Features of menstrual disorders in different age groups
Adolescence
In girls during puberty, menstruation may be irregular, the length of the cycle may vary, and so will the volume and nature of the discharge. At the beginning of establishing a cycle, such instability is acceptable, but if the cycle does not become predictable for a long time, you should definitely contact a gynecologist about this problem. The optimal age for the onset of menstruation is 12-13 years. Menstruation can begin at either 11 or 15 years of age. If a 14-15 year old teenager has not yet started menstruating, this is a reason to see a doctor. During adolescence, a menstrual cycle lasting from 21 to 45 days is considered normal.
Reproductive age
During this period of a woman’s life, menstrual irregularities can be associated with the development of pathological processes, hormone intake, pregnancy, the use of antidepressants, etc. Healthy women aged 20-40 years have regular menstruation, the cycle duration is 21-35 days. The duration of menstruation for most women is from 2 to 7 days. Irregular, prolonged, painful periods are a reason to see a doctor.
Premenopause
Before the onset of menopause, the body gradually loses its reproductive function. The ovaries produce less estrogen hormones, which are responsible for the ability to become pregnant. At this age, menstruation may become less frequent or, conversely, the cycle becomes shorter, and the volume of discharge may also change. Some women continue to have periods until they are 55 years old. During this period, regardless of the onset of menopause or the continuation of menstruation, it is very important to monitor hormonal levels, the balance of vitamins and microelements, and regularly visit a gynecologist.
The most common causes of late or irregular periods
Unlike pregnancy and menopause, which naturally stop menstruation, the following causes of amenorrhea and irregular menstruation are quite undesirable and have a negative impact on our health, but they can be addressed.
Increased stress levels
If a woman experiences severe stress for a long time, her body begins to conserve energy without ovulating. If a woman experiences a sudden traumatic event, this can cause increased stress on the adrenal glands, which leads to a cessation of production of estrogen and other reproductive hormones (a condition called hypothalamic amenorrhea). When a woman does not have enough estrogen, she will not be able to maintain the uterine mucosa in a normal state, resulting in a delay in menstruation.
Why is this happening? Your body reacts to emergency situations. Convenience is very good, and reproductive function is very important, but still, from the point of view of survival, they are secondary. Our innate natural survival mechanism involves the constant production of vital stress hormones, otherwise known as the “fight or flight” response, such as cortisol and adrenaline. Adrenaline and cortisol are two main hormones responsible for the body’s response to stress, helping us escape from threats (whether real, sudden or imaginary threats). These hormones are vital and sometimes very useful because they help us run, climb, give us strength, make us sweat and regulate our heart rate, but too much of them can lead to health problems.
The body has always given priority to the production of stress hormones that help to survive critical situations, considering sex hormones to be secondary during periods it considers difficult. With chronic stress, there is a lack of useful substances, such as amino acids that contribute to the normal functioning of neurotransmitters, and there are not enough of them to produce enough hormones, so the body has to choose between stress hormones and sex hormones, and preference is always given to the first. Under conditions of severe stress, such as dieting, strenuous exercise, or emotionally charged events, all such situations can trigger amenorrhea with or without weight loss.
Poor nutrition
Foods low in nutrients, antioxidants and probiotics, but high in stimulants, can place increased stress on the thyroid and adrenal glands. For example, cortisol levels may increase if the following factors are present:
- high consumption of sugar, hydrogenated fats and artificial additives or pesticides;
- problems with the thyroid gland;
- adrenaline fatigue.
Elevated cortisol levels interfere with the optimal production of many other important hormones, including sex hormones. If elevated cortisol levels persist for a long time, this can lead to problems with the skin, damage to bone and muscle tissue, as well as brain tissue. This cycle of elevated cortisol can lead to protein deficiency, resulting in muscle loss and osteoporosis.
If you have problems with menstruation, check how healthy you are eating. You should choose foods that are high in antioxidants and nutrients, especially those high in fat (even saturated fat, which may be good for your situation) and protein. You can also use high-calorie food supplements if you are underweight, have a lack of fatty tissue, or are actively involved in sports.
Excessive weight loss and low weight
When your body mass index (BMI) drops below 18-19, your period may be delayed due to too little fat tissue. Body fat is important for producing enough estrogen, which is why women who are too thin or have serious illnesses such as anorexia and bulimia may experience absent or delayed periods. Increased physical activity and therefore higher nutrient requirements due to intense exercise can sometimes lead to weight loss and put you at risk of developing hormonal imbalances.
Low-calorie, low-fat foods can also cause nutritional deficiencies and loss of fat tissue and contribute to irregular periods and bone loss. Some evidence suggests that very thin vegan women, including those who eat only raw, uncooked foods, and non-meat vegetarians, are also at risk, most likely because they are more likely to be underweight and lack vital nutrients. useful substances.
