Cheilitis is an inflammation of the red border, mucous membrane and skin of the lips. In common parlance, the disease is called jamming. The inflammatory process can be long-lasting and periodically worsen. In healthy young people it often goes away on its own, but in children, the elderly and people with chronic diseases it should be treated with medication. Elderly people have a high risk of leukoplakia and malignancy of the process.
Cheilitis is treated by a dentist, and if necessary, a therapist, pediatrician and other specialized specialists - an endocrinologist, an infectious disease specialist, etc. - are involved in drawing up a treatment plan.
Causes of cheilitis
Cheilitis can be an independent disease and a manifestation of other pathologies of the mucous membranes and internal organs. The most common causes of the disease include:
- Dermatoses. The mucous membranes and skin of the lips can be involved in the pathological process in lichen planus, psoriasis, erythematoses and other skin diseases.
- Unfavorable factors. Exposure to hot and cold air, wind, and excessive exposure to UV rays are especially common causes of cheilitis in people who work outdoors and under special weather conditions.
- Allergic reactions. Allergies can be triggered by chemical factors, ultraviolet rays, cosmetics, etc.;
- Other diseases. Secondary cheilitis often develops against the background of atopic dermatitis, eczema, neuritis of the facial nerve, etc.
Natural protective mechanisms are weakened by such factors as hypothermia, previous surgical interventions, long-term antibacterial therapy, hypovitaminosis, etc.
Ask a Question
Treatment results
Under the influence of the therapy, it was possible to achieve regression of AC symptoms in most patients, while improving skin trophism. The topical glucocorticosteroids used quickly stopped the exacerbation of AC.
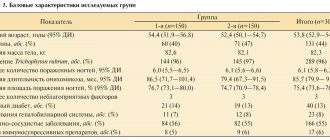
The children were under observation throughout the treatment period. The result of therapy was assessed as good when all symptoms of AC disappeared or were significantly weakened; as satisfactory – with slight improvement; as negative – in the absence of treatment effect. A good effect from treatment with external therapy was achieved by 62 (62%) patients, a satisfactory effect by 31 (31%), and no effect was observed in 7 (7%) children.
Thus, when treated with the external therapy presented above, the majority of children with AC managed to reduce hyperemia, peeling of the KKG and skin of the perioral area, as well as ensure a decrease in skin lichenification and healing of cracks.
Clinical improvement of the atopic process on the lips during treatment with external agents occurred on the 2-3rd day of treatment. The dynamics of clinical manifestations of AC during therapy are presented in the figure.
The duration of remission of the isolated form of AC was on average 4–6 months, and remission of AC against the background of AD was 2–3 months.
The dentist should consider the symptoms of AC, perioral dermatitis, and cracked oral commissures in children as possible manifestations of an allergic process. It is necessary to recommend that parents contact a pediatrician and allergist to have their child examined.
Symptoms and types of disease
Cheilitis on the lips can manifest itself in different ways depending on the form of the disease. Thus, the exfoliative type of inflammation appears more often in women; its main symptom is peeling. The disease is based on neurological and endocrine disorders. Peeling occurs on the red border of the lips and does not affect the skin and mucous membranes. The disease rarely spreads to the entire red border, so part of it remains unchanged.
With severe dry skin, peeling is accompanied by symptoms such as:
- feeling of dry lips;
- burning;
- formation of easily detachable scales.
The disease is long-term and sluggish, with periods of exacerbation occurring from time to time. It rarely goes away on its own. With the exudative form, pain, swelling of the lips, and the formation of large crusts may occur.
Glandular cheilitis develops against the background of the proliferation of minor salivary glands and their subsequent infection. With congenital pathologies, signs of such inflammation of the lips are present in almost all cases. Acquired overgrowth may be associated with chronic diseases of the periodontal tissues, tartar, multiple caries - diseases leading to infection of the dilated ducts. Lesions of the lower lip with this form of cheilitis are more common. The disease develops with the appearance of dry lips, which is initially easy to correct with the help of cosmetics. Subsequently, cracks begin to form, deepen and begin to bleed. The condition is aggravated by the constant desire to lick dry lips - cracks and ulcers can become weeping and become permanent due to the inelasticity of the skin of the lips.
Contact allergic cheilitis develops after exposure to an allergen - an irritant. The most common of them are components of lipsticks and other care products. Allergies can also be associated with bad habits, for example, constantly keeping pencils, pens and other foreign objects in the mouth. Musicians may develop occupational cheilitis due to constant contact of the mouthpieces of wind instruments with their lips. The main symptoms of the disease include:
- severe itching;
- burning;
- swelling of the lips;
- redness of the skin and mucous membranes.
