Otolaryngologist for adults and children
Son of the gods
Stanislav Vladimirovich
Experience 26 years
Otorhinolaryngologist of the highest category, Candidate of Medical Sciences, member of the European Rhinological Society (European Rhinologic Society)
Make an appointment
The most common complication of ARVI in both children and adults is sinusitis - inflammation of the mucous membrane of one or more nasal paranasal sinuses.
- Patients complain of nasal congestion, discharge, heaviness and discomfort in the frontal or paranasal areas of the face, and body temperature often rises.
- Pain with sinusitis is often pulsating in nature, it intensifies with sudden movements and tilting of the head. The disease is not mistakenly considered dangerous, but it significantly worsens the quality of life. Without adequate treatment, sinusitis easily becomes chronic, and in some cases complications may develop that can have serious consequences.
Symptoms and signs of sinusitis
Sinusitis is one of the most common diseases. Timely diagnosis and therapy can quickly get rid of pain and other unpleasant sensations, but advanced cases are difficult to treat. It can occur in an acute form with an increase in temperature and characteristic signs, or in a sluggish form.
The following symptoms are observed with sinusitis:
- prolonged runny nose, congestion in both or one nostril, clear or greenish-yellowish discharge, sometimes with blood clots, worsening in the morning;
- a feeling of dryness that persists throughout the day;
- irritation in the larynx area in the evening and at night, causing a dry cough;
- swelling, pain, increased sensitivity in the paranasal and frontal areas;
- decreased sense of smell;
- high temperature in acute form, low-grade fever (37–37.5°) in chronic form;
- increased fatigue and irritability, decreased appetite.
Are you experiencing symptoms of sinusitis?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
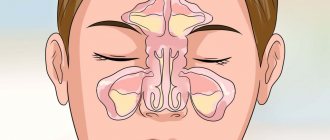
A special case of sinusitis is sinusitis, and they should not be confused. To understand the essence of the terms, you should turn to anatomy. Sinuses are air cavities in the nasal area, primarily necessary for warming and humidifying the inhaled air.
Humans have paired sinuses:
- maxillary (maxillary);
- frontal;
- ethmoid, as well as single wedge-shaped.
All of them are interconnected by channels and covered with a mucous membrane. When the inflammatory process develops, the mucous membrane swells and blocks the channels, causing the fluid to stagnate and cause discomfort. Depending on the location of the inflammation, they distinguish between sinusitis - inflammation in the maxillary sinuses, frontal sinusitis - in the frontal sinuses, ethmoiditis - in the ethmoid sinuses, sphenoiditis - in the sphenoid sinus.
Sinusitis can be left- or right-sided, as well as bilateral.
Acute sinusitis is an inflammation of the sinuses (sinuses) surrounding the nasal cavity that lasts up to 4 weeks.
It usually manifests as nasal congestion, headache, pain or tension in the face.
Most often, acute sinusitis occurs during or immediately after a cold. Less commonly, it can be caused by a bacterial or fungal infection or allergy.
In most cases, antibiotics are not required (unless symptoms of sinusitis persist for more than 7 days in adults and more than 10 days in children).
Synonyms Russian
Acute rhinosinusitis, acute sinusitis, acute sinusitis.
English synonyms
Acute sinusitis, Acute rhinosinusitis, Acute maxillary sinusitis.
Symptoms
There is no single sign by which one can accurately determine that a patient has sinusitis, so when diagnosing this disease, a doctor takes into account all the symptoms and the history of the development of the disease.
The most typical symptoms of sinusitis are:
- nasal congestion,
- headache,
- discharge from the nose, light or yellow, green in color, as well as flowing down the back wall of the throat,
- decreased sense of smell,
- pain, tension, swelling in the facial area, corresponding to the affected sinus: around the eyes, nose, forehead,
- pain in the upper jaw, teeth,
- bad breath,
- cough, especially at night,
- increase in body temperature,
- weakness.
General information about the disease
Sinusitis is an inflammation of the sinuses (sinuses) surrounding the nasal cavity. It is called acute in cases where recovery occurs no more than 30 days from the onset of the disease, subacute - when it lasts from 4 to 12 weeks. If the symptoms of the disease persist without interruption for more than 3 months, it is chronic sinusitis.
