Reading time: 6 min. 15 sec.
Oophoritis is an inflammatory disease of the ovaries. It rarely develops independently: as a rule, inflammation appears against the background of chronic pathologies of the genitourinary system. The inflammatory process spreads along an ascending path to nearby organs, which can lead to disruption of their functioning.
MedEx offers a modern approach to the treatment of gynecological diseases. We employ highly qualified doctors, including candidates and doctors of medical sciences. They draw up a personal comprehensive treatment plan for everyone, know how to speak the same language with the patient and devote enough time to detailed explanations.
How the disease develops
The vagina is a favorable environment for pathogenic microorganisms. If an infection gets on its mucous membrane, it encounters natural defense mechanisms. At normal levels of acidity and lactobacilli concentration, the activity of pathogenic and opportunistic microorganisms is suppressed.
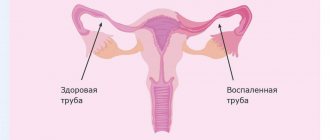
But if the immune defense is weakened, infectious agents begin to multiply and spread throughout the body. An inflammatory process occurs, which from the vagina enters the fallopian tubes and leads to the accumulation of pus. The shape and length of the fallopian tubes change: they become longer and thicker.
Excess pus may leak from the tubes, causing partial dissolution of the ovarian tissue. One or both of these paired organs become infected. Inflammation of the ovaries develops, which can spread even further - to nearby tissues and organs of the abdominal cavity.
Causes
The cause of oophoritis is most often a pyogenic infection. It is caused by aerobic or anaerobic microorganisms, including:
- mycoplasma;
- E. coli;
- chlamydia;
- Trichomonas;
- streptococci;
- staphylococci;
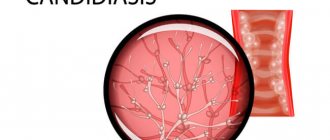
- fungi of the genus Candida.
Pathogenic and opportunistic microflora can be suppressed by the immune defense of the female body. But there are factors that weaken the immune system and increase the risk of developing the disease - excessive physical activity, psycho-emotional stress, general hypothermia, insufficiently fortified and balanced diet. The likelihood of developing inflammation increases with various hormonal disorders, the presence of an intrauterine device, and chronic infectious diseases.
Oophoritis develops when tissue integrity is disrupted. The inflammatory process often occurs in women after childbirth, abortion and other surgical interventions. Inflicted microtraumas reduce the body's natural defenses against infection.
Oophoritis may be associated with acute appendicitis. Often nearby organs are also involved in the pathological process: if the inflammation spreads to the ovaries and fallopian tubes, salpingoophoritis is diagnosed.
Consequences and complications
Among the complications of this disease it is worth highlighting:
- Hormonal imbalance. The most common luteal phase deficiency is progesterone and shortening of the luteal phase.
- Transition to chronic oophoritis, the complication of which is progesterone deficiency and chronic anovulation, which is accompanied by anovulatory uterine bleeding and the risk of ovarian malignancies.
- Miscarriage.
- Chronic pelvic pain.
- Purulent-inflammatory formations (tubo-ovarian tumor, ovarian abscesses, pyosalpings). Inflammatory tubo-ovarian "tumor" presents as enlarged and painful appendages that resemble a tumor. The spread of infection goes from bottom to top: endometritis (after abortion, intrauterine interventions, from intrauterine devices) - purulent salpingitis - oophoritis. Ovarian abscesses (pyovarium) are formed from cystic formations; often microabscesses merge with each other, forming a single abscess.
- Pelvioperitonitis (inflammation of the pelvic peritoneum) when the infection enters the peritoneal cavity through the tubes. According to the nature of the inflammation, the process can be serous-fibrous and purulent. The latter is very difficult and is characterized by the appearance of pus in the pouch of Douglas (the depression of the peritoneum between the rectum and the uterus) with the formation of abscesses.
- Ectopic pregnancy.
- Tubal infertility.
Kinds
Depending on the nature of the disease, the following forms are distinguished:
- Acute oophoritis. This form of the disease is characterized by severe symptoms. The patient's general body temperature rises, pathological discharge mixed with pus and blood appears. Pain is felt during sexual intercourse; pain occurs in the lower abdomen, spreading to the lower back and sacrum.
- Subacute oophoritis. An intermediate form between acute and chronic oophoritis. As a rule, it develops as a secondary inflammatory process. The source of inflammation in the subacute form of the disease is another disease - helminthic infestation, fungal infection, tuberculosis.
- Chronic oophoritis. Develops against the background of acute oophoritis in the absence of timely and adequate treatment. It can also be a complication of urethritis, cystitis, appendicitis. Exacerbations of oophoritis occur after hypothermia or weakened immunity: the menstrual cycle is disrupted, and the woman quickly gets tired.
The inflammatory process can affect both ovaries simultaneously: in this case, bilateral oophoritis is diagnosed. If only one of the ovaries is affected, a diagnosis of right-sided or left-sided oophoritis is made.
The prevalence of the inflammatory process may be associated with the source of infection. For example, right-sided oophoritis often develops with appendicitis. The bilateral form of the disease is usually associated with infection of the ovaries through the bloodstream or lymph.
Depending on the type of pathogen, specific and nonspecific oophoritis are distinguished. The first type of disease includes inflammation resulting from vaginal penetration of infectious agents - fungi, chlamydia, trichomonas, herpes. Oophoritis is called nonspecific if the inflammatory process develops due to imbalances in the internal bacterial microflora.
