Methyl alcohol (methanol, wood alcohol, carbon) is a strong biological poison and the cause of individual and mass cases of poisoning with a high percentage of deaths. Psychiatrist-narcologist Vladislav Sipovich, Chief Physician of the Multidisciplinary Medical Center, informs readers about the symptoms of methyl alcohol poisoning, first aid methods, treatment, prevention and consequences.
Definition
· Methanol (CH3OH) is a methyl monohydric alcohol, easily soluble in most liquids.
It looks no different from ethyl alcohol. · Poisoning occurs due to ingestion or inhalation of methanol (wood alcohol) vapor in quantities that cause intoxication.
· Poisoning often occurs by mistake due to use instead of ethanol or during suicide attempts.
· This is the most common type of alcohol intoxication after ethanol, with a high mortality rate.
· Can be successfully treated with an antidote, but in high doses and in the absence of medical attention it is fatal.
· CH3OH is found in propellants for cars and aircraft, and is also used in perfumes.
· Easily absorbed through the skin, by inhalation and through the intestines.
Causes of intoxication with alcohol surrogates
The main cause of poisoning with alcohol surrogates is their constant use. Some are so toxic that a single exposure to the body is enough to cause serious health problems, and if the permissible dose is exceeded, death. There are various factors that contribute to trying non-intended liquids. These are alcohol and drug addiction, bad company, family problems, bad heredity and others. Particular attention should be paid to children who may succumb to one of these factors.
Etiology and pathogenesis
Pathophysiology
· It is broken down by alcohol dehydrogenase in the liver to formaldehyde and further to formic acid, which is a harmful metabolite.
· Decomposition is slow, about twice as long as ethanol, but faster than formic acid.
· Consequently, it takes 15-20 hours for sufficient formic acid to accumulate to cause hyperventilation (compensation for acidosis) and visual impairment.
Combination of ethanol and methanol
· Both alcohols compete for the same decomposition enzyme, but ethanol has a higher affinity.
· Thus, simultaneous consumption of ethanol will have a positive effect due to the delayed formation of formic acid.
Toxicity
· The most vulnerable structures are the optic nerve and putamen (basal ganglia).
· Consumption of a critical dose causes optic atrophy and/or Parkinson's symptoms, respectively.
· The lethal dose of wood alcohol is up to 1 ml/kg, but this will depend on whether ethanol is taken at the same time.
· If CH3OH is not decomposed, it is excreted unchanged in urine and exhaled air with a half-life of up to 40 hours.
· Folic acid deficiency results in inhibited formic acid degradation.
What are the main symptoms and signs of methyl alcohol poisoning?
Methyl alcohol poisoning can be acute or chronic. Symptoms of an acute process, depending on the dose, appear within a few hours, maximum 2 days after consumption. The acute course is characterized by the following main symptoms: • Intoxication in the form of headache and dizziness, abdominal pain, nausea, vomiting, muscle pain. • Symptoms similar to alcohol intoxication - unsteady gait, confusion, psychomotor agitation, turning into drowsiness, decreased sensitivity. • Specific manifestations associated with toxic damage to the optic nerve - photophobia, dilated pupils, blurred vision. It often ends in optic nerve atrophy and complete blindness.
In severe poisoning, hyperventilation, respiratory failure, cyanosis of the skin and mucous membranes, increased and weakened pulse, a drop in blood pressure and the development of convulsions occur. Subsequently, coma and death occur due to respiratory and cardiac arrest.
Laboratory tests reveal an increased hemoglobin content in the blood, the presence of protein and casts in the urine.
Poisoning with methyl alcohol vapors is characterized by the following symptoms: • Irritation of the conjunctiva of the eyes and mucous membranes of the respiratory tract. • Weakness and headache. • A state similar to alcohol intoxication.
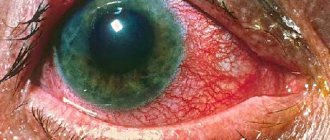
Chronic poisoning is characterized by the following symptoms: • Weakness, increased fatigue and decreased performance. • Touchiness, tearfulness, irritability. • Memory loss. • Dysfunction of the gastrointestinal tract, pain in the right hypochondrium. • Decreased visual acuity, flickering “goosebumps” before the eyes. • Dilated veins of the fundus and hyperemia of the eyeball. • Atrophic changes in the optic nerve.
