- Etiology and pathogenesis
- Classification of tonsillitis Clinical forms of vulgar tonsillitis
- Treatment of vulgar tonsillitis.
As a disease of the pharynx, sore throat has been known since ancient times.
Sore throat is described in the works of Hippocrates (IV–V century BC), Celsus (I century AD), and also in the manuscripts of the Tajik physician Abu Ali Ibn Sina (Avicenna, 11th century) mention of intubation and tracheotomy for asphyxia due to tonsillitis, etc. Sore throat is a common acute infectious disease in which local inflammation affects the lymphadenoid tissue of various tonsils of the pharynx. In the vast majority of cases, tonsillitis occurs in the palatine tonsils, while other tonsils are involved in the process much less frequently. Angina is not a homogeneous disease; it differs in etiology, pathogenesis and form of clinical course.
Etiology and pathogenesis
Among the various possible microbial pathogens of sore throat (cocci, bacilli, viruses, spirochetes, fungi, etc.), in most cases the main etiological role belongs to group A b-hemolytic streptococcus (GABHS). This pathogen, according to a number of authors, is detected in sore throat in more than 80%, according to other sources - in 50–70% of cases. Much less frequently, acute tonsillitis is caused by group C and G streptococci, Arcanobacterium haemolyticum, Neisseria gonorrhoeae, Corynebacterium diphtheria (diphtheria), anaerobes and spirochetes (Simanovsky-Plaut-Vincent angina), and extremely rarely by mycoplasma and chlamydia. The cause of acute viral tonsillitis can be adenovirus, rhinovirus, coronavirus, influenza and parainfluenza viruses, Epstein-Barr virus, Coxsackie A virus and others. Penetration of an exogenous pathogen into the mucous membrane of the tonsils can occur through airborne droplets and alimentary routes, as well as through direct contact. In the occurrence of an endogenous pathogen, great importance is attached to chronic tonsillitis. As noted by B.S. Preob¬ra¬zhensky (1954), the frequency of sore throats in chronic tonsillitis is explained by the fact that in this disease there are usually up to 75% of cases of carriage of GABHS, vegetating in the crypts of the palatine tonsils.
In the pathogenesis of tonsillitis, a certain role can be played by a decrease in the body’s overall reactivity to cold, sharp seasonal fluctuations in environmental conditions (temperature, humidity, nutrition, intake of vitamins, etc.), trauma to the tonsils, constitutional predisposition to tonsillitis (for example, in children with lymphatic – hyperplastic constitution), the state of the central and autonomic nervous system. Factors predisposing to angina are chronic inflammatory processes in the mouth, nose and paranasal sinuses. The development of sore throat occurs according to the type of allergic-hyperergic reaction, which is a prerequisite for complications such as rheumatism, acute diffuse nephritis and other diseases of an infectious-allergic nature and associated with the GABHS antigen.
Causes and routes of infection for sore throat
The inflammatory process develops under the influence of pathogenic microflora. The causative agent of the pathology is considered to be:
- staphylococcal;
- streptococcal;
- energy virus;
- pneumococcal;
- diplococcal infection.
The main ways of contracting tonsillitis are:
- airborne - when sneezing, coughing or talking to a carrier;
- hematogenous - microflora moves along with the blood from foci of inflammation located in other areas;
- enteral - pathogens enter with food (uncooked milk), through unwashed hands;
- endogenous – formed against the background of caries, gastroenteritis, purulent sinusitis;
- traumatic – formed during operations on the ENT organs.
Sore throat occurs at any age, the risk of its occurrence is associated with an inadequate diet, without a sufficient amount of nutrients, overwork, and severe hypothermia. The pronounced activity of pathogens indicates dysfunction of the immune system.
Classification of sore throats
In practice, the classification of B.S. is most widespread. Preobrazhensky, based on pharyngoscopic signs, supplemented by data obtained during laboratory research, sometimes with information of an etiological or pathogenetic nature.
This classification includes the following forms of sore throat: I - catarrhal, II - follicular, III - lacunar, IV - fibrinous, V - herpetic, VI - phlegmonous (intratonsillar abscess), VII - ulcerative-necrotic (ganrenous), VIII - mixed forms.