A rare form of the disease is autoimmune oophoritis. It occurs as a result of a genetic defect in the presence of provoking factors - injuries, chronic inflammatory processes, endometritis, adnexitis, salpingitis. Autoimmune oophoritis is more common in patients over 30 years of age who have had genital infections and invasive medical interventions.
Pathogenesis
Typically, oophoritis (usually salpingoophoritis) develops as an ascending infection from the vagina or uterus due to infection during sexual intercourse or complicated abortions and childbirth. In response to the introduction of the pathogen, an inflammatory reaction of the body occurs.
When the ovaries are involved in the process, their epithelium and adjacent peritoneum are first infected ( periophoritis ). Then inflammation covers the cortical layer of the ovary (actually oophoritis). In the ovary, microcirculation is disrupted, tissue damage occurs, and swelling occurs due to inflammatory effusion. Multiple follicular cysts of varying diameters form inside the enlarged ovary, as in polycystic ovary syndrome. Unlike polycystic disease, in this case there is no thickening of the stroma.
Proliferation is the final phase of inflammation and the number of connective tissue cells in the lesion increases and the number of T and B lymphocytes increases. Connective tissue cells can differentiate into fibroblasts, which produce rough fibrous tissue that replaces normal ovarian tissue. As a result of this, it loses its function.
Sometimes ulcers form in the cavity of the follicle or small cysts, which, merging, form an ovarian abscess , which is considered as a complication of oophoritis. Infectious factors are a prerequisite for the development of autoimmune oophoritis with its characteristic decrease in hormonal function.
The chronic inflammatory process is the breeding ground for the human papillomavirus, cancer and precancerous processes, since local immunity decreases.
Symptoms of oophoritis
Signs of oophoritis vary depending on the stage of the disease, the location of inflammation and the nature of the pathological process. At an early stage, symptoms are often blurred or mild. Symptoms characteristic of most infections of the reproductive system may appear - pain in the lower abdomen, pathological discharge from the vagina with a foamy or purulent consistency.
Acute oophoritis is accompanied by an increase in body temperature to 37.5-39 degrees, as well as nausea, vomiting and sharp pain in the iliac region. After this, temporary relief may occur: the condition improves, body temperature decreases. The reason is not recovery: these are signs of chronic oophoritis.
Symptoms vary depending on the location of the inflammation. Bilateral oophoritis can be recognized by enlargement of the uterine appendages and painful sensations on palpation. In the place of accumulation of pus, slight compactions are observed.
A characteristic sign of left-sided oophoritis is pain localized in the left iliac region. Sometimes it radiates to the lumbar region. Right-sided oophoritis is accompanied by pain on the right side.
Also observed:
- increased frequency of urination, discomfort and burning when emptying the bladder;
- menstrual irregularities;
- the appearance of uterine bleeding and pathological discharge between menstruation;
- painful sensations during sexual intercourse;
- deterioration in general health.
Acute oophoritis, as well as exacerbation of the chronic form of the disease, significantly reduces the patient’s quality of life. A woman develops neurological disorders, sleep disturbances, and loss of sexual desire.
Important!
The information provided on the site is for reference only. If you feel unwell or notice one or more alarming symptoms, consult a doctor.
Modern aspects of the treatment of inflammatory diseases of the pelvic organs in women
Inflammatory diseases of the pelvic organs are characterized by various manifestations, depending on the level of damage and the strength of the inflammatory reaction. The disease develops when a pathogen (enterococci, bacteroides, chlamydia, mycoplasma, ureaplasma, trichomonas) penetrates into the genital tract and in the presence of favorable conditions for its development and reproduction. These conditions occur in the postpartum or post-abortion period, during menstruation, during various intrauterine manipulations (introduction of intrauterine contraceptives (IUC), hysteroscopy, hysterosalpingography, diagnostic curettage) [1, 5].
Existing natural protective mechanisms, such as anatomical features, local immunity, the acidic environment of the vagina, the absence of endocrine disorders or serious extragenital diseases, can in the vast majority of cases prevent the development of genital infection.
In response to the invasion of a particular microorganism, an inflammatory response occurs, which, based on the latest concepts of the development of the septic process, is usually called a “systemic inflammatory response” [16, 17, 18].
Endometritis
Acute endometritis always requires antibacterial therapy. The basal layer of the endometrium is affected by the inflammatory process due to the invasion of specific or nonspecific pathogens. Endometrial protective mechanisms, congenital or acquired, such as T-lymphocytes and other elements of cellular immunity, are directly related to the action of sex hormones, especially estradiol, act in conjunction with the macrophage population and protect the body from damaging factors. With the onset of menstruation, this barrier on a large surface of the mucous membrane disappears, which makes it possible to become infected. Another source of protection in the uterus is the infiltration of the underlying tissues with polymorphonuclear leukocytes and the rich blood supply of the uterus, which promotes adequate perfusion of the organ with blood and nonspecific humoral protective elements contained in its serum: transferrin, lysozyme, opsonins [16].
The inflammatory process can spread to the muscle layer, and metroendometritis and metrothrombophlebitis occur with a severe clinical course. The inflammatory reaction is characterized by a disorder of microcirculation in the affected tissues, expressed by exudation; with the addition of anaerobic flora, necrotic destruction of the myometrium can occur [12].