Sinusitis is very common at any time of the year, but it is more common in winter.
In fact, it is more correct to talk about rhinosinusitis (from the Greek rhinos - “nose”), since inflammation in the sinuses is always accompanied by inflammation in the nasal cavity itself, which is called rhinitis, or, more simply, a runny nose.
The paranasal sinuses are air-filled cavities in the bones of the skull that connect to the nasal cavity. They are also called paranasal sinuses.
There are 4 groups of paranasal sinuses, and according to their damage, the following types of sinusitis are distinguished:
- sinusitis - inflammation of the maxillary (maxillary) sinuses, located on the right and left sides of the nasal cavity, in the upper jaw,
- ethmoiditis - inflammation of the ethmoid sinuses located between the eyes,
- frontal sinusitis - inflammation of the frontal sinuses located above the eyes
- sphenoiditis is an inflammation of the sphenoid (main) sinus, which is located behind the nasal cavity, close to the base of the brain.
Several sinuses can be affected at the same time, but the maxillary sinuses are most often affected.
The exact function of the sinuses is unknown; it is assumed that they, among other things, are involved in warming and humidifying the inhaled air. They are covered with a mucous membrane with cilia, which produces mucus. This mucus, due to the movement of the cilia, is removed through small holes that connect the sinuses with the nasal cavity. Normally, mucus moves in only one direction, which keeps the sinuses sterile, despite the fact that the nasal cavity connected to them is inhabited by bacteria.
If the mucus exit holes are blocked or the cilia of the sinus mucosa are disrupted, the fluid stagnates and fills the sinuses, causing symptoms of sinusitis: nasal congestion, headache. The accumulation of fluid in the sinuses becomes a favorable environment for the proliferation of bacteria, which makes the disease more severe and complications can develop.
Causes of acute sinusitis
- Infection
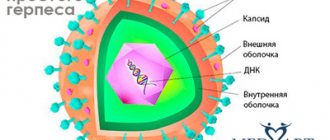
- Viral. Most often, acute sinusitis occurs during or immediately after a cold. A cold is accompanied by inflammation of the sinus mucosa in most patients, but the addition of a bacterial infection is noted in less than 1% of cases.
- Bacterial. Much less commonly, acute sinusitis is caused by bacteria. Most often they complicate viral inflammation, although they can also be the primary cause of sinusitis. Sinusitis is considered to be caused by bacterial inflammation if symptoms persist for 7 days or more in adults and 10 days or more in children.
- Fungal. Fungi can cause extremely severe, life-threatening sinusitis. People with weakened immune systems, such as HIV-infected people, are most susceptible to fungal infections.
- Allergy. Swelling of the nasal mucosa due to allergies (for example, to pollen) can block the flow of mucus from the sinuses.
- Anatomical causes, in particular a deviated nasal septum, consequences of injury, or polyps - abnormal growths of the mucous membrane inside the nose.
- Chronic heartburn.
- Chemical agents, including those contained in tobacco smoke, can impair the functioning of the cilia of the sinus mucosa.
Sinusitis can lead to the following complications.
- Meningitis. In this case, the infection spreads to the membranes of the brain.
- Abscesses inside the skull are purulent foci that cause an increase in temperature to 39-40 degrees and severe pain.
- Eye complications. When inflammation spreads to the orbital area, vision may be impaired up to complete blindness.
- Chronic sinusitis, indicated by persistence of symptoms for more than 12 weeks.
Who is at risk?
- Having a deviated nasal septum, polyps in the nasal cavity
- Suffering from allergic rhinitis.
- Suffering from chronic heartburn.
- HIV-infected and other patients with reduced immunity.
- Active and passive smokers.
Diagnostics
The diagnosis of “acute sinusitis” is made based on a study of all symptoms and the course of the disease. There are no specific signs that alone would accurately indicate sinusitis. It is important to distinguish it from the common cold, which can also present with a runny nose and nasal congestion.
