden is found in a region of sub-Saharan Africa known as the “African meningitis belt,” which is at particularly high risk for epidemics of meningococcal as well as pneumococcal meningitis.
The greatest risk occurs in settings where people are in close contact, such as large gatherings, refugee camps, overcrowded housing, or student, military, and other professional environments. Immunodeficiency associated with HIV infection or complement deficiency, immunosuppression, active or passive smoking can also increase the risk of developing various types of meningitis.
Treatment
Without adequate treatment, meningitis is fatal in half of patients and should always be considered an emergency. Hospitalization is indicated for all patients with meningitis. As a rule, it is not recommended to isolate patients after 24 hours from the start of treatment.
For bacterial meningitis, treatment with appropriate antibiotics should be started as soon as possible. Ideally, a lumbar puncture should be performed before starting a course of antibiotics, as antibiotics may make it difficult to perform a cerebrospinal fluid culture. However, the type of pathogen can also be determined by testing a patient's blood sample, and prompt treatment remains a priority. A wide range of antibiotics are used to treat meningitis, including penicillin, ampicillin and ceftriaxone. During epidemics of meningococcal and pneumococcal meningitis, ceftriaxone is the drug of choice.
Complications and consequences
During illness, the following complications may occur:
- cerebral edema;
- hydrocephalus;
- hemorrhagic cerebral stroke;
- acute renal failure;
- paralysis and other dysfunctions.
Against the background of meningococcal infection, herpes, otitis media, and meningococcal pneumonia can develop. Severe disease can cause the development of asthenic syndrome, expressed in general weakness and periodic headaches. Lead to arterial hypertension, hearing loss, epilepsy and hemiparesis (paralytic damage to one side of the body). Patients who have had meningococcal infection often experience apathy and depression.