Clinical manifestations of acute endometritis are characterized already on the 3rd–4th day after infection by an increase in body temperature, tachycardia, leukocytosis with a band shift, and an increase in the erythrocyte sedimentation rate (ESR). Moderate enlargement of the uterus is accompanied by pain, especially along its ribs (along the blood and lymphatic vessels). Purulent-bloody discharge appears. The acute stage of endometritis lasts 8–10 days and requires quite serious treatment. With proper treatment, the process ends, less often it turns into a subacute and chronic form, and even less often, with independent and indiscriminate antibiotic therapy, endometritis can take a milder abortive course [5, 12].
Treatment of acute endometritis, regardless of the severity of its manifestations, begins with antibacterial infusion, desensitizing and restorative therapy.
Antibiotics are best prescribed taking into account the sensitivity of the pathogen to them; the dose and duration of antibiotic use are determined by the severity of the disease. Due to the threat of anaerobic infection, additional use of metronidazole is recommended. Given the very rapid course of endometritis, the preferred antibiotics are cephalosporins with aminoglycosides and metronidazole. For example, cefamandole (or cefuroxime, cefotaxime) 1.0–2.0 g 3–4 times a day intramuscularly or intravenously drip + gentamicin 80 mg 3 times a day intramuscularly + metronidazole 100 ml intravenously drip.
Instead of cephalosporins, you can use semi-synthetic penicillins (for abortive cases), for example, ampicillin 1.0 g 6 times a day. The duration of such combined antibacterial therapy depends on the clinic and laboratory response, but not less than 7–10 days.
To prevent dysbacteriosis, from the first days of antibiotic treatment, nystatin 250,000 units 4 times a day or fluconazole 50 mg per day for 1–2 weeks orally or intravenously is used [5].
Detoxification infusion therapy may include the administration of infusion agents, for example: Ringer's solution - 500 ml, polyionic solutions - 400 ml, 5% glucose solution - 500 ml, 10% calcium chloride solution - 10 ml, unithiol with 5% ascorbic acid solution, 5 ml 3 times a day. In the presence of hypoproteinemia, it is advisable to carry out infusions of protein solutions (albumin), blood replacement solutions, plasma, red blood cells, and amino acid preparations [12].
Physiotherapeutic treatment occupies one of the leading places in the treatment of acute endometritis. It not only reduces the inflammatory process in the endometrium, but also stimulates ovarian function. When normalizing the temperature reaction, it is advisable to prescribe low-intensity ultrasound, inductothermy with a high-frequency or ultra-high frequency (UHF) electromagnetic field, magnetic therapy, and laser therapy.
- Nonsteroidal anti-inflammatory drugs (have anti-inflammatory, analgesic effects):
– paracetamol + ibuprofen 1-2 tablets 3 times a day – 10 days;– diclofenac rectally in suppositories or orally 50 mg 2 times a day – 10–15 days;
– indomethacin rectally in suppositories or orally, 50 mg 2 times a day – 10–15 days;
– naproxen 500 mg 2 times a day rectally in suppositories or orally – 10–15 days.
- Preparations of recombinant interferons (have an immunomodulatory, antiviral effect, enhance the effect of antibiotics): interferon a-2b or interferon a 500,000 IU 2 times a day rectally in suppositories - 10 days.
- Interferon inducers (have immunomodulatory, antiviral effects):
– methylglucamine acridone acetate 250 mg intramuscularly every other day – 10 days;– sodium oxodihydroacridinyl acetate 250 mg intramuscularly every other day for 10 days.
is recommended .
- Combined enzyme preparation (has anti-inflammatory, trophic effect): Wobenzym 3-5 tablets 3 times a day.
- Homeopathic remedies (have an anti-inflammatory effect, in combination with other drugs normalizes ovarian function): gynecohel 10 drops 3 times a day.
- Traditional methods of therapy: physiotherapy, herbal medicine, hirudotherapy, acupuncture, physical therapy.
- Methods of gravitational blood surgery: plasmapheresis, endovascular laser irradiation of blood (ELBI), ultraviolet irradiation of blood, intravenous administration of ozonized 0.9% sodium chloride solution.
- Combined oral contraceptives (medium-, low-dose, monophasic) 1 tablet per day - from the 5th to the 25th day of the cycle for 3-6 months:
– ethinyl estradiol 30 mcg + levonorgestrel 150 mcg (rigevidon);– ethinyl estradiol 35 mcg + norgestimate 250 mcg (Sileste);
– ethinyl estradiol 30 mcg + gestodene 75 mcg (femoden);
– ethinyl estradiol 30 mcg + desogestrel 150 mcg (Marvelon).
Additional treatment on menstrual days includes the following.
Tetracyclines (have a wide spectrum of action: gram-positive cocci, spore-forming bacteria, non-spore-forming bacteria, gram-negative cocci and bacilli, chlamydia, mycoplasma): doxycycline 100 mg 2 times a day.
Macrolides (active against gram-positive cocci, gram-negative bacteria, gardnerella, chlamydia, mycoplasmas, ureaplasmas):
– azithromycin 500 mg 2 times a day;
– roxithromycin 150 mg 2 times a day;
– clarithromycin 250 mg 2 times a day.
Fluoroquinolones (active against all gram-positive and gram-negative bacteria): ciprofloxacin 500 mg 2 times a day; ofloxacin - 800 mg once a day for 10-14 days.
Nitroimidazole derivatives (active against anaerobes, protozoa): metronidazole 500 mg 4 times a day.