Thrombocytopenia (decreased number of platelets in the blood) is detected in the laboratory.
Diagnostics
Diagnostic criteria
· The main sign of poisoning is metabolic acidosis with increased values of osmolality gap and anion gap.
· Symptoms appear late, no earlier than after 15-20 hours, hyperventilation and visual disturbances appear.
· If there is combined consumption of wood alcohol and ethanol, it may take several days after ingestion before feeling unwell.
· Other symptoms include nausea, vomiting and headache.
· In the most severe cases, blindness, coma and respiratory arrest occur.
History taking
What questions should you ask the patient:
- Amount and concentration of the substance used?
- Time aspect?
- Did the patient influence consumption by inducing vomiting or using sorbents?
- Was the person taking other pills or medications? What and how much?
- Could others ingest the same alcohol and accidentally become poisoned?
- Does the patient have chronic problems with alcohol ? Alcoholics can tolerate more methanol before poisoning.
It is worth considering that poisoning can also occur in industrial companies through absorption through the skin or inhalation.
Clinical data
· Various degrees of decreased consciousness.
· Hyperventilation. As a rule, it is first observed in the later stages.
· Possibly fluctuating abdominal pressure.
· Coma, cyanosis.
· Ophthalmoscopy: poor reaction of the pupil to light, retinal hyperemia with inflammation.
· Blurred edges of the papilla without protrusion, the so-called pseudo papillitis.
Additional Research
· Acid status/base.
· Metabolic acidosis.
· Electrolytes.
· Glucose.
· Urea.
· Serum amylase and possibly serum lipase for the development of pancreatitis.
· Determination of methanol in blood and urine.
· In cases of severe poisoning, a CT scan of the brain (possibly an MRI) may be indicated in later stages.
· Calculation of osmolal and anion gap. It has proven to be a reliable and very good diagnostic tool for methanol poisoning.
By calculating the osmolality gap and the anion gap, a diagnosis of methanol or ethylene glycol poisoning can be made with a high probability. The treatment is the same for both. Osmolality gap and anion gap are increased in methanol poisoning.
1. Early in the process, before methanol degradation has begun, the patient will have a high osmolality gap (lots of methanol) and usually anion gap (some formic acid) and slight acidosis. Such patients are usually not severe.
2. At the end of the process, when all the monohydric alcohol is decomposed, the value for the osmolality gap will be normal, while for the anion gap it will be high (lots of formic acid). These patients are often severe.
Impact on the body
The influence of surrogates on the body has primary and secondary characteristics.
all starts with arousing the body on an emotional and physical level. The eyes begin to shine and activity increases. It seems that all problems have been solved, and the attitude towards the world around us is improving. At the same time, a person’s confidence in himself and his beliefs grows, he becomes sharp and categorical. If you start arguing with him, you will notice dilated pupils and redness of the face, which are also primary effects.
Some secondary signs cannot be noticed - this is the absorption of toxins into the blood, as a result of which the functioning of the central nervous system and brain is disrupted. Stronger alcohol intoxication occurs and the person clearly expresses the state: stupidity in judgment, aggressive behavior, sexual craving and others.
As the amount of toxins the body receives increases It becomes difficult to breathe, blood vessels narrow, speech and movements become inappropriate. This condition is characterized by crawling . With increasing intoxication, a person stops responding to everything and an alcoholic coma , which in turn can lead to death.
There are the following stages of coma:
- The first is superficial . In order to bring a person to his senses, it is necessary to rinse the stomach.
- The second is of medium severity. The main symptom is relaxed muscle tone. Gastric lavage will not revive the victim; hospitalization is required.
- The third is a deep coma. There are no reflexes, no reaction to light, and convulsions may occur. Urgent medical attention is required.
A coma is most likely to occur if a person who rarely drinks alcohol takes a large dose of pure alcohol at a time.
If assistance is not provided in a timely manner, a critical condition , which will develop into death.