Manifestations intensify upon contact with the allergen. Bubbles of different sizes may form; their spontaneous or accidental opening leads to the formation of ulcers and cracks. Chronic forms of allergic disease are accompanied by peeling, slight itching and the absence of other signs of inflammation.
Actinic cheilitis belongs to the category of diseases that are based on increased sensitivity to weather and other external factors. Usually occurs in response to sun exposure. Exudative forms of this disease are accompanied by the formation of crusts. Sometimes small blisters form, the opening of which leads to painful erosions. In the absence of exudate, the main symptoms are pain, dryness, and burning of the lips. Actinic cheilitis often degenerates into precancerous diseases.
In atopic cheilitis, the main cause of the disease is dermatitis of the same name, or neurodermatitis. It appears in people with an allergic predisposition, and the triggering factor can be medications, cosmetics, food products, as well as microorganisms and their waste products. The disease is accompanied by redness of the lips, itching and peeling of the red border, and damage to the corners of the mouth. After acute symptoms subside, peeling and thickening of the skin may occur. Dryness stimulates the formation of cracks.
Macrocheilitis is part of the Rossolimo–Melkersson–Rosenthal syndrome. Appears against the background of neuritis of the facial nerve and the symptom of a folded tongue. Develops due to infectious-allergic effects against the background of genetic predisposition. Manifests itself with the following symptoms:
- lip enlargement;
- severe itching;
- swelling of other parts of the face;
- bluish-pink color of swollen areas of the lips.
One or both lips, cheeks, and upper parts of the face may be affected. Neuritis leads to facial asymmetry, and the nasolabial fold is smoothed out.
Hypovitaminous cheilitis of the lips develops against the background of a deficiency of B vitamins. Burning and dryness of the oral mucosa and lips appear. The mucous membranes become swollen and red, peeling occurs on the red border, and cracks appear. They are prone to bleeding, which is also associated with a lack of vitamins. The tongue may become enlarged and can easily become imprinted with teeth.
With candidal cheilitis, the inflammatory process is accompanied by the formation of white plaque on the mucous membranes. The cause of this disease is the proliferation of a fungus of the genus Candida; it often affects infants, people after radiation and chemotherapy, as well as patients with immunodeficiencies. Cheilitis develops with long-term use of antibiotics and immunosuppressants.
Prevention methods
Careful oral hygiene
To prevent the appearance of cracks, you need to protect the skin and mucous membranes from adverse effects. To do this, you should get rid of the habit of licking your lips and corners of your mouth, using medicinal cosmetics for dry skin and hygienic lipsticks. To prevent infection from getting onto the skin of the lips from the oral cavity, it is necessary to brush your teeth at least twice a day, as well as treat caries and inflammatory gum diseases.
Changing your diet
If pockets begin to appear in the corners of the mouth, it is necessary to limit the consumption of spicy, sour and salty foods that irritate the mucous membranes and skin. You can add non-acidic fruits and vegetables to your daily diet, as well as foods containing iron and riboflavin (beef, liver, dairy products, cabbage, potatoes, peanuts, almonds, etc.).
Up to contents
Diagnostic features
If inflammation appears on the lip, it is advisable to visit a therapist, for children a pediatrician, if indicated, an infectious disease specialist, a dentist, or other specialized specialists. Diagnosing cheilitis is usually not difficult - a specialist will conduct an examination, listen to complaints and prescribe a series of tests. If the allergic nature of the disease is suspected, allergy tests may be recommended, and if plaque appears, it is advisable to take a scraping. To detect endocrine and other disorders that may cause the disease, biochemical blood tests and other diagnostic methods are often prescribed. In rare cases, a biopsy is required to differentiate cheilitis from other pathologies. This will help to exclude the malignant or precancerous nature of inflammatory formations and prescribe the correct treatment.
1.3. Treatment
Inflammation of the lips - cheilitis, as mentioned earlier, can occur as a result of exposure to endogenous and exogenous factors. In this regard, treatment of any form of cheilitis should be aimed at eliminating them [47].
Exomatous cheilitis
Treated in the same way as eczema. Detoxification therapy is prescribed: prednisolone 40-50 mg (orally or intravenously), 10% calcium chloride, and courses of antihistamines (fenkarol, claritin, zyrtec) [23].