Antifungal agents (active against fungi of the genus Candida):
– nystatin 250,000 units 4 times a day;
– natamycin 100 mg 4 times a day;
– fluconazole – 150 mg once.
Acute salpingoophoritis
It is one of the most common diseases of inflammatory etiology in women. Every fifth woman who has suffered salpingo-oophoritis is at risk of infertility. Adnexitis can cause a high risk of ectopic pregnancy and pathological course of pregnancy and childbirth. The fallopian tubes are the first to be affected, and the inflammatory process can involve all layers of the mucous membrane of one or both tubes, but more often catarrhal inflammation of the mucous membrane of the tube occurs - endosalpingitis. Inflammatory exudate, accumulating in the tube, often flows through the ampullary opening into the abdominal cavity, adhesions form around the tube, and the abdominal opening of the tube closes. A saccular tumor develops in the form of a hydrosalpinx with transparent serous contents or in the form of a pyosalpinx with purulent contents. Subsequently, the serous exudate of the hydrosalpinx resolves as a result of treatment, and the purulent pyosalpinx can perforate into the abdominal cavity. The purulent process can involve wider areas of the pelvis, spreading to all nearby organs [9, 10, 13].
Inflammation of the ovaries (oophoritis) as a primary disease is rare; infection occurs in the area of the ruptured follicle, since the rest of the ovarian tissue is well protected by the covering germinal epithelium. In the acute stage, swelling and small cell infiltration are observed. Sometimes, in the cavity of the follicle of the corpus luteum or small follicular cysts, ulcers and microabscesses form, which, merging, form an ovarian abscess or pyovarium. In practice, it is impossible to diagnose an isolated inflammatory process in the ovary, and this is not necessary. Currently, only 25–30% of patients with acute adnexitis have a pronounced picture of inflammation; the remaining patients experience a transition to a chronic form, when therapy is stopped after a rapid subsidence of inflammation.
Acute salpingoophoritis is also treated with antibiotics (preferably third generation fluoroquinolones - ciprofloxacin, ofloxacin, pefloxacin), as it is often accompanied by pelvioperitonitis - inflammation of the pelvic peritoneum.
For mild forms, the following is prescribed.
1. Antibacterial therapy orally for 5–7 days.
- A combination of penicillins and b-lactamase inhibitors (have a wide spectrum of action (staphylococci, Escherichia coli, Proteus, Klebsiella, Shigella, gonococcus, bacteroides, salmonella): amoxicillin + clavulanic acid 625 mg 3 times a day.
- Tetracyclines (have a wide spectrum of action: gram-positive cocci, spore-forming bacteria, non-spore-forming bacteria, gram-negative cocci and bacilli, chlamydia, mycoplasma): doxycycline 100 mg 2 times a day.
- Macrolides (active against gram-positive cocci, gram-negative bacteria, gardnerella, chlamydia, mycoplasmas, ureaplasmas):
– azithromycin 500 mg 2 times a day;– roxithromycin 150 mg 2 times a day;
– clarithromycin 250 mg 2 times a day.
- Fluoroquinolones (active against all gram-positive and gram-negative bacteria):
– ciprofloxacin 500 mg 2 times a day;– ofloxacin – 800 mg once a day – 10–14 days.
2. Oral nitroimidazole derivatives (active against anaerobes, protozoa):
– metronidazole 500 mg 3 times a day;
– ornidazole 500 mg 3 times a day.
3. Oral antifungals (active against Candida fungi):
– nystatin 500,000 units 4 times a day;
– natamycin 100 mg 4 times a day;
– fluconazole – 150 mg once.
4. Oral antihistamines (prevent the development of allergic reactions):
– fexofenadine 180 mg 1 time per day;
– chloropyramine 25 mg 2 times a day.
Additional treatments include the following.
- Nonsteroidal anti-inflammatory drugs (have anti-inflammatory, analgesic effects):
– paracetamol + ibuprofen 1-2 tablets 3 times a day;– diclofenac or indomethacin rectally in suppositories or orally, 50 mg 2 times a day – 10–15 days;
– naproxen 500 mg 2 times a day rectally in suppositories or orally – 10–15 days.
- Preparations of recombinant interferons (have an immunomodulatory, antiviral effect): interferon α-2β or interferon α 500,000 IU 2 times a day in suppositories for 10 days.
- Multivitamin preparations with antioxidant effects: Vitrum, Centrum, Duovit, Supradin, 1 tablet for 1 month.
In severe cases, the following groups of drugs are prescribed.
1. Antibacterial therapy orally for 7–10 days. During antibacterial therapy, the clinical effectiveness of the drug combination is assessed after 3 days, and if necessary, drugs are changed after 5–7 days.
- Cephalosporins of the III, IV generations (active against gram-negative bacteria, staphylococci): cefotaxime, ceftriaxone, cefepime 0.5–1 g 2 times a day intravenously.
- A combination of penicillins and β-lactamase inhibitors (has a wide spectrum of action: staphylococci, Escherichia coli, Proteus, Klebsiella, Shigella, gonococcus, bacteroides, salmonella): amoxicillin + clavulanic acid 1.2 g 3 times a day intravenously.
- Fluoroquinolones (active against all gram-positive and gram-negative bacteria):
– ciprofloxacin 1000 mg once a day;– pefloxacin, ofloxacin 200 mg 2 times a day intravenously.
- Aminoglycosides (have a wide spectrum of action: gram-positive cocci, gram-negative aerobes):
– gentamicin 240 mg 1 time per day intravenously;– amikacin 500 mg 2 times a day intravenously.