Most sinusitis is caused by viruses and does not require antibiotics (as they do not treat viral infections), while bacterial sinusitis is treated with antibiotics. This is why it is important to distinguish between viral and bacterial sinusitis. In practice, however, this is extremely difficult to do, since there are no clear criteria for the addition of a bacterial infection. You need to know that thick, purulent yellow or green nasal discharge is not a sign of a bacterial infection and is often observed with the common cold, which is caused by viruses. Currently, bacterial and viral sinusitis are conventionally defined by the duration of the disease. If symptoms persist for more than 7 days in adults and more than 10-14 days in children, sinusitis is considered bacterial.
Usually no additional examination is required, but in controversial cases it can be useful in making a correct diagnosis.
Laboratory research
- General blood analysis. An increased number of leukocytes may indirectly indicate the bacterial nature of sinusitis.
- Erythrocyte sedimentation rate (ESR). It can be significantly increased with severe bacterial inflammation.
- C-reactive protein is an indicator characterizing the activity of inflammation. With sinusitis it may be elevated, but this is not specific to this disease.
- Rhinocytogram - taking a smear from the nasal cavity, followed by staining and examination under a microscope. Based on the ratio of cells in this analysis, one can judge the allergic or infectious nature of sinusitis, although the reliability of the results is not very high.
- Sowing the contents of the paranasal sinuses. In case of prolonged sinusitis or ineffectiveness of antibiotics, as well as in patients with reduced immunity, contents can be taken from the paranasal sinuses for subsequent culture on nutrient media, where bacteria multiply so that they can be recognized. The most reliable results are obtained with direct puncture of the sinus.
Other research methods
- X-ray of the skull. Allows you to identify thickening of the sinus mucosa or detect fluid in them. Currently, however, it is not recommended because its reliability in diagnosing sinusitis is quite low.
- Computed tomography (CT) of the paranasal sinuses. The most reliable way to study for sinusitis. Particularly useful in case of complications.
- Endoscopic examination of the sinuses. A thin tube is inserted into the nasal cavity to visually assess the condition of the paranasal sinuses. This method can be informative for fungal infections, tumors, polyps, and developmental abnormalities.
Treatment
A disease with moderate symptoms does not require seeing a doctor.
Most patients recover without antibiotics. Treatment in this case includes the use of vasoconstrictors (no more than 3-5 days), rinsing the nasal cavity, inhaling warm steam, warm compresses on the sinus area, painkillers, and taking a sufficient amount of fluid.
Antibiotics are generally only required for severe illness, when bacterial infection is clearly suspected, or when symptoms persist for a long time, and are usually administered for at least 10 days. In approximately 10-15% of patients they do not help, then a puncture of the sinus followed by rinsing it can be used. It may also be indicated if complications develop.
In case of severe purulent complications, operations are performed aimed at eliminating the purulent focus, simultaneously with intravenous antibiotics.
Prevention
- Avoid contact with people with colds, wash your hands before eating.
- Get an annual flu vaccination.
- Proper treatment of allergic rhinitis (incorrect treatment is, for example, uncontrolled and prolonged use of vasoconstrictor drops).
- Use a humidifier at home and ventilate the room (moisturizing the nasal passages increases the resistance of tissues to microbes).
- Do not smoke, avoid contact with tobacco smoke.
Recommended tests
- General blood analysis
- Erythrocyte sedimentation rate (ESR)
- C-reactive protein, quantitative
- Microscopic examination of a smear from the nasal mucosa
- Culture of flora with determination of sensitivity to antibiotics
Literature
- Dan L. Longo, Dennis L. Kasper, J. Larry Jameson, Anthony S. Fauci, Harrison's principles of internal medicine (18th ed.). New York: McGraw-Hill Medical Publishing Division, 2011.
Reasons for development
Most often, sinusitis in adults occurs due to a viral infection, less often due to a bacterial or fungal infection. The mucous membrane of the sinuses is covered with ciliated epithelium, which traps bacteria, viruses and dust that come with the inhaled air. Normally, mucus is quickly removed, preventing pathogens from starting their activity. But if this mechanism fails, the mucous membrane is not promptly renewed, and viruses manage to penetrate the epithelial cells. Inflammation begins, the vessels enlarge, which leads to increased permeability, and nasal discharge appears. The drainage of the sinuses is impaired, and this creates ideal conditions for a bacterial infection to join the viral one in the absence of adequate treatment. With bacterial sinusitis, nasal discharge acquires a yellowish tint, with purulent sinusitis it becomes greenish.