Since all patients, to one degree or another, suffer from functional disorders of the nervous system, sedative therapy (tenaten, afobazole, persen), and at the same time vitamins B and C are indicated. The prescription of group B drugs, in particular B1 and B6, is pathogenetic, since thiamine and pyridoxine influence the metabolism of amino acids and histamine, which normalizes the psycho-emotional state [24]. The prescription of vitamin C for eczematous cheilitis is explained by its participation in redox reactions and carbohydrate metabolism; vitamin C normalizes capillary permeability and eliminates tissue hypoxia [4, 67].
Also used are lotions for several days on the lips from a borax solution, as well as applications of 1% naphthalan oil [2].
Currently, creams containing 0.5% prednisolone and other corticosteroid drugs (advantan, celestoderm B, flucinar) are widely used [44].
If cracks appear with eczematous cheilitis (especially in the corners of the mouth), a microbiological examination is carried out. If streptococci or staphylococci are detected, ointments containing antibiotics and steroids (levomikol, tetracycline 1% eye ointment) are prescribed. But since long-term use of antibiotics can cause exacerbation of eczematous cheilitis, they are used for a short time [18]. In the contact form of eczematous cheilitis, eliminating the effect of a chemical agent quite quickly leads to a cure.
Treatment of exfoliative cheilitis
still remains a challenge, since the pathogenesis and etiology of the disease are unclear [25].
Patients with this disease experience more or less significant impairment of the nervous system. Therefore, general treatment should be carried out jointly with a neurologist and be accompanied by the prescription of drugs that calm the nervous system for a long time. Antihistamines are also indicated along with vitamins [27].
In case of persistent dermatosis, Bucca rays in an initial dose of 100 Gy once a week have an effective therapeutic effect. Treatment is carried out at intervals of 7-10 days until the pathological elements disappear (3-4 procedures) [34].
According to S.A. Rabinovich (2000), for exfoliative cheilitis, blockade of the red border of the lips with solutions of 1% novocaine or 1% lidocaine solution is effective.
For simple glandular cheilitis
, complicated by eczema, topical ointments based on corticosteroids are prescribed, and in case of secondary infection, creams and ointments containing corticosteroids and antibiotics, and in some cases, injections of histoglobulin [19, 60].
It has been clinically proven that the long-term course and chronicity of pathological changes in the red border of the lips can be facilitated by violations of the local immunity of the oral cavity [35]. The use of the drug Imudon stimulates the cells of the reticuloendothelial system and promotes the healing of the oral cavity (6-8 tablets per day for 2-3 weeks) [12].
Sometimes phonophoresis with interferon is prescribed (if PCR diagnostics reveal viral DNA). In this case, general antiviral drugs can also be prescribed [39, 40].
For adenomatous hyperplasia of the lip, electrocoagulation is prescribed [41], and surgical excision of the red border of the lip is extremely rarely used [38].
In the treatment of actinic cheilitis
The influence of insolation should first be excluded. The use of photoprotective creams and ointments (melascrine light, SPF 50+; bioderma, SPF 50; photoderm Ski SPF) helps stop the process. Among the means of general treatment, vitamin therapy is indicated, in particular vitamins B12, B6, A. Some authors believe that this, on the one hand, affects the normalization of proliferative processes, and on the other, affects the peripheral nervous system, normalizing psycho-emotional reactions and reducing the feeling of itching [69, 77].
In case of persistent actinic cheilitis, they resort to laser ablation of the lesion, electrodissection or chemical peeling. These methods are quite aggressive and cause cosmetic defects (scars) [22, 51, 58].
Treatment of abrasive precancerous cheilitis Manganotti
consists, first of all, in eliminating local traumatic factors; mandatory conditions - the patient’s refusal to smoke and eat hot and spicy foods; carry out sanitation of the oral cavity, including rational prosthetics; Vitamins A and E are prescribed orally, as well as applications of these vitamins on erosion and ointments containing corticosteroids (Advantan, hydrocortisone, Triderm, Flucinar) [6, 57].
If the erosion does not heal within 1-1.5 months, then it is surgically excised within healthy tissue, followed by histological examination. When using X-rays, the therapeutic effect is achieved only in large doses. All patients with Manganotti cheilitis require clinical observation [36].
Treatment of cheilitis must be improved, and a search for new effective methods of therapy is necessary.
