Is it possible to combine paracetamol and ibuprofen and how to do it correctly?
Of course, it is not recommended to drink ibuprofen and paracetamol together at the first onset of pain. They can be combined only if you have a high body temperature or pain for a long time.
The combined use of paracetamol with ibuprofen means that you first need to take a paracetamol tablet of the dosage prescribed by the doctor or indicated in the instructions. Then, after 6 hours, take an ibuprofen tablet at your prescribed dosage.
You can take paracetamol and ibuprofen at the same time for no more than 3 days. Under no circumstances should you take two tablets of these medications at one time.
The use of paracetamol and ibuprofen not according to the above rules can lead to hepatotoxicity (toxicity to the liver, leading to its structural and functional disorders) and other side effects.
Side effects from improper simultaneous use of paracetamol and ibuprofen can be as follows:
- nausea and vomiting;
- bloating, diarrhea, or constipation;
- itching or rash;
- liver damage and liver failure;
- difficulty breathing, shortness of breath;
- headache or stomach pain.
In individual cases, this list may be quite wider, so it is best to consult your doctor for advice.
Attention! Children can be given paracetamol and ibuprofen only as prescribed by a doctor and only in the form and doses indicated in the prescription.
Paracetamol and ibuprofen should be stored according to the instructions and out of the reach of children, and the drugs should be used only as directed.
Before combining these medications, consult your doctor regarding individual tolerance, dosage, time and duration of use. Stay healthy and do not self-medicate, as this may harm your health.
Have you already packed your fall first aid kit? If not, then we suggest you read a new article from which you can find out what you need to put in your home medicine cabinet .
We also reveal the big secret of online pharmacies and not only them, namely, we tell you what generic drugs are and why they are cheaper .
apteka24.ua is the first online pharmacy you can trust.
Sources
Paracetamol: not as safe as we thought? A systematic literature review of observational studies / Bmj.com (English)
Non-steroidal anti-inflammatory drugs (NSAIDs): Making safer treatment choices / Bpac.org.nz
OARSI recommendations for the treatment of osteoarthritis of the hip and knee osteoarthritis / Oarsijournal.com (English)
Denial of responsibility
apteka24.ua provides comprehensive and reliable information on issues of medicine, health and well-being, however, diagnosis and choice of treatment methods can only be made by your attending physician! Self-medication may be unsafe for your health. apteka24.ua is not responsible for possible negative consequences arising from the use by users of apteka24.ua of the information posted on the site.
When you have a headache, a fracture, or a fever, the pain is sometimes so intense that you wonder when it will all end.
Paracetamol and ibuprofen are effective painkillers, but not everyone can take them, and some people are advised to stay away from them altogether.
In addition, someone may take these medications at the same time, and for others this is very dangerous.
New data from pharmacy company LloydsPharmacy shows that the majority of Britons experience some form of physical discomfort at least once a day, but only one in five (22%) do nothing to relieve the pain.
In this article, we'll tell you everything you need to know about mixing medications for pain relief.
Can I take paracetamol and ibuprofen together?
The National Health Service (NHS) says that if you are over 16, it is safe to take paracetamol and ibuprofen together. You can take both tablets at the same time or one at a time.
For example, if you need to take your medication every four hours, you can take different pills at two-hour intervals.
However, the health service advises to think carefully about whether you need both drugs, and to contact your doctor if you take the tablets on your own for more than three days.
Both drugs can be safely mixed with alcohol, although it is unlikely that it will be useful to drink a lot if you are not feeling well. There are also over-the-counter medications that combine paracetamol and ibuprofen, so you won't need both medications in this case.
WeChat 11/14/2021 Sözcü 02/28/2021 Nihon Keizai 04/12/2020
What is the difference between paracetamol and ibuprofen?
The main difference between the two drugs is that ibuprofen has anti-inflammatory properties, while paracetamol does not.
Both drugs can be taken every four hours for pain relief and as an antipyretic.
Ibuprofen is more effective in reducing inflammation, which is why it is called a non-steroidal anti-inflammatory drug.
Inflammation occurs for various reasons. It may be a sign of infection, or it may occur in the body as a reaction to injury. Ibuprofen is taken to relieve arthritic pain, menstrual pain, back pain, or toothache. It relieves swelling caused by sprains or muscle strain. However, the health service recommends waiting a couple of days before taking this drug so as not to slow down the recovery process.
Another important difference is that ibuprofen should not be taken on an empty stomach, as this drug causes irritation of the mucous membrane and can cause ulcers or bleeding.
Ibuprofen is most effective when taken with or immediately after a meal.
Paracetamol does not need to be taken after meals and is also safe when taken with other medicines.
When should you not take paracetamol and ibuprofen together?
Paracetamol and ibuprofen should not be given together to children.
The National Health Service advises changing your painkiller if it is not helping, and this should be done at the next time you take your medication.
Who should not take painkillers?
The body also breaks down ibuprofen and paracetamol differently. Some people cannot take ibuprofen at all. Among them:
- those who have an allergic reaction to ibuprofen or any other medicines
- people who experience allergy symptoms such as wheezing, runny nose, or skin rash after taking aspirin or some other non-steroidal anti-inflammatory drug
- women trying to get pregnant or already pregnant
- people with high blood pressure that they do not control
Before taking ibuprofen, you should tell your doctor or pharmacist:
- whether you have stomach bleeding, stomach ulcers or perforation of the stomach
- diseases associated with frequent bleeding
- liver problems such as fibrosis, cirrhosis or liver failure
- cardiovascular diseases or acute heart failure
- kidney failure
- Crohn's disease or ulcerative colitis
- chickenpox or shingles - because in this case, taking ibuprofen increases the chance of certain infections and skin reactions.