In addition, the disease can occur for a number of other reasons. Among them:
- adenoid vegetations (pathological enlargement of the tonsils, making nasal breathing difficult);
- allergy expressed by rhinitis;
- anomalies of the nasal septum, polyps, trauma;
- dental caries, complications after dental surgery;
- stress (psychosomatic factor).
Sinusitis can be acute (lasts less than 12 weeks, there is a high temperature and general intoxication of the body), recurrent (up to 4 cases per year) and chronic (lasts more than 12 weeks). Without proper treatment, acute sinusitis can easily turn into a chronic form with mild symptoms, during which periods of remission and relapses are observed.
Risk factors and complications
Acute sinusitis with high fever develops in people with weakened immune systems and chronic diseases. It is more severe in people who do not adhere to the principles of a healthy diet, have bad habits, in particular, smokers, do not play sports and are not hardened. The development of the disease is facilitated by such anatomical features as an enlarged nasal concha and narrowed nasal passages, which make it difficult for mucus to pass through.
Against the background of reduced immunity, a fungus can also settle in the nasal cavity, especially if it has already affected the nails or skin on the hands or feet.
Improper treatment of sinusitis leads to complications. Among them:
- infection entering the general bloodstream;
- damage to other tissues and organs located in the skull (especially dangerous for the eyes and inner ear);
- deterioration of the sense of smell, up to its complete disappearance.
To prevent the development of complications, you should avoid self-medication and strictly follow your doctor’s recommendations. Purulent discharge is of particular concern.
Treatment of rhinosinusitis
The main goals of treating rhinosinusitis in adults are to relieve inflammation, restore normal drainage and natural ventilation of the paranasal sinuses, eliminate the cause of inflammation, and restore normal viscosity of nasal secretions.
Antibacterial therapy
Antibacterial therapy for rhinosinusitis is prescribed only by a doctor and only when diagnostics have shown that it is really necessary. Viral diseases cannot be treated with antibiotics. If there are indications for antibacterial treatment, the doctor most often prescribes broad-spectrum antibiotics.
As a rule, an analysis to identify the causative agent of infection is not indicated, since inflammation is caused by microorganisms that are well known to doctors. But if antibacterial treatment turns out to be ineffective, the pathogen is identified in order to select the drug individually. Self-medication with antibiotics is unacceptable; they should only be prescribed by a doctor.
Conservative therapy
Conservative therapy involves the use of such means as:
- local vasoconstrictor drugs - to eliminate swelling of the mucous membrane and restore normal nasal breathing;
- local antibacterial drugs - to combat pathogenic microflora;
- antihistamines - to relieve swelling, relieve an allergic reaction due to the allergic nature of inflammation;
- physiotherapy - UHF and other procedures in the period after the exacerbation is relieved.
Doctors often prescribe complex remedies. The list of frequently prescribed drugs includes the herbal medicine Sinupret® in the form of tablets and drops for oral administration. It acts comprehensively: it helps relieve nasal congestion, has an antiviral effect and reduces the likelihood of complications. It is especially effective when included in treatment from the first days of the disease.
Puncture and probing of the paranasal sinuses
Sinus probing is a method of examining the sinus cavities using a thin endoscopic instrument. The study can be supplemented by the administration of medicinal solutions through a catheter. The main task of the procedure is to isolate the contents of the sinus for examination in the laboratory. The doctor can also determine the volume of the sinuses, which is important for swelling and tissue changes.
Sinus puncture is performed under local anesthesia. The procedure allows you to empty the sinus and is prescribed when drug treatment is ineffective.
Drainage
Treatment of rhinosinusitis by drainage is carried out under local anesthesia. The doctor inserts a sinus catheter into the nasal cavity, reaching the nasopharynx. The nasopharynx and nasal vestibule are blocked by inflating small balloons. The necessary pressure is created in the nasal cavity to empty the sinuses. Then the sinuses are filled with a medicinal solution.