To this main diagnosis, after obtaining the appropriate data, the name of the microbe that caused the sore throat (streptococcal, staphylococcal, etc.) or other characteristic features (traumatic, toxic, monocytic, etc.) can be added.
It is customary among clinicians to divide all existing sore throats into vulgar (or banal) and atypical.
Vulgar tonsillitis is characterized by the presence of four general signs: (1) there are severe symptoms of general intoxication of the body; (2) there are pathological changes in both tonsils; (3) the duration of vulgar sore throat does not exceed 7 days (1 week); (4) the primary factor in the etiology of these sore throats is a bacterial or viral infection.
Clinical forms of vulgar tonsillitis
Among a large group of sore throats, the most common are vulgar (ordinary, banal) sore throats, which arise in connection with the introduction of one or another microbial or viral infection. These sore throats are recognized mainly by pharyngoscopic signs. These include catarrhal, lacunar, follicular, fibrinous and phlegmonous (intratonsillar abscess). The most common forms are:
Catarrhal sore throat.
The disease begins acutely, with burning sensations, dryness, soreness in the throat, and then slight pain when swallowing. I am concerned about general malaise, weakness, headache. Body temperature is usually low-grade; There are slight inflammatory changes in the peripheral blood. Faringoscopically, diffuse hyperemia of the tonsils and the edges of the palatine arches is determined; the tonsils are somewhat swollen. The tongue is dry and coated. There is often a slight enlargement of regional lymph nodes. In rare cases, catarrhal tonsillitis is more severe. In childhood, clinical phenomena are more pronounced than in adults. Usually the illness lasts 3–5 days.
Follicular tonsillitis.
It is characterized by predominant damage to the parenchyma of the tonsils and their follicular apparatus. Like lacunar, follicular tonsillitis begins with sudden chills with an increase in body temperature to 40°C, severe sore throat. The phenomena of intoxication are pronounced. Patients are concerned about severe general weakness, headache, pain in the heart, joints and muscles. Sometimes dyspepsia and oliguria are observed. The palatine tonsils are hyperemic and sharply swollen. Follicles in the form of whitish-yellowish formations the size of a pinhead are visible through the epithelial cover. The surface of the tonsil, in the figurative expression of N.P. Simanovsky, takes on the appearance of a “starry sky”. Regional lymphadenitis is pronounced.
Lacunar tonsillitis.
The onset of the disease and its general symptoms are the same as with follicular tonsillitis. More often, lacunar tonsillitis is more severe than follicular tonsillitis. The pharyngoscopic picture in lacunar angina is characterized by the appearance on the hyperemic surface of enlarged tonsils, first limited at the mouths of the lacunae, and then more and more widely covering the tonsil of islands of yellowish-white plaque. Sometimes individual areas of plaque merge and cover a larger or smaller part of the tonsil, without going beyond its limits. Plaque is easily removed without damaging the epithelial layer. During the period of plaque separation, on days 2–5, the severity of symptoms most often decreases, but the temperature usually remains low-grade until the inflammatory reaction in the regional lymph nodes subsides. The duration of the disease is 5–7 days; in case of complications, it can be delayed for a longer period.
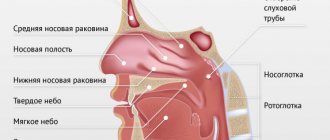
In addition to the palatine tonsils, acute inflammation may also involve other accumulations of lymphadenoid tissue, in particular those located in the nasopharynx (retronasal tonsillitis - adenoiditis, tubular tonsillitis), at the root of the tongue (lingual tonsillitis or tonsillitis IV of the tonsil). Sometimes the inflammation is diffuse, spreading throughout the lymphadenoid pharyngeal ring.
Acute inflammation of the pharyngeal tonsil (adenoiditis) is characterized by: sore throat, radiating to the deep parts of the nose, difficulty nasal breathing. The disease occurs mainly in pediatric practice.
Damage to the lingual tonsil is accompanied by pain when swallowing and when protruding the tongue. Inflammation, spreading to connective and intermuscular tissue, can lead to interstitial purulent inflammation of the tongue.
What helps with sore throat
It all depends on its cause.
For bacterial inflammation of the tonsils, doctors prescribe antibiotics. Only they can relieve a sore throat and reduce the risk of complications1,2,3,4,5. For a viral infection, antibiotics are useless.