Increased physical activity
While moderate exercise is important for heart health, mood control, sleep, and maintaining a stable body weight, increased physical activity places increased stress on the adrenal, thyroid, and pituitary glands. Therefore, women who suddenly begin intense physical training, such as training for a marathon or similar important event that requires high physical excretion, may suddenly stop menstruating.
Like other stress hormones, cortisol surges in response to any real or anticipated stress. The latter can be physical (including sports) or emotional. Such stress factors include overwork and physical exhaustion from increased physical activity, which may be accompanied by lack of sleep, constant rush, infectious diseases and emotional exhaustion. Nowadays, with the constant desire to be thin and maintain good physical shape, some women believe that they need to exercise intensely, they think that sweating a lot is healthy, and so they tire themselves out constantly.
Such physical overload can increase stress and deprive the body of the energy it needs to regulate sex hormones. Thus, one report from the University of Michigan reported that running and ballet are among the physical activities where the largest number of women suffering from amenorrhea are found. Almost 66% of women who participate in long-distance running or ballet dancing experience amenorrhea at some point in their lives. The situation is even worse for women involved in bodybuilding. Almost 81% of them suffer from amenorrhea from time to time, while they eat a diet low in nutrients.
“Exercise-induced amenorrhea” may indicate general exhaustion of the body, decreased vitality, and is more common in young girls. Thus, the number of women participating in athletics in childhood and adolescence has increased by 800% over the past 30 years, while at the same time the number of people suffering from hormonal imbalances has increased. Other problems that often accompany amenorrhea include decreased bone density and eating disorders. Therefore, doctors are concerned about the vulnerability of this category of patients to heart complications, bone problems and nutritional deficiencies.
Thyroid disorders
You may not even realize that the thyroid gland may be causing hormonal imbalances.
According to recent studies, problems with the thyroid gland are one of the main causes of delayed menstruation; almost 15% of patients with amenorrhea suffer from abnormalities in the functioning of the thyroid gland.
The thyroid gland, considered the main regulatory mechanism of the endocrine system, is responsible for metabolism and influences many sex hormones.
Problems with the thyroid gland, including underfunctioning or endemic goiter and hyperfunction, can cause a wide range of health problems, such as changes in estrogen and cortisol levels, and delayed menstruation. Increased cortisol levels can lead to general hormonal insensitivity, including thyroid insensitivity. This means that the body becomes desensitised to estrogen and cortisol, which can cause their increased production.
Stopping the use of oral hormonal drugs
Some women deliberately interrupt their menstrual cycle to prevent pregnancy, but when they stop taking birth control pills, their periods do not start. Although some doctors say that periods should return to normal within a few months of stopping hormonal pills, many women experience delayed or irregular periods for several years afterward.
A woman's natural menstrual cycle consists of rising and falling levels of estrogen and progesterone, but taking birth control pills keeps estrogen levels high enough that it confuses the body into feeling like you're pregnant, thus causing your menstrual cycle to go awry. It takes the body many months and even years to correct this situation and restore homeostasis.
Thus, a report published in one of the American journals dedicated to obstetrics and gynecology reports that about 29% of women suffer from a delay in menstruation for more than three months after using contraceptives. Hence our advice: stop using contraceptives if there are signs of menstrual irregularities.
Chronic hormonal imbalance and other hormonal disorders
Polycystic ovary syndrome (PCOS) is a hormone imbalance in women that negatively affects ovulation. When a woman suffers from polycystic ovary syndrome, it means that her levels of hormones, including estrogen, progesterone and testosterone, are disrupted, which can manifest itself in different ways:
- abnormal hair growth on the body or face;
- problems with sugar levels;
- being overweight;
- acne;
- irregular menstrual cycle.
Polycystic ovary syndrome can be diagnosed by a gynecologist, who must check the woman's hormone levels, analyze the symptoms and check your genetic predisposition to the disease, as well as examine the ovaries and find out whether cysts are growing or not.
Also, women with polycystic disease often experience premature menopause before the age of 40, which can be accompanied not only by the absence of menstruation, but also by hot flashes, night sweats, and vaginal dryness. Although this is the most rare cause of irregular periods.
Diagnostics of NMC
On your first visit to the clinic, you talk with the doctor, show him the results of previous studies (if you have them), tell him details about your health, lifestyle, and the presence of chronic diseases. Next, the doctor conducts an examination in a gynecological chair. During the examination, a smear is taken for cytology (PAP test), flora, as well as colposcopy to obtain a complete picture of the condition of the genital organs. You will also undergo ultrasound diagnostics and donate blood. You can bring a container of urine with you to your initial appointment and submit it to the laboratory for testing on the same day.