- Carbapenems (active against gram-positive and gram-negative aerobes and anaerobes): imipenem/cilastatin or meropenem 500–1000 mg 2–3 times daily intravenously.
- Lincosamides (active against gram-positive aerobes and gram-negative anaerobes): lincomycin 600 mg 3 times a day intravenously.
2. Antifungal agents (active against fungi of the genus Candida): fluconazole 150 mg once orally.
3. Nitroimidazole derivatives (active against anaerobes, protozoa): metronidazole 500 mg 2 times a day intravenously.
4. Colloidal, crystalloid solutions (intravenous drip):
– rheopolyglucin 400 ml;
– reogluman 400 ml;
– glucose 5% solution 400 ml.
5. Vitamins and vitamin-like substances (have an antioxidant effect). Intravenous stream or drip in 0.9% sodium chloride solution:
– ascorbic acid 5% solution 5 ml;
– cocarboxylase 100 mg.
Additional treatments include the following.
- Human immunoglobulins - normal human immunoglobulin (contains immunoglobulin G, complements antibacterial therapy for severe infections), intravenously at a dose of 0.2–0.8 g/kg body weight.
- Preparations of recombinant interferons (have an antiviral, immunomodulatory effect, enhance the effect of antibiotics): interferon α-2β 500,000 IU 2 times a day rectally in suppositories - 10 days.
- Interferon inducers (have antiviral, immunomodulatory effects):
– methylglucamine acridone acetate 250 mg intramuscularly every other day – 10 days;– sodium oxodihydroacridinyl acetate 250 mg intramuscularly every other day for 10 days.
- Methods of gravitational blood surgery (have detoxification, immunostimulating, antimicrobial, antiviral effects): plasmapheresis, intravenous administration of ozonated 0.9% sodium chloride solution.
- Laparoscopy, inspection and sanitation of the pelvic cavity, rinsing the pelvic cavity with ozonated 0.9% sodium chloride solution.
Treatment for chronic salpingoophoritis includes the following.
- Nonsteroidal anti-inflammatory drugs (have anti-inflammatory, analgesic effects):
– paracetamol + ibuprofen 1-2 tablets 3 times a day after meals – 10 days;- diclofenac or indomethacin rectally in suppositories or orally 50 mg 2 times a day - 10-15 days;
– naproxen 500 mg 2 times a day rectally in suppositories or orally – 10–15 days.
- Preparations of recombinant interferons (have an immunomodulatory, antiviral effect, enhance the effect of antibiotics): interferon α-2β or interferon α 500,000 IU 2 times a day rectally in suppositories (10 days).
- Interferon inducers (have an immunomodulatory, antiviral effect): methylglucamine acridone acetate or sodium oxodihydroacridinyl acetate 250 mg intramuscularly every other day - 10 days.
Additional treatment is recommended.
- Combined enzyme preparation (has anti-inflammatory, trophic effect): Wobenzym 3-5 tablets 3 times a day.
- Traditional methods of therapy: physiotherapy, herbal medicine, hirudotherapy, acupuncture, physical therapy.
- Methods of gravitational blood surgery: plasmapheresis, ELBI, ultraviolet irradiation of blood, intravenous administration of ozonized 0.9% sodium chloride solution.
- Combined oral contraceptives (medium-, low-dose, monophasic) 1 tablet per day - from the 5th to the 25th day of the cycle for 3-6 months:
– ethinyl estradiol 30 mcg + levonorgestrel 150 mcg (rigevidon)– ethinyl estradiol 35 mcg + norgestimate 250 mcg (Sileste).
– ethinyl estradiol 30 mcg + gestodene 75 mcg (femoden)
– ethinyl estradiol 30 mcg + desogestrel 150 mcg (Marvelon).
Low-dose oral contraceptive drugs normalize the function of the hypothalamic-pituitary-ovarian system. With long-term use, monitoring of hemostasis and liver function is necessary.
- Homeopathic remedies (have an anti-inflammatory effect, in combination with other drugs normalize ovarian function): gynecohel 10 drops 3 times a day.
Pelvioperitonitis
Inflammation of the pelvic peritoneum most often occurs secondary to the penetration of infection into the abdominal cavity from an infected uterus (with endometritis, infected abortion, ascending gonorrhea), from the fallopian tubes, ovaries, from the intestines, with appendicitis, especially with its pelvic location. In this case, an inflammatory reaction of the peritoneum is observed with the formation of serous, serous-purulent or purulent effusion. The condition of patients with moderate pelvioperitonitis, the temperature rises, the pulse quickens, but the function of the cardiovascular system is slightly impaired. With pelvioperitonitis, the intestine remains unbloated, palpation of the upper half of the abdominal organs is painless, and symptoms of peritoneal irritation are determined only above the pubis and in the iliac regions. However, patients note severe pain in the lower abdomen, there may be retention of stool and gas, and sometimes vomiting. The level of leukocytes is increased, the leukocyte formula shifts to the left, the ESR is accelerated. Gradually increasing intoxication worsens the condition of patients [14, 15].
Treatment of salpingoophoritis with or without pelvioperitonitis begins with a mandatory examination of the patient for flora and sensitivity to antibiotics. The most important thing is to determine the etiology of inflammation. Today, benzylpenicillin is widely used for the treatment of specific gonorrheal process, although drugs such as ceftriaxone, perazone, ceftazidime are preferable.