Surgical intervention
The ineffectiveness of conservative methods forces the doctor to recommend surgical treatment. This is especially true for patients with chronic rhinosinusitis caused by the anatomical features of the structure of the nasal passages and other structures.
There are several types of operations that are indicated in specific cases: removal of polyps or adenoids, elimination of a deviated nasal septum (septoplasty), etc. Interventions can be carried out traditionally or using modern technologies - laser, endoscopic equipment.
Diagnosis of sinusitis
Sinusitis is treated by an otorhinolaryngologist, but in the case of psychopathic factors, it is necessary to involve a psychotherapist. The doctor listens to the patient's complaints and examines his nose (performs rhinoscopy) using special mirrors. A source of local light helps him in this - a head reflector-mirror. In addition, the larynx and pharynx, as well as the ears, are examined using ear specula.
To accurately assess the condition of the nasal sinuses and diagnose the disease, the following types of research are used:
- rhinoscopy - performed using a rhinoscope to examine the nasal septum, determine the degree of swelling and irritation of the mucous membrane;
- endoscopic examination using optics - shows the presence of an inflammatory process in the sinuses, polyps and other pathologies, the condition of the mucous membrane and nasal septum;
- radiography – records foci of inflammation;
- computed tomography – in addition to areas of inflammation, reveals complications;
- puncture - taking samples from the nasal sinuses to test for the presence of a bacterial infection.
Instrumental research methods
- Rhinoscopy. Anterior rhinoscopy against the background of diffuse congestive hyperemia and edema of the nasal mucosa reveals a typical sign of purulent rhinosinusitis - the presence of pathological discharge in the anastomosis area of the affected paranasal sinuses. With sinusitis and frontal sinusitis, the discharge can be seen in the middle nasal passage, and with sphenoiditis - in the upper.
- Endoscopic examination requires a minimum of time and is painlessly tolerated by the patient. The study includes three main points: sequential examination of the lower, middle and upper nasal passages. The method allows you to identify an additional anastomosis of the maxillary sinus. With a choanal polyp, a formation is detected, the stem of which comes from the anastomosis of the maxillary sinus.
- Diaphanoscopy. Illumination of pericutaneous formations or cysts with a narrow beam of light. Allows to identify a decrease in pneumatization of the maxillary and frontal sinuses.
- Ultrasound is a fast, non-invasive method that is used mainly for screening purposes, to diagnose inflammatory diseases and cysts of the maxillary and frontal sinuses. Both special devices for scanning the paranasal sinuses and standard equipment are used. The sensitivity of ultrasound in diagnosing sinusitis is lower than that of X-ray and CT.
- X-rays of the paranasal sinuses are usually performed in the nasomental projection. To clarify the condition of the frontal and sphenoid sinuses, an additional study can be carried out in the nasofrontal and lateral projections. X-ray of the ethmoid bone sinuses is not very informative. Poor quality radiography often leads to diagnostic errors.
- CT , which is performed in a coronal projection, is the most informative method and is gradually becoming the “gold standard” for studying the paranasal sinuses. CT not only makes it possible to establish the nature and extent of pathological changes in the paranasal sinuses, but also reveals the causes and individual features of the anatomical structure of the nasal cavity and sinuses, leading to the development and recurrence of rhinosinusitis. High-resolution CT allows you to visualize structures that are not visible with conventional radiography.
- MRI , although it provides better visualization of soft tissue structures, is not one of the main methods for diagnosing rhinosinusitis. This method gives virtually no idea of the patency of the air spaces connecting the paranasal sinuses with the nasal cavity. MRI is indicated only in certain situations - for example, if a fungal infection of the paranasal sinuses is suspected or the possible tumor nature of the disease, as well as with orbital and intracranial complications of rhinosinusitis. MRI is the most informative method for differential diagnosis between a cerebral hernia (meningoencephalocele) and a tumor or inflammatory process in the roof of the ethmoidal labyrinth.
- Diagnostic puncture and probing make it possible to assess the volume and nature of the contents of the affected sinus and indirectly obtain an idea of the patency of its natural opening.