Laboratory results will be available in a few days or a week. Once you receive all the results by email, you can schedule a follow-up consultation to receive a doctor’s opinion and prescribe a treatment plan.
What other causes of irregular periods are there?
Also, the cause of NMC can be: ovulation processes (bloody discharge or spotting once, or for several days, more often in the middle of the cycle); ovarian cysts, polyps in the uterus and cervix; cervical erosions, foci of endometriosis in the uterus or on the cervix; diseases of the thyroid gland (nodules or cysts, dysfunction of the gland). In such situations, further examination of this organ, its structure and function is carried out. An ultrasound and blood test for hormones are performed.
Additional instrumental studies may be offered depending on the problem organ:
- for the cervix - examination under a microscope (colposcopy),
- hysteroscopy - examination of the uterus using an endoscopic device,
- puncture of an ovarian or thyroid cyst is possible.
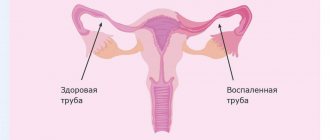
What is especially important and unsafe is NMC due to ectopic pregnancy (most often tubal). In this case, the fertilized egg, due to insufficient patency of the tube, does not descend into the uterus, but continues to grow in the tube. Your period may not come on time or may come but not as usual (scanty or heavy, long, frequent). This is the situation when it is important to contact a gynecologist in a timely manner. The most common complication of ectopic pregnancy is a rupture of the tube with bleeding into the abdominal cavity, pain, and loss of consciousness. In this case, urgent surgery is necessary for life-saving reasons.
A pregnancy test (the first thing a woman can do at home to understand the situation), a blood test for general hCG (pregnancy hormone), and a dynamic ultrasound of the pelvic organs to monitor the development of pregnancy will help you choose the right treatment tactics in a timely manner.
Any NMC requires clarification of the causes of this situation and an individual approach to examination and treatment of each woman separately.
Treatment of menstrual irregularities
The problem of NMC cannot be solved instantly - it requires detailed treatment / correction of disorders. The following can be used in the treatment of NMC:
- hormone therapy;
- uroseptic drugs;
- vitamins, microelements (dietary supplements);
- antibiotics.
Sometimes physical therapy is prescribed. And always, regardless of the cause of cycle disorders, the doctor gives recommendations on normalizing the daily routine, level of physical activity, and nutrition. A woman should minimize stress at home and at work, walk more in the fresh air, sleep in the dark in a well-ventilated area. An integrated approach to eliminating menstrual irregularities will definitely bear fruit!
In rare cases, surgical treatment is performed. It is indicated when dysmenorrhea is associated with the presence of neoplasms.
Reasons for violations
Violation of the cycle refers to polyetiological conditions, when several factors can contribute to the development: dysfunction of the hypothalamus, pituitary gland, ovaries, organic pathology of the genital organs, hemostasis disorders, blood diseases, endocrine and systemic diseases. The nature of the menstrual cycle changes against the background of organic changes in the endometrium, endometrial polyps, and endometrial cancer.
Disturbances can be transient in nature when the cause of cycle instability is due to energy and protein malnutrition, hypovitaminosis, underweight, obesity, psychological overload and acute psychological trauma, long-term use of various groups of drugs. Acyclic uterine bleeding can occur after hypothermia or unprotected sexual intercourse. After eliminating the provoking factor, the menstrual cycle, as a rule, restores itself.
Cost of treatment for menstrual irregularities
Diagnosis and treatment of menstrual cycle disorders in women at the Marina Ryabus clinic are carried out by experienced gynecologists, candidates of medical sciences. There are two specialists at your service:
- gynecologist-oncologist, surgeon Ekaterina Nikolaevna Kozlova;
- gynecologist-endocrinologist, nutritionist Irina Sergeevna Vyatkina.
Our doctors work by appointment. You can do all the necessary diagnostics (laboratory tests, ultrasound, colpososcopy, biopsy, etc.) in our clinic. Call to make an appointment.
Cost of consultations with gynecologists at the Marina Ryabus Clinic
| Doctor | Initial consultation | Repeated consultation within the designated period | Repeated consultation after the specified period |
| Vyatkina I.S. | 8 500,00 | up to 4 months – 6,000.00 | from 4 months – 8,500.00 |
| Kozlova E.N. | 5 000,00 | Up to 2 months – 4,000.00 | from 2 months – 5,000.00 |
We recommend visiting a gynecologist at least once every six months/year. If a woman is undergoing treatment, it is necessary to visit the gynecologist more often, in accordance with the plan outlined by the doctor.