Therapy for methanol poisoning
Methanol poisoning is a dangerous condition that requires prompt diagnosis and treatment. The primary goal of therapy is to minimize the effect of alcohol on the body.
Generally about treatment
Treatment should begin even before a final diagnosis is made.
· Gastric lavage. It is indicated if <2 hours have passed since administration.
· Correction of acidosis. It is performed with sodium bicarbonate and is initially most important along with supporting vital functions such as breathing and circulation.
· Inhibition of alcohol dehydrogenase with ethanol or the antidote fomepizole.
· Removal of methanol and formic acid by hemodialysis. This is most often done in parallel.
Antidote for methanol poisoning
At the moment, there are 2 known antidotes for wood alcohol intoxication - ethanol and fomepizole.
Ethanol
The most accessible of the antidotes, but it has both advantages and some disadvantages for use.
Benefits of ethanol treatment:
· Low price.
· Easy access.
· Good and fast effect.
Quantity:
· The effect of ethanol on methanol degradation depends on the molar concentration between them. A lot of methanol requires a lot of ethanol and vice versa.
· For practical reasons, a therapeutic ethanol concentration of 1 g/L (22 mmol/L) is usually recommended.
Minuses:
· It has been found difficult to maintain adequate ethanol concentrations in patients, especially during concurrent dialysis. There are simple formulas for determining the amount of ethanol in various situations, and ethanol can also be added to the dialysate fluid.
· Other disadvantages of ethanol treatment are that it becomes increasingly difficult for the patient to cope with it.
· In some cases, the ethanol supply may be what makes the patient a respiratory candidate.
Treatment regimen:
1. If methanol > 0.2 g/L or acidosis, ethanol is given as a 10% solution, such as 50 mg/ml glucose solution (remove 50 ml from the 500 ml infusion bag and replace with 50 ml ethanol).
2. Start with a dose of 0.6 g/kg body weight (i.e. 1 ml 70% sterile alcohol/kg) over 15-20 minutes. For adults, an additional 7-10 g/h is given as an infusion.
Titers are such that plasma concentrations of about 1 are maintained for at least 48 hours or methanol can no longer be detected in the blood.
Fomepizole (4-methylpyrazole)
It is an effective alcohol dehydrogenase inhibitor without the side effects of ethanol and dosage problems. Inhibits the formation of toxic metabolites.
· The drug is used to treat poisoning with methanol and ethylene glycol.
· Treatment can be carried out without measuring serum values even during dialysis.
Fomepizole also inhibits ethanol degradation. Therefore, any supply of ethanol should be stopped when switching to fomepizole.
Advantages:
· Ensures safe dosing.
· More effective than alcohol.
· Gives few side effects.
Flaws:
· High price.
When combined with hemodialysis, the need for intensive care is significantly less, and some patients are discharged after 24 hours.
Dosage:
· The dose is diluted in 100 ml of NaCl 154 mmol/l or glucose 50 mg/ml and administered as a slow i.v. infuse for 30 minutes.
· Initial dose of 15 mg/kg followed by doses of 10 mg/kg every 12 hours 4 times.
· Later 15 mg/kg every 12 hours.
· Can also be given orally and the dosage remains the same.
· Second dose for dialysis.
Actions of doctors
The person is hospitalized. The main life-saving actions are to remove toxins from the body by lavaging the stomach. This treatment of poisoning with alcohol surrogates is indicated for 3 days. At the same time, the patient is given sorbents.
If poisoning is caused by methanol, then ethyl alcohol is administered orally or intravenously, but only in therapeutic doses and diluted. For ethylene glycol intoxication, the antidote is calcium gluconate. It neutralizes toxic substances.
Vitamin preparations, hormonal agents, glucose, novocaine and other medications are also administered intravenously, which help normalize the functioning of the body.
Subsequent treatment tactics depend on the detected disorders of the internal organs. If your kidneys have problems, a person may need hemodialysis. This procedure helps cleanse the blood and minimize the load on the kidneys. In extremely severe cases, a kidney transplant is performed.
