Experience with the use of natalizumab (Tysabri) at the Neurology Research Center
The article summarizes the experience of using natalizumab (a drug that modifies the course of multiple sclerosis), accumulated at the Scientific Center for Neurology in 2012–2014. The efficacy, safety and tolerability of natalizumab were analyzed. It is noted that natalizumab is well tolerated and appears to be effective in cases of active demyelinating process and in cases of ineffectiveness of first-line drugs that modify the course of multiple sclerosis. The need for mandatory adherence to a plan to minimize the risks of side effects of therapy is emphasized. The tactics of patient management after cessation of natalizumab treatment are considered.
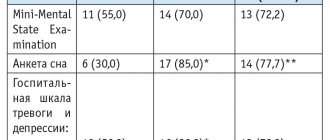
Table 1. Clinical characteristics of patients at the time of prescription of Tysabri
Table 2. Number of infusions performed at the time of drug discontinuation and at the time of detection of JCV antibodies
Table 3. Clinical data on the course of multiple sclerosis in the first year after discontinuation of Tysabri
Drawing. Sum of EDSS scores at the time of Tysabri prescription, at the time of discontinuation of therapy and one year after discontinuation of the drug (numbering of clinical cases as in Table 1)
Introduction
Multiple sclerosis is a chronic progressive demyelinating disease of the central nervous system. Multiple sclerosis affects mainly young, able-bodied and socially active people. More than half of patients with multiple sclerosis experience difficulties in performing professional duties after ten years, problems in independent movement after 15 years, and difficulties in self-care after 20 years and longer [1].
The prescription of drugs that modify the course of multiple sclerosis (DMD) pursues such goals as reducing the risk of exacerbations, stabilizing the condition, namely slowing down the rate of increase in disability and preventing transformation into a progressive course in the relapsing-remitting variant of the disease [2].
The key problem in therapy that modulates the course of multiple sclerosis is currently considered to be the development of criteria for treatment failure with the aim of timely transition to another type of therapy before the course of the pathological process leads to irreversible damage. The development of exacerbations during the first year of therapy, confirmed progression of neurological deficit according to the Expanded Disability Status Scale (EDSS), persistence or increase in the activity of the pathological process according to magnetic resonance imaging (MRI) can be regarded as a set of signs of partial or complete treatment failure [3, 4].
As the understanding of the pathogenesis of multiple sclerosis deepens, more and more “targets” for therapeutic intervention appear. Currently, such a possibility of treating multiple sclerosis as the use of monoclonal antibodies aimed at specific antigens is being actively developed [5]. Antibodies to adhesion molecules can inhibit one of the main stages of the pathogenesis of multiple sclerosis - interaction with endothelial cells and migration of lymphocytes across the blood-brain barrier. The first of these drugs to undergo clinical trials for multiple sclerosis was natalizumab, a humanized monoclonal antibody that binds to the alpha-4 subunit of alpha-4-beta-1 and alpha-4-beta-7 integrin, a component of the very late antigen integrin. 4 (VLA-4) on leukocytes. The binding of natalizumab to VLA-4 blocks its interaction with the vascular cell adhesion molecule ligand on the surface of endothelial cells of the blood-brain barrier, which reduces the migration of lymphocytes and monocytes from venules and capillaries to inflammatory foci. Natalizumab is also able to reduce the severity of the ongoing inflammatory process in the central nervous system, mediated by lymphocytes already present in the nervous tissue.
Tysabri (natalizumab) is the first monoclonal antibody drug to demonstrate efficacy in multiple sclerosis in randomized controlled trials. Thus, patients in the AFFIRM study received 300 mg of natalizumab intravenously every four weeks. While taking natalizumab, the frequency of exacerbations significantly decreased (by 68%) and the progression of disability slowed down (by 54%) compared with placebo. These changes were more typical for patients with active multiple sclerosis (81 and 64%, respectively). A decrease in the activity of the pathological process was also observed on MRI: the average number of new/enlarging lesions decreased by 83% and the number of lesions accumulating contrast agent decreased by 92%. 64% of patients had no signs of clinical activity, 57% had no signs of activity on MRI, and 37% had neither clinical nor radiological signs of activity [6].
Currently, natalizumab is recommended as monotherapy for relapsing-remitting multiple sclerosis without signs of secondary progression when first-line drugs (interferon beta, glatiramer acetate) are ineffective [3] or in cases of aggressive relapsing-remitting multiple sclerosis.
In Russia, this drug was registered in 2010 for the treatment of relapsing-remitting multiple sclerosis, and since 2011, the “Council” observational program has been carried out, the purpose of which is to assess the safety and effectiveness of natalizumab in the Russian patient population [7]. This article presents the experience of using natalizumab accumulated at the Scientific Center for Neurology in 2012–2014.