What are the side effects of paracetamol and ibuprofen?
Paracetamol rarely causes side effects if taken in the right doses. However, the health service says it can cause:
- an allergic reaction resulting in rash and swelling
- flushing, low blood pressure and rapid heartbeat - sometimes this happens in the hospital when the patient is given paracetamol intravenously
– blood diseases such as thrombocytopenia and leukopenia
- damage to the liver and kidneys in case of overdose, and in severe cases death is possible
WeChat 09/19/2021 Sabah 10/02/2021 Wirtualna Polska 03/14/2021
Side effects from taking too much ibuprofen include:
- painful condition
- stomach pain
- fatigue and drowsiness
- black stool and the presence of blood in the vomit, which indicates gastric bleeding
- ringing in the ears
- difficulty breathing, changes in heart rate
If you experience any of these side effects that you think are caused by paracetamol or ibuprofen, you should contact your doctor or pharmacist.
People over 65 also have an increased risk of stomach ulcers if they take ibuprofen. Therefore, they are advised to refrain from taking this drug if they have chronic diseases.
Pregnant women should also avoid taking ibuprofen if possible. In general, they are advised to take paracetamol.
But you also need to use paracetamol carefully.
In 2022, the University of Edinburgh conducted a study that found that both painkillers, when taken during pregnancy, could negatively affect the fertility of future generations because they reduce the number of cells in the fetus that produce sperm and eggs.
How long should there be between taking paracetamol and ibuprofen?
For paracetamol, the usual dose for an adult is one or two 500 mg tablets, taken up to four times a day. The interval between taking tablets should always be four hours.
The usual dose of ibuprofen for an adult is one to two 200 mg tablets taken three times a day. In some cases, the doctor may increase the dose to 600 mg, which should be taken four times a day if necessary. If you take ibuprofen three times a day, leave at least six hours between doses. But, if you have four doses a day, the interval between doses will be four hours.
For those who have persistent pain, your doctor may recommend long-acting ibuprofen tablets or capsules. The drug in this form is usually taken once a day in the evening or twice a day. If you take the medicine twice, you should leave a gap of 10-12 hours between doses.
What happens if you take too much paracetamol or ibuprofen?
Taking too much paracetamol or ibuprofen can be dangerous. Do not rush to double the dose if you feel severe pain.
If you realize that you have taken too much of this drug, consult your doctor immediately. At the same time, do not drive yourself - ask someone else to drive you or call an ambulance. Take the pill bottle or instructions and any remaining medicine with you.
How many days in a row can you take paracetamol or ibuprofen?
When taking ibuprofen tablets, doctors recommend taking the minimum dose, and for the shortest possible time.
If the pain is fleeting (toothache, pain during menstruation), you need to take the medicine for a day or two.
Do not take the drug for more than 10 days unless your doctor advises. Without a doctor's recommendation, use ibuprofen in the form of a gel, mousse or spray for no more than two weeks.
If you have a long-term health problem, such as rheumatoid arthritis, you may need to take ibuprofen for longer. When a person has to take ibuprofen for more than six months, the doctor may recommend additional medicine to protect the stomach from side effects.
As for paracetamol, its daily dose should not exceed eight tablets.
If the symptoms for which you are taking the medicine do not improve within three days, you should contact your doctor or call the NHS on 111.
InoSMI materials contain assessments exclusively of foreign media and do not reflect the position of the InoSMI editorial staff.
New opportunities in the treatment of headaches in general medical practice
Headache (HE) is the most common complaint in medical practice among patients with a wide variety of diseases. It should be noted that out of fifty different diseases, headache can be the leading (and sometimes the only) complaint. HD is widespread, occurring, according to various sources, in 50–85% of residents of different ages, and its occurrence and development can be determined by both somatic and mental factors. Up to 50% of all consumers resort to self-medication for headaches [1].
All this makes us consider the problem of diagnosing and treating hypertension as a general medical, interdisciplinary task that deserves the attention of doctors of all specialties, a task, primarily for specialists in general medical practice.
The frequency and intensity of headaches are variable, usually distinguished:
- rare (no more than 1 time per month/12 times per year) - 60% of cases;
- episodic (several times a month) - 37% of cases;
- daily (or almost daily) - 2-3% of cases of headache sufferers.
In order to study the prevalence and frequency of hypertension, 578 adolescents aged 14–17 years (average age 16.1 years) were studied who underwent a routine medical examination in the 2014–2015 academic year in a large urban clinic in the metropolis with the involvement of specialized specialists (girls accounted for 55.7% , boys - 44.3%).
All patients were asked to answer four questions:
1) Have you experienced headache at least once in your life? 2) If yes, how often (several times in life, several times a year, several times a month, almost daily)? 3) Have you consulted a doctor about hypertension? 4) Do you use any painkillers to relieve headaches (no, several times a year, several times a month, constantly when headaches occur).
The survey results were as follows: 496 adolescents (85.8%) reported that they had experienced headache at least once in their life. 82 respondents (14.2%) denied the occurrence of hypertension during their lifetime.
Of the subgroup of adolescents familiar with the phenomena of headache (496 cases - 100%), 40.7% (202 cases) of those examined reported that they had experienced headache several times in their lives; 28.6% (142 cases) - several times a year; 29.5% (146 cases) - several times a month and 1.2% (6 cases) - almost daily. Among this subgroup of adolescents, 11.7% (58 cases) reported that they had previously consulted a doctor about hypertension. In order to relieve the headache that occurred, 58.1% (288 cases) took painkillers, 14.1% (70 cases) did this several times a year, 34.1% (169 cases) took several times a month, and 9.9 % (49 cases) used drugs continuously during each headache attack.