Treatment methods
The treatment plan for cheilitis is developed individually, depending on the form of the disease, the severity of symptoms, and the characteristics of the health condition. Thus, in the treatment of the exfoliative form of the disease, the key element of effective treatment is the impact on the psycho-emotional sphere: you will need to contact a neurologist or psychoneurologist to prescribe sedatives and antidepressants according to indications. Consultation with an endocrinologist may be required.
Local treatment may involve the use of laser or ultrasound physiotherapy, local anti-inflammatory drugs, and less commonly, radiation therapy. Elimination of excessive dryness is possible with the help of hygienic lipsticks. To speed up recovery, the doctor may prescribe vitamin therapy, UVOC and other methods of maintaining the body's defenses.
Therapy for glandular cheilitis consists of using local anti-inflammatory agents. Antibacterial, antiviral, and hormonal ointments can be used. A radical method of therapy is electrocoagulation of the salivary glands or their surgical removal, as well as laser ablation. These methods are used when conservative methods are ineffective. After the main course, the doctor will prescribe medications to prevent relapses - they will eliminate dry or weeping skin. It is important to sanitize the oral cavity in a timely manner and undergo professional teeth cleaning.
Treatment of atopic cheilitis consists of eliminating irritating factors. Drugs with antipruritic and anti-inflammatory effects can be used locally, and therapy with antihistamines with a systemic effect is also carried out. The use of glucocorticosteroids allows you to get quick relief, but it is important to strictly adhere to medical prescriptions - they can only be used for a short time. It is important to follow a hypoallergenic diet and remove allergenic foods from the diet.
Therapy for meteorological cheilitis begins with limiting harmful effects, for example, insolation. Local treatment is usually carried out - the doctor prescribes hormonal agents and protective creams, including those with SPF. The course of treatment is supplemented with vitamins - vitamin-mineral complexes or individual preparations (B, PP, C, etc.).
In the treatment of macrocheilitis, immunocorrective and antiviral therapy is of particular importance. The doctor may prescribe:
- hormonal anti-inflammatory drugs of systemic action;
- novocaine blockades;
- antihistamines, etc.
Laser therapy can have a positive effect on the correction of the entire triad of symptoms. Other physical therapy methods have been successful in treating facial neuritis.
1.2. Use of computer capillaroscopy in medicine
Capillaries play a key role in maintaining homeostasis in the body, providing tissues with oxygen, nutrients and metabolic products between tissues and the bloodstream. They are the first to respond to the influence of environmental factors and changes occurring in central hemodynamics. Microcirculation parameters are used to diagnose various diseases and identify prognostic signs [30].
In dentistry, computer capillaroscopy has begun to be used in the diagnosis of periodontal diseases and to monitor the effectiveness of their treatment. Disruption of microcirculation in periodontal diseases is accompanied by shifts in the parameters of vascular-platelet and coagulation hemostasis, caused by local tissue coagulation factors. Disorders of microcirculatory hemostasis are not specifically isolated, but to a certain extent reflect the nature of inflammatory and destructive processes in periodontal tissues [8].
Under the guidance of prof. E.K. Krechina defended a number of dissertations devoted to the study of microcirculatory disorders of periodontal tissues in various forms of periodontitis [21, 26].
It has been established that changes in the hemodynamics of tissue blood flow in the initial stages of inflammatory diseases are moderate (linear and volumetric blood flow velocities are reduced by 22-40%). As the severity of the inflammatory process in the periodontium increases (moderate and severe periodontitis) and with periodontal disease, changes in the hemodynamic parameters of tissue blood flow become pronounced (blood flow velocity decreases by 56-80%) [14].
When assessing the reaction of the vascular bed against the background of various diseases of the oral cavity, hemodynamics is still used in isolated cases. A study of the microvasculature in patients with glossalgia revealed in a significant number of cases spastic and spastic-atonic syndromes of capillary hemodynamics, which indicated a violation of the peripheral blood supply to the oral cavity at the level of the microvasculature (changes in metabolism and hypoxia). Subsequently, this served as the basis for prescribing anti-inflammatory and antioxidant therapy [10].
Studies have found that an increase in vascular density in lichen planus (LP) may be associated with the mechanism of angiogenesis and serves as an indicator of the development of the pathological process. In the diagnosis and monitoring of the development of LP, capillaroscopy plays an important role, as it allows one to determine all vascular changes in patients suffering from this pathology. The method makes it possible to evaluate differences in the vascular pattern in healthy people and people suffering from LP with high and low degrees of basement membrane degeneration [15, 66, 72, 79].