To assess the patency of the anastomosis of the punctured sinus, a simple scheme is used, taking into account 3 degrees of violation of the patency of the anastomosis (see table). To do this, using a syringe connected to a needle or drainage tube, the contents are first aspirated, and then the sinus is washed.
Assessment of the patency of the natural anastomosis of the paranasal sinuses
| Normal patency of the anastomosis | During aspiration, air or liquid contents of the sinus enter the syringe; when rinsing, the liquid flows freely into the nasal cavity |
| Obstruction of the 1st degree | During aspiration, negative pressure is created; during rinsing, the liquid freely enters the nasal cavity (valve mechanism and negative pressure in the sinus) |
| Impairment of patency II degree | Aspiration from the sinus is impossible; rinsing is possible only by increasing pressure on the syringe plunger |
| Level III obstruction | Neither aspiration nor lavage of the sinus is possible: there is a complete blockage of the anastomosis |
How to cure sinusitis in adults
This disease can be catarrhal, purulent, mixed type.
With catarrh, profuse discharge and swelling of the sinuses are observed. With proper treatment, recovery occurs relatively quickly.
With purulent sinusitis, bacteria and other pathogenic microorganisms develop in the appendages. The temperature rises, general intoxication is observed, and the discharge becomes greenish. Without adequate treatment, inflammation can spread to bone tissue.
If the causative agent is a virus, the symptoms resemble a cold: discomfort in the throat, runny nose, stuffy nose, cough. In this case, antibiotics are not prescribed. The main therapy is bed rest, plenty of warm fluids, and saline nasal sprays for rinsing. At high temperatures, antipyretic drugs are prescribed. Normally, recovery occurs within 7–10 days; if the process is prolonged, the alarm should be sounded.
If the nasal discharge has become thick, with a greenish-yellow tint, and the swelling does not go away, antibiotics may be prescribed after additional examination. In this case, the person recovers in 10–14 days.
Sinusitis can be allergic - the disease becomes chronic and manifests itself throughout the year. Treatment involves identifying the allergen and taking antihistamines. It is possible to prescribe immunotherapy.
Previously, in the treatment of sinusitis, vasoconstrictor drops were widely used, which temporarily reduced swelling of the mucous membrane. But it turned out that their long-term use (over 5 days) worsens the condition of the ciliated epithelium and leads to the development of drug-induced rhinitis. And children may even experience symptoms of poisoning. Considerable problems also arise due to the uncontrolled use of antibiotics and antiviral drugs.
When drug therapy does not give the expected results, a surgical procedure is performed - puncture. A puncture is made to remove accumulated fluid, and then the sinuses are washed with antiseptic solutions. Elimination of curvature of the septum, removal of polyps and tumors also cannot be done without surgical intervention. Physiotherapeutic procedures may be additionally prescribed during treatment: heating, laser and magnetic therapy.
Only a doctor can choose the right remedy for sinusitis, taking into account the research results. There is no universal pill for this disease; the approach to each patient is individual.
Odontogenic sinusitis
A special place is occupied by odontogenic maxillary sinusitis, which occurs due to problems with teeth. It can be perforated, as well as chronic, often purulent.
Main reasons for development:
- caries and periodontitis;
- osteomyelitis, suppurating cysts of the upper jaw;
- perforation of the maxillary cavity, the presence of root remains due to the removal of severely neglected teeth;
- unerupted teeth;
- careless work of the dentist when filling dental canals.
It also happens that the roots of the tooth grow into the maxillary sinus, and granulomas and subperiosteal abscesses appear at their tips.
The disease is diagnosed using radiographic or tomographic examination.
Its distinctive features are:
- unilateral damage to the maxillary sinus (during infection, bilateral sinusitis mainly develops);
- absence of anatomical predispositions to development - deviated nasal septum and other anomalies.
Treatment is carried out only surgically.