Material and methods
In the period from January 2012 to the present, the drug Tysabri was prescribed to 12 patients at the Scientific Center for Neurology who met the following criteria:
- high clinical activity of relapsing-remitting multiple sclerosis and/or high activity according to MRI (more than nine lesions accumulating contrast agent);
- ineffectiveness of first-line DMT (two or more exacerbations in the previous year).
The main clinical characteristics of the patients are presented in Table 1. An equal number of women and men (six people each) received the drug. The median age of the recruited group was 33 [28; 40] (21; 50) years*. The median duration of the disease at the time of initiation of therapy was 48 [23; 84] (6; 204) months. The median severity on the EDSS scale at the time of initiation of therapy was 3.75 [2.5; 5.5] (1.5; 6.0) points, median disease progression index (the ratio of the sum of points on the EDSS scale and the duration of the disease) – 0.09 [0.05; 0.13] (0.02; 0.6).
Among patients included in the program, 50% had previously used first-line DMTs with insufficient effectiveness. The administration of the drug Tysabri was carried out according to a standard scheme in inpatient conditions of the sixth neurological department of the Scientific Center of Neurology.
Results and its discussion
Efficacy of natalizumab
Of the 12 patients who received Tysabri, four continue therapy to date; in eight cases, Tysabri was discontinued. The duration of therapy ranged from 10 to 28 infusions.
When assessing the effectiveness of treatment, the frequency of exacerbations was primarily assessed. In the treated group, exacerbations during therapy were noted in only two patients: in one case, an exacerbation was recorded the next day after the first administration of the drug, in the other case - after the 13th infusion. These exacerbations were stopped by pulse therapy with methylprednisolone according to the standard regimen. These data indicate the high effectiveness of natalizumab in controlling the activity of the pathological process when prescribed as both the first and second line of therapy that changes the course of multiple sclerosis.
Safety and tolerability of natalizumab
When discussing the safety and tolerability of Tysabri, it should be noted that side effects of such therapy include reactions to infusion (dizziness, nausea, urticaria, chills), hypersensitivity reactions (hypotension, chest discomfort, shortness of breath, angioedema, rash, urticaria) , changes in laboratory parameters (increased levels of liver transaminases, decreased hemoglobin and red blood cells, increased number of leukocytes), infections (herpes simplex, herpes zoster), including opportunistic ones. In our observation, adverse reactions were recorded once and were regarded as reactions to the drug infusion: one patient experienced nausea and dizziness for several hours after the first infusion. Otherwise, Tysabri was well tolerated and no other side effects were noted.
As is known, one of the serious side effects of therapy is progressive multifocal leukoencephalopathy (PML). PML occurs as a result of activation of the John Cunningham virus (JCV). In this case, diffuse, steady inflammatory demyelination is noted with the formation of confluent foci in the white and gray matter of the brain. To date, PML is a potentially fatal disease. A prerequisite for prescribing Tysabri is strict adherence to a plan to minimize the risk of developing PML. If PML is suspected, treatment is recommended to be stopped immediately [8].
Risk factors for the development of PML include a history of immunosuppressive therapy, the presence of JCV antibodies, and duration of natalizumab therapy for more than two years. In the observed group, no patient had previously received mitoxantrone therapy. At the same time, JCV antibodies were detected in eight patients. The number of infusions performed in case of drug discontinuation, the number of infusions at the time of detection of JCV antibodies are presented in Table 2.
Recently, not only a qualitative analysis of the presence of JCV antibodies has been carried out, but also a quantitative determination of the antibody index, which makes it possible to assess the risk of developing PML. The index demonstrates the optical density of the sample normalized in the calibrator, which is the final measure of the antibody titer when serially diluted. For comparison, we present the following data: with an index ≤ 0.9 and a duration of therapy of 1–24 months, the risk of developing PML is 0.1 per 1000 patients, and with an index > 1.5 with a similar duration of therapy – 1.0 per 1000 patients, then there is an increase of 10 times [9].
Thus, during the use of natalizumab, it is important to evaluate JCV antibodies over time: in the studies conducted, it is recommended to pay attention to the change in the patient’s status from seronegative to seropositive. It is important to note that the use of natalizumab is not contraindicated in the presence of JCV antibodies, as this is not the only risk factor for the development of PML. About 55% of patients with multiple sclerosis are JCV seropositive [10], which is comparable to the population of healthy individuals [11].