The “gold standard” in the treatment of salpingoophoritis from antibiotic therapy is the administration of cefotaxime at a dose of 1.0–2.0 g 2–4 times a day intramuscularly or 1 dose - 2.0 g intravenously in combination with gentamicin 80 mg 3 times a day (Gentamicin can be administered once at a dose of 160 mg intramuscularly). It is imperative to combine these drugs with intravenous administration of metronidazole 100 ml 1-3 times a day. The course of antibiotic treatment should be carried out for at least 5–7 days and you can vary mainly the basic drug by prescribing cephalosporins of the second and third generation (cefamandole, cefuroxime, ceftriaxone, perazone, ceftazidime and others at a dose of 2–4 g per day) [14].
If standard antibiotic therapy is ineffective, ciprofloxacin is used at a dosage of 500 mg 2 times a day for 7–10 days.
In case of acute inflammation of the uterine appendages, complicated by pelvioperitonitis, oral administration of antibiotics is possible only after the main course, and only if the need arises. As a rule, there is no such need, and the persistence of previous clinical symptoms may indicate the progression of inflammation and a possible suppurative process.
Detoxification therapy is mainly carried out with crystalloid and detoxification solutions in an amount of 2–2.5 liters with the inclusion of solutions of rheopolyglucin, Ringer, polyionic solutions - acessol, etc. Antioxidant therapy is carried out with a solution of unithiol 5.0 ml with a 5% solution of ascorbic acid 3 times a day intravenously [14].
In order to normalize the rheological and coagulation properties of blood and improve microcirculation, acetylsalicylic acid 0.25 g/day is used for 7–10 days, as well as intravenous administration of rheopolyglucin 200 ml (2–3 times per course). Subsequently, a whole complex of resorption therapy and physiotherapeutic treatment is used (calcium gluconate, autohemotherapy, sodium thiosulfate, humisol, plasmol, aloe, fiBS) [3, 15]. Physiotherapeutic procedures for acute processes include ultrasound, which provides analgesic, desensitizing, fibrolytic effects, increased metabolic processes and tissue trophism, inductothermy, UHF therapy, magnetotherapy, laser therapy, and subsequently, sanatorium-resort treatment.
Purulent tubo-ovarian formations
Among 20–25% of inpatients with inflammatory diseases of the uterine appendages, 5–9% develop purulent complications requiring surgical interventions [9, 13].
The following features regarding the formation of purulent tubo-ovarian abscesses can be highlighted:
- chronic salpingitis in patients with tubo-ovarian abscesses is observed in 100% of cases and precedes them;
- the spread of infection occurs predominantly through the intracanalicular route from endometritis (with IUD, abortion, intrauterine interventions) to purulent salpingitis and oophoritis;
- there is a frequent combination of cystic transformations in the ovaries with chronic salpingitis;
- there is a mandatory combination of ovarian abscesses with exacerbation of purulent salpingitis;
- Ovarian abscesses (pyovarium) are formed mainly from cystic formations, often microabscesses merge with each other.
The following morphological forms of purulent tubo-ovarian formations are found:
- pyosalpinx - predominant lesion of the fallopian tube;
- pyovarium - predominant damage to the ovary;
- tubo-ovarian tumor.
All other combinations are complications of these processes and can occur:
- without perforation;
- with perforation of ulcers;
- with pelvioperitonitis;
- with peritonitis (limited, diffuse, serous, purulent);
- with pelvic abscess;
- with parametritis (posterior, anterior, lateral);
- with secondary lesions of adjacent organs (sigmoiditis, secondary appendicitis, omentitis, interintestinal abscesses with the formation of fistulas).
Clinically differentiating each of these localizations is practically impossible and impractical, since the treatment is fundamentally the same - antibacterial therapy occupies a leading place both in the use of the most active antibiotics and in the duration of their use. In purulent processes, the consequences of the inflammatory reaction in tissues are often irreversible. Irreversibility is due to morphological changes, their depth and severity. Severe renal dysfunction is common [3, 9].
Conservative treatment of irreversible changes in the uterine appendages is unpromising, since if it is carried out, it creates the preconditions for the occurrence of new relapses and aggravation of impaired metabolic processes in patients, increases the risk of upcoming surgery in terms of damage to adjacent organs and the inability to perform the required volume of surgery [9].
Purulent tubo-ovarian formations are a difficult diagnostic and clinical process. Nevertheless, characteristic syndromes can be identified.
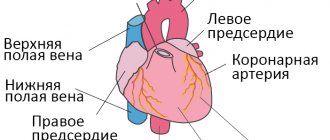
- Clinically, intoxication syndrome manifests itself in the phenomena of intoxication encephalopathy, headaches, heaviness in the head and severity of the general condition. Dyspeptic disorders (dry mouth, nausea, vomiting), tachycardia, and sometimes hypertension (or hypotension during the onset of septic shock, which is one of its early symptoms, along with cyanosis and facial hyperemia against the background of severe pallor) are noted [4].
- Pain syndrome is present in almost all patients and is of increasing nature, accompanied by a deterioration in general condition and well-being, there is pain during a special examination and symptoms of irritation of the peritoneum around the palpable formation. Pulsating increasing pain, persistent fever with a body temperature above 38°C, tenesmus, loose stools, lack of clear contours of the tumor, ineffectiveness of treatment - all this indicates the threat of perforation or its presence, which is an absolute indication for urgent surgical treatment.