Thus, despite their young age, adolescents (more than 4/5) are already familiar with the phenomena of hypertension. A third of these patients experience headaches several times a month or more often.
In order to establish the cause of headache, 168 patients (112 women and 57 men), whose average age was 38.7 years, were examined, who complained of headache to the advisory center of the city neurological hospital of a large regional city for outpatient care during 2014 and the first half of 2015 gg. As a result of the examination, it was found that the most common cause, noted in almost half of the examined (47% - 79 cases), was tension headaches (TTH), migraine cephalgia was recorded half as often (21.4% - 36 cases), characteristically, that migraine was always more pronounced, was much more difficult for the patient to tolerate, and was perceived and assessed by him as a “severe headache.” In the remaining patients (31.6% - 53 cases), headache was regarded as symptomatic, several patients were referred for further examination to clarify the diagnosis.
Thus, due to the fairly high probability of occurrence of tension-type headaches and migraine attacks in the population, attention should be focused on them when choosing treatment tactics.
It should be noted that the diagnosis between primary and secondary headaches is of fundamental importance for the choice of therapy (Fig. 1).
Tension headache
A tension headache occurs at least once in every person’s life. There is an episodic form of TTH - it can last from several hours to 7-15 days - and a chronic form of TTH - recorded up to 180 days a year. One of the most common causes of tension-type headache is the so-called “office syndrome” (this is facilitated by: incorrect posture during prolonged work at the computer, stress, sleep disturbance, lack of rest, etc.) [2]. Researchers attribute particular importance to the “muscle factor” in the occurrence of tension-type headaches, since incorrect posture that accompanies stress can cause muscle tension [2–4]. Because as a result of prolonged muscle tension, pressure points, or “trigger points,” are formed in the muscles, leading to the local synthesis of inflammatory mediators - prostaglandins. In turn, peripheral nerve endings become more sensitive to pain impulses, and increasing pain signals lead to the perception of these processes in the form of referred tension headache [2, 4–5].
TTH usually has a painful “aching” character, covers the entire head, and is sometimes accompanied by a feeling of nausea, dizziness and/or other signs of emotional disorders (increased irritability, decreased mood, fatigue, poor sleep, severe autonomic disorders, etc.).
Diagnostic criteria:
- Localization: diffuse, bilateral with severity in the occipital-parietal or parietal-frontal regions.
- Character: monotonous, squeezing (like a “helmet”, “helmet”, “hoop”), practically never pulsating.
- Intensity: moderate, less often intense, usually does not increase with physical activity.
- Accompanying symptoms: soreness of the pericranial muscles and muscles of the collar zone, neck, shoulder girdle and loss of appetite (often), nausea, photo- or phonophobia (rarely).
- Combination with other algic syndromes (cardialgia, abdominalgia, dorsalgia, etc.) and psychovegetative syndrome, with a predominance of emotional disorders of a depressive or anxiety-depressive nature.
Migraine
Migraine is a periodically recurring paroxysmal condition, manifested by attacks of intense headache of a pulsating nature, in one (rarely in both) half of the head (mainly in the frontal-temporal-parietal-orbital region) in combination with other non-painful manifestations (nausea and/or vomiting, intolerance bright lights, loud noises, emotional disturbances, aura symptoms, drowsiness and lethargy after an attack). The possible duration of an attack is from 1–2 to 72 hours.
There are migraine without aura (simple migraine) and migraine with aura (classic). An aura is a complex of neurological symptoms that occurs immediately before or at the very beginning of a migraine headache.
Auras are distinguished: ophthalmic - with visual disturbances (zigzags, sparks, flickering spiral-like contour); hemiparesthetic - paresthesia or a feeling of numbness that occurs locally and slowly spreads to half the body; paralytic - in the form of unilateral weakness in the limbs; aphasic - in the form of speech disorders, etc. It should be remembered that migraine can have complications: status migraine (duration of attack more than 72 hours) and migraine stroke.
Diagnostic criteria
Migraine without aura
- Headache has at least two of the above symptoms (unilateral localization; pulsating nature; moderate or significant intensity of headache, reducing the patient’s activity; headache worsening during monotonous work or walking).
- At least five “attacks” of headache, with each duration (without treatment or with unsuccessful treatment) from 4 to 72 hours.
- The presence of at least one of the accompanying symptoms (nausea, vomiting, sensitivity to light and/or sound).
Migraine with aura
- GB has a minimum of 2 attacks (meeting the criteria for “Migraine without aura”).
- Migraine attacks have: complete reversibility of one or more aura symptoms; none of the aura symptoms last more than 60 minutes; the duration of the “light” interval between the aura and the onset of headache is less than 60 minutes.
Treatment of headache
In the treatment of hypertension, various types of medications are used, the most frequently used of which are the most accessible to patients - simple (non-narcotic) analgesics and non-steroidal anti-inflammatory drugs (NSAIDs). From the group of NSAIDs, ibuprofen is most often used in the treatment of hypertension, and from the group of non-narcotic analgesics - paracetamol.
General criteria for choosing NSAIDs in the treatment of hypertension are: rapid action (complete cessation of headache); effectiveness (no recurrence of headache); safety and good tolerability. It was the selection criteria that formed the current recommendations for choosing NSAIDs in the treatment of hypertension: it is more effective to use analgesics at the beginning of an episode of headache, using fast-acting forms of analgesics; and also use the maximum initial dosage in order to prevent relapse and repeated use for the prevention of abuse headaches, it is necessary to limit the doses of analgesics containing barbiturates - up to 4 times a month, simple analgesics and NSAIDs - up to 15 doses per month, and also limit drugs with caffeine content, avoid drugs containing metamizole sodium) [6–7].