In the observed group, in most cases, we continued Tysabri therapy, increasing the number of infusions to 12, both in the case of a negative and positive test result for JCV antibodies. In clinical case No. 6, therapy was interrupted after 10 infusions due to a high increase in the antibody index over time (from 2.8 to 3.72 over seven months). In other cases, seroconversion was also taken into account. In cases No. 9 and 10, more than 12 infusions were performed with a positive test for JCV antibodies at the time of drug prescription due to the high activity of the disease, the young age of the patients, and their desire to continue therapy with Tysabri. In these two cases, therapy was later interrupted at the request of the patients (planned pregnancy in one case and the desire to discontinue the drug without specifying the reason in the other).
Management of patients in case of discontinuation of natalizumab therapy
Finally, another extremely pressing issue today is the course of the disease, return of activity and tactics for managing patients in case of discontinuation of natalizumab therapy. Currently, optimal tactics for managing patients after natalizumab discontinuation for one reason or another are being actively developed.
The results of an analysis were published that assessed how stopping natalizumab therapy affected clinical activity (rate of exacerbations) in 1866 patients and MRI activity (number of contrast-enhancing lesions) in 341 patients with relapsing-remitting multiple sclerosis over eight months of follow-up. Both parameters of pathological process activity have been shown to increase after cessation of this therapy, reaching a peak between the fourth and seventh months. The return of disease activity does not depend on the duration of natalizumab therapy, transfer of the patient to alternative therapy, and is also observed in patients with highly active multiple sclerosis [12]. However, the phenomenon of rebound in the frequency of exacerbations or the activity of contrast-accumulating foci was not observed.
According to the results of another cohort study, in 375 patients with multiple sclerosis with high disease activity, the average frequency of exacerbations after stopping natalizumab therapy may increase, but in most patients does not reach the same values as before starting natalizumab therapy. For comparison, the rate of exacerbations before natalizumab therapy was 0.94 (95% confidence interval (CI) 0.88–1.00), during natalizumab therapy 0.47 (95% CI 0.43–0.52 ), in the first–sixth month after discontinuation of natalizumab 0.63 (95% CI 0.51–0.76), in the 7–12th month 0.55 (95% CI 0.42–0.70). In other words, the frequency of exacerbations after cessation of natalizumab therapy in the entire group did not exceed the same rate before the start of therapy. However, in 22% of patients, the course of the disease after stopping this therapy could be classified as a rebound phenomenon based on the frequency of exacerbations: the frequency of exacerbations after discontinuation of natalizumab was higher than before the start of treatment. These same patients showed a higher frequency of exacerbations during treatment with natalizumab [13].
According to a number of authors, when observing 201 patients for 12 months, withdrawal syndrome due to disease activity was observed in 11.9% of cases. At the same time, the average frequency of exacerbations before natalizumab therapy was lower and the therapeutic response was worse in those patients who subsequently experienced the rebound phenomenon, compared with patients without this phenomenon. Patients without withdrawal symptoms were also more likely to be switched to alternative therapy earlier [14].
Data on the course of multiple sclerosis in the first year after discontinuation of Tysabri in patients observed at the Scientific Center for Neurology are shown in Table 3.
In cases No. 6 and 9, frequent exacerbations after discontinuation of Tysabri required not only the administration of methylprednisolone according to the standard regimen, but also high-volume plasmapheresis due to the high total dose of methylprednisolone received (12–13 g) over the past months. It is important to note: in cases of pronounced activation of the pathological process diagnosed by MRI (in clinical cases No. 7, the exacerbations were not severe in terms of neurological deficit and responded well to treatment with glucocorticosteroid drugs. In cases No. 2 and 10, a gradual increase in neurological deficit was noted during the year of observation, which corresponds to a secondary progressive course of the disease.In the remaining two cases (No. 3 and 12), exacerbations of multiple sclerosis were not recorded (Table 2).
It is important to note: in cases of pronounced activation of the pathological process diagnosed by MRI (in clinical cases No. 7, the exacerbations were not severe in terms of neurological deficit and responded well to treatment with glucocorticosteroid drugs. In cases No. 2 and 10, a gradual increase in neurological deficit was noted during the year of observation, which corresponds to a secondary progressive course of the disease.In the remaining two cases (No. 3 and 12), exacerbations of multiple sclerosis were not recorded (Table 2).
As can be seen from the figure, during Tysabri therapy there was a decrease in the severity of the neurological deficit, and the sum of points on the EDSS scale stabilized. After cessation of therapy, the EDSS score either increased slightly (in eight patients the score increased by 0.5–1) or remained unchanged. The exception was case No. 2, when, as a result of the development of secondary progressive multiple sclerosis, the neurological deficit a year after discontinuation of Tysabri began to exceed that at the time of prescription of the drug.