Progress, complications and prognosis
To prevent household accidents, ensure that liquids containing methanol are kept out of the reach of children and label bottles to avoid confusion between methanol and ethanol.
Gradient
· Most often the latency is 12-24 hours before symptoms appear.
· Concomitant use of ethanol will further increase latency.
· In cases of severe poisoning, severe symptoms may occur earlier.
· The course of the patient's symptoms will often be as follows: first, mild intoxication, therefore headache, lethargy and nausea, gradually visual disturbances, diffuse abdominal pain and shortness of breath are possible.
Complications
· Decreased vision or blindness.
· Parkinsonism.
· Pancreatitis, in the worst case hemorrhagic pancreatitis.
· Seizures, cerebral edema and possibly necrosis of the basal ganglia.
· Rhabdomyolysis and acute renal failure.
· Hypoglycemia.
Forecast
1. The degree of acidosis is critical to the outcome. Without treatment, methanol poisoning leads to permanent vision damage, collapse and coma.
2. Injuries to the basal ganglia may produce a Parkinson's-like picture.
3. The dose of lethal is most often indicated at 1 g/kg body weight (30-240 ml).
4. The minimum dose that can cause visual damage is unknown.
Early and proper treatment of methanol poisoning will help prevent complications.
What kind of alcohol are they poisoning with?
In addition to alcohol, which is clearly not intended for ingestion, poisoning with so-called “scorched vodka” often occurs. It can be quite difficult to distinguish licensed and counterfeit vodka by appearance. Moreover, there are numerous cases where similar products were sold in regular stores and even supermarkets of large retail chains.
To protect against this, as well as in an attempt to save money, people are increasingly resorting to moonshine. But even here, not everything is smooth and simple. Moonshine can contain a large amount of harmful impurities in the form of fusel oils. The consequences of consuming such a “homemade” product can also be very, very serious.
In addition to “palenka” and moonshine, the leading positions in the number of cases of poisoning include medical tinctures with alcohol. Alcohol tinctures of pepper and hawthorn are especially popular. Their use as an alternative to food alcohol in any long term leads to rapid social and mental degradation.
Poisoning after food alcohol may not appear immediately and may not be in an acute form; such poisoning can be treated in the usual ways, but if the signs described below are observed, special measures must be taken.
Additional Information
Find out:
- What substances available for everyday use contain ethylene glycol, and what properties does it have? What does ethylene glycol poisoning , what symptoms does it cause and how effectively is it treated. What antidote exists for intoxication and how accessible is it for use?
- What are the common sources of fluoride poisoning and why are children at risk? What symptoms indicate intoxication, and what needs to be done at home to provide first aid if you feel unwell.
- After consuming what foods can histamine poisoning , and how dangerous this condition is.
- Due to an overdose of which drugs iron poisoning and how effectively it is treated.
- Common sources of lead intoxication , and what irreversible consequences poisoning can lead to.
- Is it possible to get intoxicated after exceeding the dose of calcium antagonists , and does this affect human health?
First aid
Most deaths from alcohol poisoning are associated with delayed medical care. If you suspect severe intoxication, you should urgently call a doctor.
Before his arrival:
- do not leave the person alone, even if he has fallen asleep or lost consciousness. If he starts to feel sick, he may choke on the vomit;
- It is better if the patient stays awake; you should not let him fall asleep;
- if he is vomiting but cannot get up, place him on his side to prevent him from choking;
- if there are no problems with swallowing, you can give a sorbent. This will reduce the absorption of alcohol from the stomach.
What not to do:
- give a person to drink alcohol, coffee, milk, etc.;
- send him under a cold or contrast shower or into the bath;
- try to induce vomiting, rinse the stomach (danger of internal bleeding);
- force him to walk, stand on his feet (it’s better to sit him down or lay him down comfortably).
In cases of alcohol poisoning, people most often die due to breathing problems. It is associated with the accumulation of vomit in the oral cavity and trachea. If a person is not breathing, is wheezing, or wheezing, the upper respiratory tract needs to be cleared. To do this, place him on his side, and remove the vomit with his fingers without pushing it deeper. If the victim is unconscious, he should lie so that the tongue does not fall into the larynx.