Treatment of tension-type headache
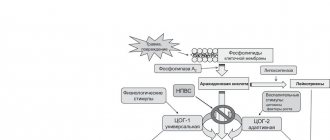
When treating TTH, it should be remembered that the source of TTH is the release of prostaglandins, key mediators of inflammation. Therefore, the choice of drug for the treatment of tension-type headache is aimed at its cause, at suppressing the synthesis of prostaglandins. Based on the mechanism of action, NSAIDs are the first choice drugs for the treatment of TTH [4, 14–16].
Thus, when studying the comparative effectiveness of treating TTH with drugs, ibuprofen proved its effectiveness on a par with other NSAIDs (Diclofenac, Naproxen, Ketoprofen); it was proven [17–18] that ibuprofen brings significant relief in TTH within 30 minutes after its administration to a larger number of patients (20% of cases) than paracetamol (12.5% of cases). And it is ibuprofen that provides complete relief of TTH 3 hours after its administration in the majority of patients (75%), compared with paracetamol (32%) [19].
The new original drug Nurofen Express forte is presented in a unique format (capsules with a liquid center), thanks to which the drug has high absorption, and its maximum concentration in the blood (Tmax) is achieved in 30–40 minutes. The enhanced formula contains ibuprofen - 400 mg and targets the source of pain. Currently, the drug Nurofen Express forte is considered the best drug in the Nurofen “line”; it is recommended for use from the age of 12, which is important, given the frequency of headaches in adolescence.
Nurofen Express forte 400 mg begins to eliminate headaches after 15 minutes [20], and its fast-acting form and dosage of 400 mg has the highest efficacy rate, since the earliest achievement of a high concentration of ibuprofen in the blood leads to faster pain relief [21].
Nurofen Express forte (400 mg) has a more pronounced analgesic effect than 1 gram of paracetamol [22–23], or a low dose of ibuprofen (200 mg) compared to an average dose of acetylsalicylic acid (500 mg) [24].
When comparing the risks of adverse events, as well as toxicity in the gastrointestinal tract, Nurofen Express forte with other drugs that aggressively affect the gastrointestinal mucosa (piroxicam, ketoprofen, indomethacin, diclofenac, naproxen, acetylsalicylic acid), showed a high safety profile, accordingly, the lowest risk for undesirable consequences [25–26].
Thus, the drug Nurofen Express forte meets all the criteria for choosing an NSAID: namely “Fast” (begins to act after 15 minutes); “Effectiveness” (contains an effective dose of 400 mg of ibuprofen in one capsule with a liquid center); “Safety” (has the most favorable safety profile among NSAIDs). Nurofen Express forte, according to European standards, can be recommended as the first choice drug for headaches [14–15, 27–30].
Migraine treatment
Migraine, although it ranks second in prevalence, is, however, more pronounced in terms of severity of manifestation and subjectively difficult to tolerate for headache sufferers.
During clinical studies, it was noted that the optimal result in relieving hypertension is achieved by a combination of ibuprofen and paracetamol, which is widely used and considered safe in appropriate doses [8–9]. It is important to note that pharmacokinetic interactions between ibuprofen and paracetamol have not been documented, and no additive effects have been observed from the combined use of these two drugs [10–11].
Ibuprofen and paracetamol are reasonably considered to be relatively safe with a proven analgesic effect, which allows their use in multicomponent analgesics [9, 12–13]. At the same time, a combined drug of ibuprofen and paracetamol allows not only to use the advantages of the two drugs, but also to avoid the disadvantages and dangers of independent combined prescription of NSAIDs [10–11].
In this regard, the drug Nurofen MultiSymptom is interesting, which relatively recently appeared in the Nurofen “line” and is positioned as a “special remedy for migraines”, since its high effectiveness (in terms of the speed of onset of therapeutic effects and elimination of the severity of headache symptoms) is associated with a successful combination of its constituents components: ibuprofen - 400 mg and paracetamol - 325 mg. These components affect the central and peripheral mechanisms of pain syndrome formation and have a rapid, pronounced analgesic effect [9, 12], since it is the combination of ibuprofen and paracetamol that provides a higher analgesic effect due to the combined inhibition of COX types 1–2, which is noticeably superior in effectiveness NSAID monotherapy. The results of randomized, double-blind, placebo-controlled studies for the treatment of acute pain give grounds to conclude that the drug is superior in analgesic efficacy, duration of action and time of development of analgesia to its individual ingredients and placebo [9, 12–13]. It is worth noting that both components of the drug Nurofen MultiSymptom are recommended by the European Neurological Federation and the American Society for the Study of Hypertension as the drugs of choice for the relief of migraine attacks; in addition, studies show that repeated use of the drug is required much less frequently, and the rate of recurrence of a migraine attack is significantly lower [9 , 12–13].
It should also be understood that in relieving hypertension, the use of any drug is more effective if treatment is started earlier (for migraine with aura - at the stage of aura appearance, for simple migraine - from the moment the headache appears), at the height of the attack - most medications are ineffective.
Thus, the attention of doctors should be focused on the use of drugs in the most favorable period, from the point of view of prognosis. It is during this period that non-narcotic analgesics and non-steroidal anti-inflammatory drugs are effective in many patients with rare migraine attacks.