To determine the type of sore throat, the doctor conducts a bacteriological study and analysis for beta-hemolytic streptococcus2, since it is the most dangerous representative of the bacterial pathogens of sore throat.
To alleviate the condition of sore throat caused by viruses, symptomatic treatment is sufficient: antipyretics and local therapy aimed at combating inflammation and reducing sore throat1,2.
HEXORAL® preparations may be recommended as a symptomatic remedy.
To irrigate the throat with a sore throat, you can use HEXORAL®8 spray. The broad-spectrum antiseptic hexetidine, which is part of the drug, is active against most bacteria, herpes simplex viruses type 1, influenza A, PC virus that affects the respiratory tract, and fungi, and provides a mild analgesic effect.
HEXORAL® in the form of a spray is convenient to use because it allows you to evenly spray the drug onto the entire mucous membrane of the tonsils and pharynx8. HEXORAL® solution can be used for traditional gargling9.
Lozenges HEXORAL® TABS, HEXORAL® TABS CLASSIC and HEXORAL® TABS EXTRA10,11,12 also help fight infection and sore throat during sore throat.
- HEXORAL®TABS with a neutral mint taste, based on the antiseptic chlorhexidine and the anesthetic benzocaine, can be suitable for both adults and children over 4 years of age10.
- HEXORAL®TABS CLASSIC for adults and children over 6 years old, contains a combination of antiseptics (amylmetacresol and 2,4-dichlorobenzyl alcohol), available in orange, black currant, lemon and honey with lemon flavors11.
- HEXORAL®TABS EXTRA, in addition to the antiseptic component, contains the anesthetic lidocaine, which can relieve even severe sore throat. The drug can be used by adults and children from 12 years of age.
Up to contents
The information in this article is for reference only and does not replace professional advice from a doctor. To make a diagnosis and prescribe treatment, consult a qualified specialist.
Complications of sore throat
Patients with angina may experience the following local complications: peritonsillitis and peritonsillar abscess, otitis media, etc. They usually occur in people whose treatment was started relatively late - after the 3rd day from the moment of illness. Peritonsillitis and paratonsillar abscess have similar symptoms, which include: high fever, predominance of unilateral pain in the oropharynx, sharply intensifying when swallowing, increased salivation, trismus and pain when opening the mouth, unilateral edema, hyperemia of the soft palate, swelling of the palatine arch on the affected side, and also a shift to the center of the affected tonsil and asymmetry of the uvula.
In addition to local complications, angina can cause metatonsillar diseases - rheumatism, infectious-allergic myocarditis and polyarthritis, cholecystocholangitis. With modern approaches to the treatment of patients with tonsillitis, rheumatism and polyarthritis, it is more often possible to avoid other metatonsillar diseases (for example, glomerulonephritis in 0.8% with primary tonsillitis and in 3.0% with a recurrent form of the disease).
Myocarditis develops with primary angina in the first days of the convalescence period, and with repeated angina - from the first days of the disease. This complication rarely manifests itself with the classic symptoms of this disease. Most often, the only signs of myocarditis are persistent changes in the electrocardiogram, indicating focal damage to the heart muscle, and a moderate increase in the 1st-2nd fractions of lactate dehydrogenase.
The development of glomerulonephritis corresponds to the time of formation of autoimmune (against kidney tissue) and immunopathological factors on the 5–6th day of normal body temperature (8–10th day of the disease). Glomerulonephritis occurs without extrarenal symptoms. Its only manifestation is persistent urinary syndrome in the form of moderate proteinuria (0.033–0.099 g/l), leukocyturia (10–50 cells per field of view in a urine sediment specimen), erythrocyturia (3–20 cells per field of view) and cylindruria .
Treatment of sore throats
Treatment of vulgar tonsillitis.
The rational treatment of sore throats is based on adherence to a certain gentle regimen, local and general therapy. Bed rest is mandatory in the first days of the disease, and then at home without physical activity. Prescribe a non-irritating, soft, nutritious diet, mainly vegetable and dairy, vitamins, and drinking plenty of fluids is beneficial.
Patients with angina, regardless of the severity of the condition and the period of the disease (even after the fever subsides), require antibacterial treatment to prevent the subsequent development of the described metatonsillar diseases.