Prices
| Service | price, rub. |
| Collection of material for histological examination (Biopsy) | 4000,00 |
| Collection of material for bacteriological research | 350,00 |
| Diagnosis of disorders of the separation mechanism of the hypopharynx | 1250,00 |
| Consultation with an otolaryngologist, candidate of medical sciences | 2600,00 |
| Consultation with an otolaryngologist | 1800,00 |
| Repeated consultation | 1300,00 |
| Inhalation (ultrasonic) device Omron nebuliser | 350,00 |
| Steam inhalation | 350,00 |
| Toilet cavity boil/nasal abscess | 3000,00 |
| Radio wave nasal polypotomy (multiple polyps, one side) | 21800,00 |
| Radio wave coagulation of eroded vessels of the nasal septum | 6000,00 |
| Radio wave coagulation of blood vessels for recurrent nosebleeds | 14500,00 |
| Radio wave coagulation of the inferior turbinates | 18200,00 |
| Primary surgical treatment of nasal wounds up to 1.5 cm | 2500,00 |
| Primary surgical treatment of nasal wounds over 1.5 cm | 2900,00 |
| Puncture of the maxillary sinus (on one side) | 2100,00 |
| Removal of a foreign body from the nasal cavity | 1450,00 |
Home Remedies for Sinusitis
During the acute period of illness at home, it is recommended to only rinse the nose with an isotonic (0.9%) saline solution or a decoction of medicinal herbs and drink more warm teas.
- Decoctions can be prepared from St. John's wort, eucalyptus, sage, calendula, which have antibacterial properties, as well as chamomile, mint, linden, which have an antispasmodic effect. The decoction must be freshly prepared.
- Vials of sterile saline solution of the required concentration are sold at the pharmacy. At home, 9 grams of table or sea salt are dissolved in 1 liter of boiled water.
- When the acute period is over, you can do steam inhalations with eucalyptus and menthol oils. For this purpose, an inhaler or an aroma lamp is used. It is recommended to avoid drinking coffee and alcoholic beverages, which remove fluid from the body. Tea with honey, rose hips and/or ginger is beneficial. Massage of the paranasal sinuses and breathing exercises give a good effect. You can warm your nose, but this is contraindicated in case of fever and purulent sinusitis.
Myths and dangerous misconceptions about treating sinusitis
There is an opinion that sinusitis is a minor disease that will end in a week without treatment. However, it is worth remembering: the nasal sinuses are located close to the brain and eyes, to which the inflammatory process can spread under unfavorable circumstances. It should also be borne in mind that sometimes the natural opening connecting the cavities of the sinuses and nose is blocked, then there is no discharge at all. In this case, puncture and x-rays are used for diagnosis.
Another myth is related to punctures. They say that after one puncture you will have to do this procedure constantly. But today this is done quickly and painlessly, under local anesthesia. The puncture site heals without changing the anatomy of the sinus.
Sinusitis during pregnancy
Due to hormonal changes during pregnancy, almost 30% of women experience swelling and congestion in the nasal mucosa. This makes it difficult for mucus to come out and creates ideal conditions for bacteria to multiply in the sinuses. Increased stress on the immune system leads to a weakening of the defense mechanism, which may result in infectious rhinosinusitis. Disturbances in nasal breathing, up to its complete blockage, lead to insufficient saturation of the mother’s blood with oxygen, which can lead to fetal hypoxia. This is especially dangerous in the first trimester of pregnancy, when vital organs are forming. If sinusitis is infectious in nature, intoxication of the whole body begins. The maxillary and frontal sinuses are most often affected.
It is impossible to fully treat sinusitis during pregnancy, since many drugs have a negative effect on the fetus. Therefore, in order to avoid the addition of a bacterial infection and the development of complications, at the first signs of ARVI and allergic rhinitis, you should immediately consult a doctor.
The main method of treating sinusitis during pregnancy is to rinse the nose with a water-salt solution and decoctions of medicinal herbs to remove mucus, reduce swelling, and restore drainage function. Dry heat and inhalations are also recommended, but all therapeutic techniques should be discussed with a doctor.
X-rays cannot be taken during pregnancy, so diagnosis is made based on palpation and rhinoscopy. Allergic sinusitis and vasomotor rhinitis are excluded, and in the case of infectious sinusitis, the type of pathogen is determined. Pregnant women can undergo a puncture under local anesthesia. A sample is taken for bacteriological culture, and then the sinuses are washed with antiseptic solutions. In cases of severe bacterial sinusitis, it is possible to prescribe antibiotics that have minimal risk to the fetus.