Despite the fact that the use of triptans is currently considered one of the promising areas in the treatment of migraine, it is difficult to use these drugs in general medical practice (especially in underexamined patients). In most cases, one should resort to a stratified approach “from simple to more complex”; this gives every reason to use an effective combination of NSAIDs and analgesics for migraine headaches (Fig. 2).
It is known that significant disadvantages of triptan therapy are:
- Possibility of prescribing only with a confirmed diagnosis of migraine;
- contraindication for use during aura and more often than 9 days a month;
- ability to cause dependence;
- prescription dispensation.
In studies where ibuprofen 400 mg was used to treat migraine, it reduced nausea and vomiting, this is likely due to ibuprofen's ability to reduce platelet aggregation or prostaglandin synthesis, both of which are involved in the development of migraine symptoms [31].
conclusions
- HD occurs quite often in the population, regardless of gender and age.
- Among primary headaches, tension headache is the leader, and migraine is the second most common headache.
- The new drug Nurofen Express forte can be considered as the first choice drug for tension-type headache, which has a highly effective, rapidly onset (begins to act within 15 minutes) effect with a proven most favorable safety profile among NSAIDs, and the use of which is an ideal solution for tension-type headache.
- The new drug Nurofen MultiSymptom contains a combination of ibuprofen and paracetamol in doses that reliably relieve a migraine attack faster and more effectively compared to the individual components of the drug [9, 12, 13], which makes it possible to talk about an effective solution to the problem of migraine, and the components contained in it (ibuprofen and paracetamol) correspond to a high level of evidence of effectiveness and are recommended as the drugs of choice for the treatment of migraine.
Literature
- World Health Organization. Atlas of headache disorders and resources in the world 2011. A collaborative project of World Health Organization and Lifting The Burden, 2011. Available at: https://www.who.int/mental_health/management/atlas_headache_disorders/en/. Accessed May 2014.
- Bendtsen L., Fernández-de-las-Peñas C. // Curr Pain Headache Rep. 2011; 15: 451–458.
- Abboud J. et al. Cephalalgia. 2013. Fernández-de-la-Peñas C. et al. Cephalalgia. 2007.
- Fernández de las Peñas C. et al. // Cephalalgia. 2007; 27: 383–393.
- Jensen R. // Cephalalgia. 1999; 19: 602–621.
- Bendtsen L., Evers S., Linde M. et al. EFNS guideline on the treatment of tension-type headache 2010.
- Sarchielli P. et al. // J Headache Pain. 2012.
- Moore RA, Derry CJ, Derry S., Straube S., McQuay HJ A conservative method of testing whether combination analgesics produce additive or synergistic effects using evidence from acute pain and migraine // European Journal of Pain. 2012; 16(4):585–591.
- Derry CJ, Derry S., Moore RA Single dose oral ibuprofen plus paracetamol (acetaminophen) for acute postoperative pain // Cochrane Database Syst Rev. 2013, Jun 24; 6.
- Rainsford KD, Roberts SC, Brown S. // J. Pharm. Pharmacol. 1997, 49, p. 345–376.
- Frank de Vries et al. // Br J Clin Pharmacol. 2010, 70: 3, 429–438, 4291.
- Baranova L.N. et al. // Pharmateka. 2012, no. 5.
- Nikoda V.V., Mayachkin R.B. // Therapeutic archive. 2005, November.
- Steiner T. et al. // J Headache Pain. 2007; 8:S 1–47.
- Bendtsen L. et al. // Eur J Neurol. 2010; 17: 1318–1325.
- Burian M. et al. // Pharmacol Ther. 2005; 107:139–154.
- Kubitzek F. et al. // Eur J Pain. 2003; 7: 155–162.
- Lange R. et al. // Drugs Exp Clin Res. 1995.
- Packman B. et al. // J Headache. 2000; 40:561–567.
- Schachtel B. Thoden W. // Headache. 1988; 28:471–474.
- Moore A. et al. // Pain. 2013.
- Schachtel B. et al. // J Clin Pharmacol. 1996; 36:1120–1125.
- Packman B. et al. // J Headache. 2000; 40:561–567.
- Nebe J. Heier M., Diener HC // Cephalalgia. 1995.
- Henry D. et al. // Int J Clin Pract Suppl. 2003; 135:43–49.
- Fries JT et al. // Arthritis Rheum. 1991, Nov; 34(11):1353–1360.
- British Association for the Study of Headache (BASH). Guidelines for all healthcare professionals in the diagnosis and management of migraine, tension-type headache, cluster headache and medication-overuse headache. 3rd edition (1st revision). 2010.
- Haag G. et al. // J Headache Pain. 2011; 12: 201–217.
- NICE. Headaches — diagnosis and management of headaches in young people and adults. NICE clinical guideline 150. Issued September 2012.
- Bendtsen L. et al. // J Headache Pain. 2012; 13(Suppl 1):S 1–29.
- Pearce, Franketal - 1983.
V. G. Moskvichev*, Candidate of Medical Sciences Yu. G. Petrova**, Candidate of Medical Sciences R. M. Mamin***
* GBUZ PKB No. 4 named after. P. B. Gannushkina DZM, Moscow ** State Budgetary Healthcare Institution JSC City Clinical Hospital No. 5, Astrakhan *** State Budgetary Educational Institution of Higher Professional Education of the State Medical University "MSCh", Astrakhan
Contact Information
Ibuprofen, cortisone or paracetamol? What will help in the fight against coronavirus
The French Ministry of Health said that when infected with coronavirus, it is strictly forbidden to use a number of anti-inflammatory drugs, as they can only worsen the patient’s condition. We are working with Russian experts to find out whether such medications can really cause complications and in what cases it is necessary to take paracetamol.