The experiment involved studies of the microvasculature using a helium-neon laser (HNL) for diseases of the oral cavity. The effect of GNL on the vascular system of tissues is manifested by an increase in vascular tone and fibrinolytic activity of the blood. This method has been widely used in the treatment of periodontal diseases, Melkersson-Rosenthal syndrome, etc. [3].
Thus, studies of microhemodynamics in all kinds of chronic inflammatory processes, such as diseases of the lips (cheilitis), are diagnostically and prognostically promising.
Possible complications
Failure to see a doctor in a timely manner often causes serious complications. The disease itself often does not pose a serious health risk. But only an experienced specialist can tell you how to treat cheilitis. Self-medication can lead to unpleasant consequences and provoke the occurrence of a chronic form of the disease. In addition, cheilitis is dangerous because its symptoms can mask malignant tumor processes. It is important to remember that some forms are prone to malignancy - cheilitis may be followed by precancerous conditions.
Diagnostics
In the process of diagnosing this disease, the key task of a specialist is to differentiate exfoliative cheilitis from other diseases that are similar in external manifestations.
Thus, the dry form of cheilitis in the diagnostic process is compared with the following diseases:
- meteorological cheilitis,
- atopic cheilitis,
- contact allergic cheilitis.
The exudative form requires differentiation with the following diseases:
- exudative form of actinic cheilitis;
- eczematous cheilitis;
- erosive-ulcerative form of lupus erythematosus.
Prognosis and prevention
With timely treatment and the absence of malignancy processes, the prognosis is almost always favorable. If the therapy has caused noticeable cosmetic defects, you can resort to methods for correcting the appearance of the lips.
To prevent complications, it is important to understand whether you are at risk. The presence of allergic diseases and dermatoses, chronic endocrine diseases, and wearing dentures increase the risk of developing pathology. To prevent the appearance of cheilitis, it is important to adhere to several rules:
- regularly visit the dentist, sanitize the oral cavity, remove tartar;
- promptly replace outdated fillings and orthopedic structures, contact after chipped teeth and injuries to prevent lip injury from the sharp edges of fillings and enamel;
- For the manufacture of prostheses, contact only professionals;
- eat properly and nutritiously to prevent hypovitaminosis;
- try to avoid prolonged exposure to the sun and use products with SPF, including for lips;
- be attentive to your health and promptly treat diseases of the gastrointestinal tract, endocrine, nervous system, and internal organs.
Reasons for the development of the disease
The most common cause of the disease is heredity. Also among the provoking factors are the presence of allergies, reduced immunity, lack of nutrients and vitamins in the diet, and chronic diseases.
Atopic cheilitis and intestinal dysbiosis are often associated. Chronic stress, disruptions in the endocrine system, bad habits and exposure to certain medications can also influence its appearance. Among the allergens that can trigger the development of this disease are dust, pollen, food products, dyes and some medications.
Allergic cheilitis
A disease that develops in allergy sufferers upon contact with an allergen and affects the surface of the lips. Typical manifestations of this type of cheilitis are a feeling of itching and burning on the lips, dryness and significant discomfort. The lips begin to dry and peel, and the scales of dead epithelium begin to flake off.
The main cause of this disease is the patient’s increased sensitivity to external irritants, in particular to allergens. Allergic, or, as it is also called, contact cheilitis can develop gradually.
It all depends on the patient’s personal sensitivity to allergens, and it can develop over several weeks, months and even years. The duration of this process is determined by the peculiarities of the endocrine system, as well as the degree of manifestation of allergic reactions.
This disease practically does not appear in children. According to statistics, most patients with allergic cheilitis are women over twenty years of age.
Causes of the disease
In most cases, allergic cheilitis is caused by contact allergic irritants. Among the most common allergens that cause cheilitis is lipstick. It is not the lipstick itself that is dangerous, but the substances it contains - rhodamine, eosin and others. Provoking factors also include low-quality dental implants and plastic dentures.
Allergic manifestations may appear after contact with citrus fruits, as well as in patients who have the habit of chewing pencils or pens. The disease is also common for those whose work involves playing wind instruments or hazardous chemical production.
Symptoms of the disease
The disease manifests itself as hyperemia and swelling of the lips, as well as a sensation of itching and burning, accompanied by the formation of erythema. Small painful blisters appear and burst on the affected areas of the lips. If the pathogenic process is prolonged, over time, small scars and scars will form in their place on the lips. Dry lips only increase over time.