Sinusitis in children
The maxillary sinuses are fully formed by the age of 7, so children most often have frontal sinusitis and ethmoidal sinusitis. Their symptoms are the same as those of adults, but they are more pronounced. The disease begins with nasal congestion and dry cough in the evening (night). Then a headache appears and appetite decreases.
In children under one year of age, ethmoiditis is especially severe. There is severe intoxication, swelling and copious discharge. The risk of infection of the bronchopulmonary system and even the development of sepsis cannot be ruled out.
In children from 1 to 3 years old, infection of the eyes is also possible, in children 4–7 years old – damage to the maxillary sinuses, and in older children – inflammation of the frontal part.
Factors predisposing to the development of rhinosinusitis
- Rhinitis.
- Intolerance to non-steroidal anti-inflammatory drugs.
- Anomalies in the structure of the nasal cavity and paranasal sinuses (deviated nasal septum; bulla of the middle turbinate; additional anastomosis of the maxillary sinus, etc.).
- Immunodeficiency states (X-linked agammaglobulinemia; common variable immunological deficiency; deficiency of IgG subclasses; selective IgA deficiency; hyper-IgM syndrome; HIV).
- Diseases accompanied by a slowdown in MCT (Kartagener's syndrome; Young's syndrome; cystic fibrosis).
- Wegener's granulomatosis.
- Hyperplasia of the pharyngeal tonsil, adenoiditis.
- Gastroesophageal reflux disease.
- Fistula between the oral cavity and the maxillary sinus.
Prevention
To prevent sinusitis, you should maintain your immune status at the proper level. To do this, it is recommended to lead a healthy lifestyle, enrich the menu with vegetables and fruits, harden yourself, and play sports. Sinusitis often occurs after ARVI and influenza, so it is advisable to get vaccinated before the start of the epidemic period. When the first signs of sinus inflammation appear, you should consult a doctor for adequate treatment to prevent the disease from becoming chronic. In addition, it is important to promptly identify and correct defects of the nasal septum (curvatures), due to which the passage of mucus may be difficult, as well as regularly sanitize the oral cavity.
Sinusitis
Sinusitis is one of the most common types of sinusitis. This disease is accompanied by inflammation in the maxillary and maxillary cavities. During inflammation, swelling of the mucous membrane occurs, which blocks the opening from the sinus to the nasal cavity. Mucus begins to accumulate in the sinus space, pathogenic bacteria multiply, and pus appears. Inside the cavity, pressure occurs on the vessels, and the person begins to feel pressing pain at the site of accumulation of pus.
Chronic sinusitis is the result of a long inflammatory process, when a person has had sinusitis for more than 2 months. The patient develops general weakness, nasal discharge has an unpleasant odor, the sense of smell is impaired, and a night cough appears. Chronic sinusitis is characterized by inflammation of only one sinus, right or left. Pressure in the sinus can cause a deviated nasal septum.
Symptoms of sinusitis
The following symptoms are characteristic of sinusitis:
- increased body temperature;
- copious discharge, nasal congestion;
- disturbances of smell;
- weakness;
- headache radiating to the forehead, bridge of the nose, teeth;
- pain that intensifies when tilting the head and pressing on the sinus;
- constant, intense pain;
- a feeling of fullness in the forehead and cheeks, aggravated by tilting the head, coughing and sneezing;
- photophobia and lacrimation.
Signs of sinusitis
If after a flu or cold the temperature rises again, your health worsens, severe pain appears when tilting your head and when pressing on the sinuses, then you need to urgently consult an otolaryngologist. These could be manifestations of sinusitis! Sinusitis in adults is often advanced, since adults are usually in no hurry to see a doctor.
Treatment of sinusitis
Antibiotics for sinusitis are used only after a complete examination of the patient, based on the characteristics of his body and possible allergic reactions.
Antibiotics are not advisable in case of sinusitis of allergic or fungal origin. For mild sinusitis, inhalations, rinses and immunotherapy are also sufficient.
1 Rhinoscopy in MedicCity
2 Video endoscopy of the nasopharynx in MedicCity
3 ENT office in MedicCity