- The infectious syndrome is present in all patients, manifested in most of them by high body temperature (38°C and above), tachycardia corresponds to fever, as well as an increase in leukocytosis, ESR and leukocyte index of intoxication increase, the number of lymphocytes decreases, and the shift of the leukocyte formula to the left increases , the number of molecules of average mass increases, reflecting increasing intoxication.
- Kidney function often suffers due to impaired urine passage.
- Metabolic disorders manifest themselves in dysproteinemia, acidosis, electrolyte disturbances, and changes in the antioxidant system.
The treatment strategy for this group of patients is based on organ-preserving operations, but with radical removal of the main source of infection. Therefore, for each specific patient, both the time of the operation and the choice of its volume should be optimal. Clarifying the diagnosis sometimes takes several days, especially when differentiating it from an oncological process. Antibacterial therapy is required at each stage of treatment [1, 2].
Preoperative therapy and preparation for surgery include:
- antibiotics (use cefoperazone 2.0 g/day, ceftazidime 2.0–4.0 g/day, cefazolin 2.0 g/day, amoxicillin + clavulanic acid 1.2 g intravenous drip once a day, clindamycin 2.0 –4.0 g/day, etc.). They must be combined with gentamicin 80 mg intramuscularly 3 times a day and metronidazole infusion 100 ml intravenously 3 times;
- detoxification therapy with infusion correction of volemic and metabolic disorders;
- mandatory assessment of the effectiveness of treatment based on the dynamics of body temperature, peritoneal symptoms, general condition and blood counts.
The surgical stage also includes ongoing antibacterial therapy. It is especially advisable to administer one daily dose of antibiotics on the operating table, immediately after the end of the operation. This concentration is necessary and creates a barrier to further spread of infection, since penetration into the area of inflammation is no longer prevented by dense purulent capsules of tubo-ovarian abscesses. β-lactam antibiotics (cefoperazone, ceftriaxone, ceftazidime, cefotaxime, imipinem/cilastatin, amoxicillin + clavulanic acid) pass these barriers well.
Postoperative therapy includes continuation of antibacterial therapy with the same antibiotics in combination with antiprotozoal, antimycotic drugs and uroseptics. The course of treatment is prescribed in accordance with the clinical picture and laboratory data; it should not be stopped earlier than 7–10 days. Infusion therapy should be aimed at combating hypovolemia, intoxication and metabolic disorders. Normalization of gastrointestinal motility (intestinal stimulation, hyperbaric oxygenation, hemosorption or plasmapheresis, enzymes, epidural blockade, gastric lavage, etc.) is very important. Hepatotropic, restorative, antianemic therapy is combined with immunostimulating therapy (ultraviolet irradiation, laser irradiation of blood, immunocorrectors) [2, 9, 11].
All patients who have undergone surgery for purulent tubo-ovarian abscesses require post-hospital rehabilitation in order to restore organ function and prevention.
Literature
- Abramchenko V.V., Kostyuchek D.F., Perfileva G.N. Purulent-septic infection in obstetric and gynecological practice. St. Petersburg, 1994. 137 p.
- Bashmakova M. A., Korkhov V. V. Antibiotics in obstetrics and perinatology. M., 1996. P. 6.
- Bondarev N. E. Optimization of diagnosis and treatment of mixed sexually transmitted diseases in gynecological practice: abstract. dis. ...cand. honey. Sci. St. Petersburg, 1997. 20 p.
- Ventsela R.P. Nosocomial infections. M., 1990. 656 p.
- Gurtovoy B. L., Serov V. N., Makatsaria A. D. Purulent-septic diseases in obstetrics. M., 1981. 256 p.
- Keith L. G., Berger G. S., Edelman D. A. Reproductive health. T. 2: Rare infections. M., 1988. 416 p.
- Krasnopolsky V.I., Kulakov V.I. Surgical treatment of inflammatory diseases of the uterine appendages. M., 1984. 234 p.
- Korkhov V.V., Safronova M.M. Modern approaches to the treatment of inflammatory diseases of the vulva and vagina. M., 1995. P. 7–8.
- Kumerle X. P., Brendel K. Clinical pharmacology during pregnancy / ed. X. P. Kumerle, K. Brendel: trans. from English: in 2 volumes. M., 1987. T. 2. 352 p.
- Serov V.N., Strizhakov A.N., Markin S.A. Practical obstetrics: a guide for doctors. M., 1989. 512 p.
- Serov V.N., Zharov E.V., Makatsariya A.D. Obstetric peritonitis: Diagnosis, clinic, treatment. M., 1997. 250 p.
- Strizhakov A. N., Podzolkova N. M. Purulent inflammatory diseases of the uterine appendages. M., 1996. 245 p.
- Khadzhieva E. D. Peritonitis after cesarean section: textbook. allowance. St. Petersburg, 1997. 28 p.
- Sahm DE The role of automation and molecular technology in antimicrobial susceptibility testing // Clin. Microb. And Inf.1997. 3; 2: 37–56.
- Snuth CB, Noble V, Bensch R et al. Bacterial flora of the vagina during the mensternal cycle // Ann. Intern.Med. 1982: 948–951.
- Tenover FC Norel and emerging mechanisms of antimicrobial resistance in nosocomial pathogens // Am. J. Med. 1991; 91: 76–81.