Inflammation almost never extends beyond the red border around the lips. In rare cases, it may spread to adjacent skin. Sometimes the inflammatory process moves to the oral mucosa. This form of allergic cheilitis is characterized by hyperemia (significant redness of the tissues), the appearance of noticeable swelling of the tissues, and when trying to palpate, pain occurs.
Diagnosis and treatment
Diagnosis of the disease is carried out by a dentist together with an allergist. To determine the allergen, it is necessary to conduct allergy tests.
When making a diagnosis, it is important to distinguish allergic and atopic cheilitis, as well as exclude exfoliative and actinic cheilitis. Treatment of this disease includes the mandatory elimination of the irritant or allergen that caused it.
Systemic (general) and topical (local) drug therapy is used. General therapy refers to the use of medications taken orally. To relieve allergy symptoms, a course of antihistamines is used. If the case is sufficiently complex, the use of corticosteroids may be indicated. In addition, calcium supplements may be prescribed.
Local treatment of allergic cheilitis includes the use of a variety of emollient oils, ointments and balms based on sea buckthorn, vitamin E and others. To avoid the recurrence of the pathology, it is necessary to take an allergy test in order to eliminate any contact with the allergen in the future. It is also advisable to reconsider your diet and carefully consider the choice of cosmetics.
Glandular
The main difference between glandular cheilitis is the presence of small red dots (enlarged hypertrophied salivary glands) on the red border of the lips. Droplets of salivary fluid are constantly released from these channels, which irritate the skin and provoke an inflammatory process, as well as drying out of the epithelium, the formation of cracks and erosions.
The disease itself appears as a result of gene abnormalities, or against the background of serious diseases. Treatment with drugs rarely gives a positive result, so most often the hypertrophied glands are removed surgically.
Prevention
The main prevention of cheilitis is maintaining a healthy lifestyle and timely treatment of any infectious and allergic diseases. Basic list of measures:
- Eat right - a balanced menu should contain an abundance of fruits, vegetables, herbs, nuts, fish, and high-quality dairy products.
- Reduce the use of cosmetics - try to choose hypoallergenic formulations and constantly monitor the skin's reaction.
- Dose your exposure to open wind or direct sunlight.
- Protect your lip skin from physical and chemical damage.
- Take vitamin and mineral complexes periodically in courses (after consultation with your doctor).
- Give up bad habits.
- Seek medical advice promptly if you have characteristic symptoms.
Remember: your health is the greatest value, and constant monitoring of its condition is very important to maintain the body’s performance, especially in old age.
Diagnosis of cheilitis
There are no specific laboratory tests to detect cheilitis. All diagnosis of the disease is carried out by visual examination. To determine the causes of inflammation, diagnostics of the gastrointestinal tract may be prescribed for the presence of Crohn's disease or ulcerative colitis. Additionally, allergy tests are performed to exclude food allergies.
General laboratory tests allow you to check the condition of the body and determine the possible causes of cheilitis:
- low levels of vitamins due to hypovitaminosis can provoke exfoliative cheilitis;
- bacterial cultures of smears and biopsies are performed in patients with immune system disorders in the absence of results from the treatment;
- testing for markers of HIV infection, herpes, the presence of fungal or bacterial microflora, respectively, allows us to identify the viral, bacterial or fungal causative agent of cheilitis;
- a blood test for anemia, ESR are required to assess general health;
- examination of the function of the thyroid and pancreas for endocrine pathologies.
On a note! Cheilitis tends to be chronic with periodic relapses. Self-healing without medical supervision is almost impossible, so try to pay attention to such a “minor” problem and consult a specialist. Diagnosis of the disease is carried out by a general practitioner or attending dentist. In some cases, consultation with an allergist, infectious diseases specialist, dermatovenerologist or gastroenterologist may be required.
Treatment of cheilitis
This disease requires special treatment, depending on the cause, type and degree of the inflammatory process. The main methods of treating cheilitis:
- local treatment of the surface of the skin of the lips with disinfectant solutions, ointments, vitamin oil solutions;
- physiotherapeutic methods: Bucca radiation, ultrasound, laser therapy;
- a course of vitamin therapy;
- rinsing the mouth with decoctions of medicinal herbs.
If necessary, to eliminate the causes of the disease, specialized specialists may be involved: a dermatologist, an allergist, an infectious disease specialist.