GABHS are highly sensitive to penicillins and cephalosporins. β-lactams remain the only class of antibiotics to which GABHS has not developed resistance. The main problem is resistance to macrolides, which in Russia is 13–17%. At the same time, the M-resistance phenotype, characterized by resistance to macrolides and sensitivity to lincosamides (lincomycin and clindamycin), has become widespread. Resistance to tetracyclines and sulfonamides of GABHS in Russia exceeds 60%. In addition, tetracyclines, sulfonamides, co-trimoxazole do not provide eradication of the pathogen, and therefore they should not be used for the treatment of acute streptococcal tonsillitis caused even by strains sensitive to them in vitro.
Given the high sensitivity of GABHS to b-lactams, the first-line (drug of choice) for the treatment of acute streptococcal tonsillitis is penicillin (phenoxymethylpenicillin). More reliable, due to the possible resistance of the pathogen, is the use of amoxicillin clavulanate and sulbactam. Oral cephalosporins are rarely used. In patients allergic to b-lactams, macrolides or lincosamides should be used. Recommended medications, doses and dosage regimens are presented below.
Antibacterial therapy for acute streptococcal tonsillitis
Penicillins
- amoxicillin 750 mg in 3 doses 10
- amoxicillin/clavulanate 625 mg in 3 divided doses 10
- amoxicillin/sulbactam
Cephalosporins
- Cefadroxil 30 mg/kg in 1 dose 10
Macrolides (prescribed
for β-lactam intolerance)
- azithromycin 12 mg/kg in 1 dose 5
- Clarithromycin 15 mg/kg in 2 divided doses 10
- midecamycin 50 mg/kg in 2 divided doses 10
- roxithromycin 5 mg/kg in 2 divided doses 10
- spiramycin 3 million units in 2 doses 10
Lincosamides (prescribed
with intolerance to β-lactams and macrolides)
- lincomycin 30 mg/kg in 3 doses 10
- clindamycin 20 mg/kg in 3 divided doses 10
In severe cases of the disease, the patient is treated in an infectious diseases hospital. Here it is rational to use parenteral administration of an antibiotic. To prevent candidiasis on an individual basis, it is necessary to prescribe antifungal drugs. It is also advisable to prescribe a hyposensitizing drug (diphenhydramine, chloropyramine, mebhydrolin, loratadine, etc.).
In addition to general therapy, rinsing (slightly warm) with a solution of furacillin, miramistin, calendula tincture, and chamomile decoction is prescribed locally; apply a warm compress to the submandibular area. During febrile periods, drinking plenty of fluids is recommended.
Antipyretics (paracetamol-containing: paracetamol, ketaprofen, ibuprofen, etc.) are indicated at a body temperature of 38°C and above.
In the acute period of the disease and in the first days of normal body temperature, bed rest is necessary, then semi-bed rest and home rest (until the 7th day of normal body temperature). At this time, taking multivitamins is indicated.
Health indicators after a sore throat are normal body temperature for 5 days, absence of sore throat and pain on palpation of the maxillary lymph nodes, normal blood tests, urine tests and electrocardiogram.
- Atypical tonsillitis should first of all include Simanovsky-Versan tonsillitis (ulcerative-necrotic), as well as tonsillitis that occurs with systemic blood diseases and leukemia, herpetic and fungal tonsillitis.
- Treatment of ulcerative-necrotic sore throat of Simanovsky-Vincent (symbiosis of the spindle-shaped rod (B. fusiformis) and spirochete (Spirochaeta buccalis) of the oral cavity) is carried out by an otolaryngologist and consists of lubricating the ulcerated mucous membrane of the pharynx with a 10% solution of novarsenol in glycerin , 2% solution of methylene blue, 1% solution of boric acid, 10% solution of copper sulfate. Gargling with a 0.1% solution of ethacridine lactate, 0.1% solution of potassium permanganate. In severe cases of the disease, amoxicillin clavulanate (625 mg x 3 times) and intravenous infusion of novarsenol (0.3–0.4 g at intervals of 1–2 days) are recommended.
- Treatment of patients suffering from secondary acute tonsillitis due to infectious diseases is carried out in an infectious diseases hospital. Etiotropic and pathogenetic therapy is used. Disinfecting rinses are used locally.