V. N. Kuzmin , Doctor of Medical Sciences, Professor MGMSU, Moscow
Diagnostic methods
Diagnosis of oophoritis begins with manual examination, palpation and medical history. It is important to find out the presence of acute or chronic infections, injuries and invasive interventions in the anamnesis.
Then diagnostic procedures and laboratory tests are prescribed:
- general blood analysis;
- general urine analysis;
- bacterial culture;
- polymerase chain reaction;
- linked immunosorbent assay.
If there is a primary infection not related to the genitourinary system, you may need to consult a doctor of related specialization.
To make an accurate diagnosis, the patient is prescribed an ultrasound of the pelvic organs: the study allows one to visualize structural changes and determine the localization of the inflammatory process. For a thorough examination of the uterus and appendages, laparoscopy is performed.
Acute and chronic oophoritis: risk factors
In a woman's body, the uterine appendages are located in such a way that the reproductive organs are well protected. However, some factors can increase the risk of developing an inflammatory process. These include:
- inflammatory diseases of the female reproductive organs. A woman’s history of vulvitis (inflammation of the external genitalia), colpitis (inflammation of the vagina), cervicitis (inflammatory process affecting the cervix), endometritis (inflammation of the mucous membrane of the reproductive organ) significantly increases the risk of ovarian inflammation. Pathogenic or conditionally pathogenic flora can penetrate the uterine appendages by ascending, lymphogenous or hematogenous routes, causing oophoritis, salpingitis or their combined form - salpingoophoritis;
- inflammatory processes in the abdominal cavity. Acute appendicitis and peritonitis can serve as a trigger for the development of inflammatory processes in a woman’s ovaries;
- invasive interventions in the uterine cavity (for example, fractional diagnostic curettage, abortion by curettage of the uterine cavity, placement of intrauterine devices). Surgical intervention can cause infectious and inflammatory processes in the pelvic organs. This is why competent and safe contraception is so important, which will not only help regulate your reproductive function and avoid abortions, but also prevent the transmission of infection during sexual intercourse;
- surgical interventions on the abdominal and pelvic cavity organs, performed through a laparotomy approach (an incision on the anterior abdominal wall). Laparoscopy, during which access is made through punctures with a diameter of about 1 centimeter, carries a lower risk of infection;
After surgical interventions, it is worth carrying out rehabilitation therapy both with medication and using modern methods of physiotherapeutic treatment.
For diagnoses such as acute or chronic oophoritis, treatment should begin as quickly as possible. Timely therapy reduces the risk of pathology becoming chronic and also reduces the incidence of relapse. This will avoid the development of severe adhesions in the pelvic organs.
Treatment of oophoritis
Ovarian oophoritis is a disease, at the first signs of which you need to consult a gynecologist. You should not try to treat inflammation on your own. This may negatively affect subsequent diagnosis and increases the risk of complications.
Acute oophoritis is treated in a clinic or hospital. The patient is recommended bed rest and symptomatic medications to relieve spasms and pain. The bacterial form of the disease is treated with antibiotics and sulfonamides, selected individually. In the acute period, restorative therapy is also carried out: the patient is given antihistamines and vitamin-mineral complexes.
When treating ovarian oophoritis in subacute form, physiotherapy is allowed. The complex may include magnetic therapy, therapeutic massage, electrophoresis, mud therapy and other procedures.
When treating chronic oophoritis, it is important not only to eliminate the symptoms of the disease, but also to understand its root cause. If the disease develops as a result of a sexually transmitted infection, both partners should be treated. During the period of recovery from illness, sexual intercourse is contraindicated.
Expert opinion
The consequences of oophoritis can negatively affect the condition of the female reproductive system. The fact is that normally the fallopian tubes are lined with ciliated epithelium, which facilitates the advancement of the egg into the uterus. The inflammatory process makes it difficult for the egg to move or completely blocks it. There is a risk of ectopic pregnancy.
Even cured oophoritis can prevent a woman from becoming pregnant. To avoid complications, it is important to start treating the disease at an early stage. If a woman finds out about the presence of inflammatory processes while she is already pregnant, she needs to discuss further actions with her doctor. The high risk of ectopic pregnancy threatens not only the ability to bear and give birth, but also the life of the expectant mother.
List of sources
- Abramchenko V.V., Bashmakova M.A., Korkhov V.V. Antibiotics in obstetrics and gynecology. – St. Petersburg: Spetslit, 2000.– 220 p.
- Rational pharmacotherapy in obstetrics and gynecology // Guide for practitioners, edited by V.I. Kulakova, V.N. Serova, M., “Litterra”, 2005, pp. 724–727.
- Serov V.N., Tikhomirov A.L. Modern principles of treatment of inflammatory diseases of the female genital organs. Toolkit. M., 2002.
- Prilepskaya V.N. Features of infectious processes of the lower genital tract. Possibilities of therapy with drugs for local use // Gynecology. 2000; 2 (2): pp. 57–59.
- Abramchenko V.V., Kostyuchek D.F., Perfileva G.N. Purulent-septic infection in obstetric and gynecological practice. St. Petersburg, 1994. 137 p.
Prevention
Prevention of oophoritis consists of following the rules of personal hygiene and regular visits to the gynecologist. It is necessary to avoid casual sex and use barrier contraceptives. When diseases of the reproductive system are detected, they must be treated under the supervision of a specialist.
Measures to strengthen the body's natural defenses are important. To reduce the risk of infection, you need to adhere to a healthy lifestyle, eat right, and engage in moderate physical activity. This significantly reduces the risk of developing genitourinary diseases.