To date, there have been no results from randomized studies to answer the question: “What to do after stopping natalizumab therapy?” According to a group of experts from Germany (Krankheitsbezogene Kompetenznetz Multiple Sklerose), taking a break from treatment or administering methylprednisolone once a month is not advisable, as opposed to switching to another line of therapy. An eight-week interval must be maintained before switching to fingolimod therapy, while treatment with glatiramer acetate or interferon beta can be started immediately after discontinuation of natalizumab [15].
In Italy, a comparative study of continuation of natalizumab therapy after two years (24 administrations) and discontinuation/replacement with first-line drugs was conducted. No disease rebound phenomenon was observed in patients who stopped taking natalizumab. However, in the natalizumab group, the clinical and radiological activity of multiple sclerosis was significantly lower than in those who “switched” or “discontinued” therapy. Thus, according to the literature, discontinuation of natalizumab therapy in patients with a good response to therapy should only be discussed if there is a high risk of developing PML, provided that this risk outweighs the benefit of continuing therapy [16].
Conclusion
From our own experience using Tysabri, we can draw the following conclusions. Tysabri is well tolerated and appears to be effective in cases of active demyelinating process and in cases of failure of first-line DMT. During the first two years of therapy, patients experienced seroconversion of JCV antibodies, in some patients in combination with a significant increase in the JCV antibody index, which may affect the risk of developing PML. In case of discontinuation of natalizumab therapy, clear organization of transfer of the patient to other DMTs is necessary.
The use of Tysabri is not without risks, and long-term use requires caution. When prescribing new, highly selective drugs, it is important to pay attention to minimizing risks. Assessing the risks and benefits of using a particular drug for the treatment of multiple sclerosis is a complex but necessary step in choosing a therapeutic strategy for a particular patient. Strict adherence to the risk management plan is key to the safety of therapy.
basic information
Active ingredient: natalizumab 20.0 mg/ml. Auxiliary components:
- Sodium dihydrogen phosphate monohydrate 1.13 mg/ml,
- sodium hydrogen phosphate heptahydrate 0.48 mg/ml,
- sodium chloride 8.20 mg/ml,
- polysorbate 80 (E433) 0.20 mg/ml,
- water for injection 983.00 mg/ml.
Appearance: concentrate for the preparation of a solution for infusion in the form of a colorless or slightly opalescent solution. Pharmacotherapeutic group: monoclonal antibodies. Average price for the drug Natalizumab in Russia: 90,000.00 rubles. Country of origin: USA, UK, Germany, Denmark, Belgium, Russia. A detailed description and detailed instructions for use of the drug for patients are presented below.
Mechanism of action
The active substance of the drug Tysabri (Natalizumab) is a selective inhibitor of adhesion molecules (membrane receptors that are involved in the binding of cells to other cells). The substance binds to the alpha-4 subunit of human integrin (cellular receptor). Integrin is formed in large quantities on the surface of all leukocytes, except neutrophils.
Natalizumab creates a specific binding to alpha-4-beta-1 integrin, thereby blocking the interaction with this receptor, vascular cell adhesion molecule (VCAM-1) and the osteopontin ligand, fibronectin domain, which is formed as a consequence of alternative splicing, junctional segment-1 (CS-1). Natalizumab also blocks the interaction of alpha-4-beta-7 integrin with the mucosal adhesion molecule addressin-1 (MadCAM-1). Disruption of these molecular bonds prevents the entry of leukocytes into areas of inflammation. The further mechanism of action of the drug may be due to the elimination of inflammation in the affected tissues. This occurs by inhibiting the interaction of alpha-4-expressing leukocytes with associated molecules in the extracellular space and on parenchymal cells. Using this mechanism, natalizumab can eliminate inflammation in affected tissues and prevent further entry of leukocytes into the site of inflammation.
Indications for use
The drug is indicated for monotherapy in the following patients diagnosed with multiple sclerosis.
- People whose disease continues to progress after using interferon beta. The course of interferon beta therapy should be at least one year. Tysabri is prescribed if during this time the patient has more than one relapse, more than nine foci of inflammation are visible on magnetic resonance imaging, or more than one foci that are visible when using the gadolinium contrast agent.
- Patients with severe MS that progresses rapidly. That is, people who have had more than two relapses in a year, have more than one focus of inflammation on an MRI with gadolinium, or a significant increase in the number of affected areas compared to the previous examination.