Dangerous drugs?
French Health Minister Olivier Veran said on his Twitter page that taking a number of anti-inflammatory drugs like ibuprofen or cortisone can be a factor that worsens the infection. “If you have a fever, take paracetamol,” he advised.
However, some Russian experts do not share this opinion. In particular, clinical virologist Georgy Vikulov, in a dialogue with Moscow 24, said that to date there are no studies confirming this. “Ibuprofen and paracetamol are non-steroidal anti-inflammatory drugs. They are allowed in certain dosages as antipyretics, recommended by WHO and leading specialized organizations both abroad and in Russia.”
“, the specialist explained. Regarding COVID-19, there are no studies whose results would indicate that ibuprofen and paracetamol should not be used.
Vikulov added that paracetamol and ibuprofen are allowed both in the treatment of children and pregnant women. “When an antipyretic effect is required, nothing is more effective than non-steroidal anti-inflammatory drugs”
, the expert believes.
At the same time, the virologist confirmed the negative consequences for the body after using cortisone. “Cortisone, corticosteroids, and cortisone-related substances are not recommended because they cause significant immune suppression.”
, says Vikulov.
According to the specialist, any hormonal drugs are dangerous for any viral infections. And COVID-19 is no exception.
When and how can you take paracetamol?
Today, people often abuse antipyretic and anti-inflammatory drugs because such drugs are actively advertised, experts believe. At the same time, the decision on the use of such drugs and their dosage should be made by the attending physician, emphasized clinical virologist Georgy Vikulov. Paracetamol can only be used as prescribed by a doctor. If there are indications for use, he will recommend non-steroidal anti-inflammatory drugs with antipyretic or anti-inflammatory effects, depending on what is required.
Professor of the Department of Hospital Therapy of the First Moscow State Medical University named after I.M. Sechenov Sergey Yakovlev
said that antibiotics are used to combat bacterial pneumonia. But if pneumonia is caused by viruses, including coronavirus, then antibiotics are useless. Antibiotics have no effect on the virus. And to prevent this coronavirus, you don’t need to take any medications, they are pointless.
In addition, Yakovlev
reminded that any medicine can have side effects. Starting from allergic reactions and ending with damage to the liver, kidneys and other organs. Therefore, you should not abuse self-medication. The main thing is to remember about hand hygiene and follow the recommendations of the Ministry of Health and Rospotrebnadzor on the prevention of coronavirus.
Virologist Georgy Vikulov also added that antibiotics should be prescribed only by doctors after examination and consultation. “The sale of antibiotics in a pharmacy without a doctor’s prescription is a violation of the federal program to combat the spread of antibiotic resistance in the Russian Federation until 2030,” the specialist emphasized. Moreover, if you use antibiotics with or without reason, then at the moment when such a medicine is really needed, it simply will not work. Professor of the Department of Hospital Therapy at the First Moscow State Medical University named after I.M. Sechenov Sergei Yakovlev explained that in case of severe fever (temperature more than 39 degrees), it is necessary to reduce the temperature, especially in children. “Paracetamol in this regard is the most neutral and safe, so it will be optimal”
, says Yakovlev. However, he also emphasized that a doctor should prescribe the medicine.
More details: https://www.m24.ru/articles/obshchestvo/18032020/156530?utm_source=CopyBuf
Grodno Regional Children's Clinical Hospital
Details Published August 22, 2019
PARACETAMOL? IBUPROFEN? IBUKLIN?
Antipyretic medications for children are available under different commercial names and in a variety of dosage forms: syrups, tablets, suspensions, rectal suppositories.
But all antipyretic drugs are one way or another divided into two groups, where the active ingredients are paracetamol and/or ibuprofen.
How to figure it out? What to choose? Especially when there is no doctor nearby.
PARACETAMOL
— first choice antipyretic drug
— registered in USA in 1953
- used almost from birth
- a pure antipyretic drug, not an analgesic
- acts gradually, the effect takes place after 30-40 minutes, but its effect lasts for about 4 hours.
— few contraindications, but cannot be used for liver, kidney diseases, viral hepatitis, diabetes mellitus
- is a “secret indicator” of the disease: in most viral infections it effectively reduces high fever, in bacterial infections it is worse.
- in case of overdose - hepatotoxic
- available without a doctor's prescription!!
— available in various convenient dosage forms (rectal suppositories, syrups, suspensions, tablets)
IBUPROFEN
- an antipyretic drug of the second choice, especially if you are allergic to paracetamol.
— registered in Great Britain in 1962.
- used from 3 months of age in the form of syrup, in the form of tablets - from 6 years of age
- has an analgesic effect, the antipyretic effect may not be as effective.
- antipyretic effect develops after 30 minutes
- the duration of action is about 6 hours, so it is better to prescribe it for antipyretic purposes at night
- irritates the gastrointestinal tract, many side effects
- according to Danish scientists, regular use of ibuprofen can cause infertility in men in the future
- available without a doctor's prescription
IBUCLIN - a combination of paracetamol and ibuprofen
- combination of antipyretic and analgesic effects
- many contraindications!!!
- cannot be used for a long time
- Available in tablets and syrup
- contraindicated in tablets for children under 3 years of age, in syrup - up to 2 years of age
- available with a doctor's prescription
THE BEST “medicinal” solution: for antipyretic purposes, use the safer PARACETAMOL; if you are intolerant to PARACETAMOL, use IBUPROFEN; in special cases, it is possible to alternate PARACETAMOL and IBUPROFEN, no more often than every 4-6 hours.