- Treatment of patients with secondary acute tonsillitis due to diseases of the blood system is carried out in a therapeutic or specialized hematology department according to the rules for the treatment of the underlying disease.
- Fungal tonsillitis (pharyngomycosis) occurs mainly in young children and is caused by yeast-like fungi of the genus Candida albicans in 95% and Leptotryx buccalis in 5%.
Treatment of mycotic tonsillitis should be comprehensive. It includes oral use of antifungal antibiotics for 10–14 days (levorin, nystatin, decalinium chloride, mycoheptin, amphoglucamine B, ketoconazole, fluconazole), ascorbic acid, antihistamines and B vitamins. Rinses and inhalations are prescribed locally. For inhalation use amphotericin B, sodium salt of levorin, fluconazole, for rinsing - an aqueous solution of 3% boric acid, gramicidin 1:10000, potassium permanganate 1:10000, 1% quinosol.
How to treat sore throat in an adult?
Treatment of angina symptoms in adults and children includes measures to combat infection, eliminate symptoms of the disease, and prevent recurrences.
In the acute period, it is recommended to adhere to bed rest. It is forbidden to consume cold drinks and foods that irritate the mucous membranes. A gentle diet speeds up recovery and reduces signs of local inflammation. Walking is allowed only in the absence of fever, if the weather is good - no wind, rain, or severe frost. It is necessary to frequently ventilate the room, carry out wet cleaning, and drink as much as possible.
Local treatment with antiseptic and anti-inflammatory drugs helps to quickly get rid of pain, reduce signs of inflammation, and improve overall well-being. For example, in the process of washing the tonsils with antiseptic solutions, the pus is washed away and signs of inflammation are reduced. If a bacterial pathogen is identified (in particular, BSGA), antibacterial drugs can be used. But you shouldn’t prescribe them to yourself. Uncontrolled self-use of antibiotics can lead to disruption of microflora and suppression of the immune system, which causes severe complications of the disease. In extreme cases, surgical intervention is resorted to. Hypertrophied tissues are removed, thereby ridding the body of the source of chronic infection.
Do not forget about the importance of local immunity. He must always be ready to repel the attack of viruses and bacteria. To support local immunity for preventive purposes, adults and adolescents over 14 years of age use Imudon® 6 tablets per day for 20 days. The tablets dissolve, and it is not recommended to eat or drink for about an hour after using the drug6.
Instructions
More details
1 - Kochetkov P. A. Angina and acute pharyngitis / P. A. Kochetkov, A. S. Lopatin // Practical Pulmonology.. - 2005. - No. 3. - 8-14 p. 2 - Varlamov R. K. Angina. Symptoms, treatment and features of the course of the disease / R. K. Varlamov // Integration processes in science in modern conditions. Collection of articles of the International Scientific and Practical Conference. – 2016. – 120-123 p. 3 — Kunelskaya N. L. Angina: diagnosis and treatment / N. L. Kunelskaya, A. B. Turovsky, Yu. S. Kudryavtseva // Medical Affairs. – 2010. – No. 3. – 1-9 s. 4 - Pyshny D.V. Angina and tonsillopharyngitis: differences, prevention, treatment / D.V. Pyshny // New pharmacy. Pharmacy assortment. – 2008. – No. 2. – 7-11 p. 5 — Nikolaevskaya V. P. Chronic tonsillitis. Etiology, pathogenesis, clinic // Medicine. – Moscow, 1989. 6 — Instructions for medical use of the drug Imudon® lozenges dated 07/02/2018 The material was developed with the support of Abbott in order to increase patient awareness of their health status. The information in the material is not a substitute for healthcare advice. Contact your doctor. RUIMD191614 dated 06/26/2019.
Prevention of sore throat
In addition to general restorative therapy and measures aimed at preventing infection, preparations of bacterial origin, in particular complexes of antigens - lysates, the most common causative agents of inflammatory diseases of the upper respiratory tract, oral cavity and pharynx, have proven to be an effective means of preventing exacerbations in various forms of pharyngitis and recurrent tonsillitis. It is possible to use similar drugs with systemic action, but this group of drugs has a greater number of contraindications.
It should be noted that all patients suffering from chronic tonsillitis who have had more than 2 sore throats over the past 3 years are subject to mandatory follow-up in group D3, that is, 2 times a year.