Use for renal impairment
Studies on the use of the drug for people with impaired renal function have not been conducted. Taking into account the mechanism of elimination of natalizumab and the pharmacokinetics of the substance, it can theoretically be assumed that the administration of the drug to patients with impaired renal function is permitted. There is no need to change the dose.
Use for liver dysfunction
Studies on the results of using Tysabri for people with impaired liver function have also not been conducted. Based on theoretical calculations of pharmacokinetics and the mechanism of elimination, it is assumed that the drug can be prescribed to patients with impaired liver function without changing the dose. There is a risk of liver damage throughout the course of therapy. Some people with liver disease have worsened their general condition and liver function during therapy. Therefore, patients with any abnormalities require special attention from the attending physician. Symptoms of organ damage include a bitter taste in the mouth, nausea, pain in the right hypochondrium, jaundice, problems with stool, and general malaise. If liver damage is severe, Tysabri therapy should be discontinued immediately.
Use in elderly patients
There are no data on the safety of Tysabri in people over 65 years of age. Therefore, the use of the drug for people of this age category is not recommended.
Use in children
Tysabri is contraindicated in children. Not recommended for use in adolescents.
Directions for use and doses
Treatment of MS with Tysabri must be carried out under the supervision of a physician. The attending physician must be competent in the field of neurology and specialize in diseases associated with dysfunction of the nervous system. Magnetic resonance imaging should be performed periodically throughout the course of therapy. It is better if everything necessary for treatment will be located in one medical institution. Patients should be informed about the possible risks. After two years of treatment, they should be made aware of the increased possibility of developing PML. Patients and their caregivers should also be aware of the early symptoms of progressive multifocal encephalopathy. Before the first IV is placed, you need to make sure that you have the medications that may be needed if a hypersensitivity reaction to Tysabri occurs. The diluted solution is administered intravenously using a dropper over an hour. During this time, patients must remain under medical supervision. Rapid administration of the drug is unacceptable. Before starting therapy, you need to make sure that the patient does not have immunodeficiency. After stopping suppressive medications, a person may remain immunosuppressed for some time. Treatment with Tysabri should be continued if the patient’s condition has improved within six months. Otherwise, the justification for therapy should be reconsidered. Tysabri is administered as an infusion once every four weeks. Patients should remain under the supervision of a physician for an hour after infusions.
Sequence of actions when preparing a dropper
- First of all, you should inspect the substance for the presence of any impurities. You need to make sure that the appearance of the drug corresponds to the description specified in the instructions.
- The solution for infusion is prepared under strictly sterile conditions. To do this, remove the cap, pierce the stopper and draw 15 milliliters of the substance into the syringe.
- The contents of the syringe are then added to 100 milliliters of saline.
- To mix the sodium chloride solution with tysabri, you need to turn the bottle over several times. Do not shake the bottle.
- Before connecting the dropper, be sure to once again inspect the appearance of the drug.
Contraindications
- hypersensitivity to natalizumab or any of the excipients;
— progressive multifocal leukoencephalopathy (PML);
- increased risk of infection with opportunistic microorganisms, incl. immunodeficiency conditions (for example, patients receiving or receiving immunosuppressants such as mitoxantrone or cyclophosphamide, see also section "Special instructions");
- simultaneous use of interferon beta or glatiramer acetate;
- malignant neoplasms, with the exception of basal cell skin cancer;
- children and teenagers.
Interaction with other drugs
The combination of Tysabri with other immunosuppressants has not yet been fully studied. Patients who have previously taken drugs that suppress the immune system are at increased risk of developing PML. Therefore, before prescribing Tysabri, one should wait until the immune system is restored. The doctor should carefully examine the patient to exclude the possibility of the presence of immunodeficiency. Concurrent therapy with natalizumab and anticancer drugs is also not recommended, as the likelihood of developing infections increases. Studies in people with multiple sclerosis have found that treating relapses with a short course of glucocorticosteroids does not increase the risk of developing infections. Hence the conclusion is that the combination of natalizumab with a short course of glucocorticosteroids is permitted. Combining Tysabri with any other medications is not recommended. The only exception is saline solution. In a study of sixty people with multiple sclerosis, no abnormalities in the immune response to natalizumab were reported.
Transportation and storage conditions
Tysabri natalizumab should not be frozen. The optimal temperature for storing ampoules and the finished solution is from two to eight degrees Celsius. Immediately before infusion, be sure to allow the product to warm to room temperature. After the infusion, the system should be flushed with saline solution. The ampoule is intended for single use. Tysabri should be kept out of the reach of children and in a dark place. Exposure to direct sunlight is not recommended. The concentrated substance can be stored for four years. Diluted solution – no more than eight hours. Any waste or expired products must be disposed of in the designated area.