To the above, it is worth adding that Ibuprofen, Ibuklin and even Paracetamol are incompatible with sweet carbonated drinks. The fact is that carbon dioxide and acid, which are found in carbonated waters (drinks), increase the absorption of the drug in the blood, thereby increasing their concentration in the body. In this case, it is almost impossible to control the dosage of the drug; small doses do not have the desired effect and there is a possibility of an overdose of the antipyretic drug.
When using medications to treat fever, parents should remember:
- Don't overheat your baby! (access to fresh air, open windows, do not wrap yourself in clothes)
- Provide your child with enough fluids! (preferably drink clean water)
- Do not force feed a child during a fever!
- There is no need to bring down the high temperature to normal numbers, it is enough to feel good.
Head reception department Vorontsova O.M.
Lecofen Combo tab 200 mg+500 mg 10 pcs
Pharmacological group:
Combined analgesic (NSAID + non-narcotic analgesic).
ATX code: M01AE51. Pharmacodynamics:
A combined drug whose effect is determined by its constituent components. It has a targeted effect against pain (analgesic), antipyretic and anti-inflammatory effect. Ibuprofen and paracetamol differ in their mechanism and site of action. As a result of their mutually reinforcing action, a more pronounced decrease in pain sensitivity and an increase in antipyretic effect is achieved than individually.
Ibuprofen is a derivative of propionic acid from the group of non-steroidal anti-inflammatory drugs (NSAIDs), has anti-inflammatory, including anti-edematous, analgesic and antipyretic effects. The mechanism of action of ibuprofen is due to inhibition of the synthesis of prostaglandins - mediators of pain, inflammation and hyperthermic reaction, through indiscriminate inhibition of the activity of cyclooxygenase 1 (COX-1) and cyclooxygenase 2 (COX-2). The analgesic effect of ibuprofen is provided by its inhibitory effect at the peripheral level. The antipyretic effect of ibuprofen is associated with central inhibition of prostaglandin synthesis in the hypothalamus. Ibuprofen inhibits the migration of leukocytes to the site of inflammation. In addition, ibuprofen reversibly inhibits platelet aggregation.
Paracetamol is an analgesic non-narcotic drug that has analgesic, antipyretic and weak anti-inflammatory effects. Indiscriminately blocks COX-2, mainly in the central nervous system. Paracetamol can also stimulate the activity of the descending serotonin pathways, which leads to the inhibition of the transmission of pain impulses in the spinal cord. At the peripheral level, paracetamol has a weak effect on COX-1 and COX-2.
The drug Lecofen Combo has a faster therapeutic effect and a more pronounced analgesic effect (reduces pain better) than ibuprofen and paracetamol separately. After taking one tablet, the analgesic effect is observed on average 15 minutes after taking the drug; a clinically significant analgesic effect is achieved after 40 minutes and lasts for 8 hours. After taking two tablets, the analgesic effect is observed on average 18 minutes after taking the drug; a clinically significant analgesic effect is achieved after 45 minutes and lasts for 9 hours.
Pharmacokinetics:
Ibuprofen:
Absorption: absorption is high, quickly and almost completely absorbed from the gastrointestinal tract (GIT). Detected in blood plasma 5 minutes after taking the drug on an empty stomach. The time to reach maximum concentration in blood plasma after oral administration is about 1-2 hours. Taking the drug with food may increase the time to reach maximum concentration by 25 minutes, but the overall extent of absorption is equivalent.
Distribution: connection with blood plasma proteins - 90%. Slowly penetrates into the joint cavity, accumulates in the synovial fluid, creating higher concentrations in it than in the blood plasma. There is evidence that ibuprofen was found in breast milk in trace concentrations.
Metabolism: Metabolized in the liver. After absorption, about 60% of the pharmacologically inactive R-form is slowly transformed into the active S-form.
Elimination: half-life (T1/2) is about 2 hours. It is predominantly excreted by the kidneys in the form of metabolites (no more than 1% unchanged) and to a lesser extent with bile in the form of metabolites and their conjugates. There were no significant differences in the pharmacokinetic profile of ibuprofen in older adults compared to younger adults.
Paracetamol:
Absorption: high absorption, quickly absorbed from the gastrointestinal tract. Detected in blood plasma 5 minutes after taking the drug on an empty stomach. The time to reach maximum concentration in blood plasma after oral administration is 30-40 minutes. Cmax - 5-20 mcg/ml. When taking Lecofen Combo with food, its concentration in the blood plasma is lower, which is achieved 55 minutes later, but the overall degree of absorption is equivalent.
Distribution: binding to plasma proteins is less than 10% when taken in therapeutic doses, increases slightly with overdose. Distributed fairly evenly in body fluids. Penetrates the blood-brain barrier.
Metabolism: about 90-95% of paracetamol is metabolized in the liver to form inactive conjugates with glucuronic acid (60%), taurine (35%) and cysteine (3%), as well as a small amount of hydroxylated and deacetylated metabolites. A small portion of the drug is hydroxylated by microsomal enzymes to form highly active N-acetyl-p-benzoquinone imine, which binds to the sulfhydryl groups of glutathione. When glutathione reserves in the liver are depleted (in case of overdose), the enzyme systems of hepatocytes can be blocked, leading to tissue damage. Excretion: excreted by the kidneys mainly in the form of glucuronides and sulfated conjugates with the formation of about 10% of glutathione conjugates (less than 5% is excreted unchanged). T1/2 - 3 hours.
There were no significant differences in the pharmacokinetic profile of paracetamol in older adults compared to younger adults.
The bioavailability and pharmacokinetic parameters of ibuprofen and paracetamol taken as part of this combination drug do not change with either single or repeated use. The drug is formulated using technology that allows ibuprofen and paracetamol to be released simultaneously, so that the active ingredients provide a combined effect.
Newspaper “News of Medicine and Pharmacy” 19 (293) 2009
Ibuprofen is a drug recommended for the treatment of arthritis in children and is well tolerated. It is also an effective antipyretic [4] and is therefore a potential alternative to paracetamol. A number of previous studies have determined the optimal dosage range for ibuprofen [5]. Many studies comparing ibuprofen and paracetamol excluded young children, children with wheezing and asthma. Accordingly, the aim of the present study was to compare the antipyretic efficacy and tolerability of ibuprofen and paracetamol suspensions in febrile children, including young children and those with typical pediatric illnesses.
Methods
Study design and patients
This work was performed as a double-blind, parallel-group, multi-dose study and was approved by the local bioethics committee. Written informed consent for participation in the study was obtained from parents or legal guardians, as well as from children if they were able to give such consent. All children included in the study were hospitalized in the same hospital, were aged between 2 months and 12 years, of both sexes, and had an axillary temperature of 37.5°C or higher. Children were excluded from the study if their body weight was below the third centile for age, if they were receiving anticoagulant therapy, if they had a history of intolerance to ibuprofen, paracetamol or other similar substances, or if they had previous or current symptoms of peptic ulcers or gastrointestinal tract. intestinal bleeding or had severe diseases of the liver, cardiovascular system, kidneys or systemic diseases, malignant neoplasms. Taking medications that could interfere with the study was stopped at least 6 hours before the start of the study.
At enrollment, the following parameters were recorded: age, sex, weight, primary diagnosis, treatment received during the previous month, and history of asthma, wheezing, or seizures.
The drugs tested were manufactured by Boots Pharmaceuticals as orange-flavored, saccharin-free suspensions. Randomization was performed in a block of 4 patients to achieve an equal number of children in each group. The dosage of the drugs depended on age - for ibuprofen it was approximately 20 mg/kg/24 hours, for paracetamol 50 mg/kg/24 hours - and was prescribed in divided doses. Patients took the drugs orally, every 6 hours as needed, up to four doses every 24 hours, for a maximum of 3 days (12 doses).
Children could be withdrawn from the study at any time if continued participation would be harmful to their health.
Measurements taken during the study
During the first dose, axillary temperature was recorded and then recording continued every hour for 6 hours. After this, the temperature was recorded every 6 hours (that is, immediately before taking each subsequent dose of the tested drugs). After taking the first dose, the palatability of the drugs was assessed by observing the reaction of young children or by taking into account formulated requests if the child was over 7 years old. At the same time, we used a five-point scale from 0 (I didn’t like the taste to a large extent) to 4 (I liked the taste to a large extent). Irritability was assessed using a three-point scale
from 0 (very irritable) to 2 (not irritable). Before taking subsequent doses, changes in clinical status were noted on a five-point scale from 0 (much worse) to 4 (much better), after which irritability, etc. was again assessed. After taking the last dose of the test drug or after resolution of fever, the overall effectiveness of treatment was assessed on a four-point scale from 0 (no effect) to 3 (very good effect). The study documented any adverse effects regarding their nature, cause, and severity.
Statistical processing
The planned sample size was 75 patients in each treatment group: with a power of 90%, a 5% significance level and an estimated variability of 1.07 °C, changes in baseline temperature of more than 0.56 °C could be determined when observing a patient for more than 4 hours. The actual variability during the study was 1.18 °C. All statistical tests were performed as two-tailed and considered significant at the 5% level. The null hypothesis has always been the idea that ibuprofen and paracetamol are equivalent to each other. Two selected groups of children were compared in terms of body temperature at the 4th hour of the study using analysis of covariance, with the assigned treatment used as factors and age as covariates. The magnitude of palatability, changes in irritability and clinical status, and assessment of the overall effectiveness of treatment, expressed on an ordinal scale, were compared between the selected groups using the Wilcoxon rank sum test. The rate of withdrawal of patients from the study and the time during which the temperature decreased below 37.5°C were compared using the log-rank test. The number of patients who developed side effects and the number of patients whose temperature decreased by 1°C or more at 4 hours of observation were compared using the chi-square test.
results
For all 150 children included in the study, it was possible to obtain at least one reliable assessment of the effectiveness of treatment.
The diseases suffered by the children who took part in this study are listed in Table. 1. Demographic and baseline characteristics of patients
The selected groups of children were comparable in age, gender and body weight. In the group of children receiving ibuprofen (42 boys and 34 girls), the median age was 1.8 years (range 0.4–11.6 years), median body weight 11.9 kg (range 6.7–45 kg) ), 20 children were ≤ 12 months of age. In the group of children receiving paracetamol (47 boys and 27 girls), the median age was 1.6 years (range 0.2–9.4 years), median weight 11.9 kg (range 5.8–34 kg) , 20 children were ≤ 12 months of age. At the time of inclusion in the study, 11 patients in the ibuprofen group had a preliminary diagnosis of wheezing, 21 had a history of wheezing and/or asthma; in the paracetamol group there were 4 and 12 such patients, respectively. All 150 children included in the study received at least one dose of the test drugs, although 1 child was unable to swallow the suspension given to him. When included in the study, 25 children in the ibuprofen group and 28 children in the paracetamol group received concomitant therapy in addition to the tested drugs.
Treatment efficacy data
The main results of the study are presented in table. 2. The difference between both treatments in the mean change in body temperature at 4 hours of observation was -0.2 °C (95% confidence interval -0.6 to 0.2, p = 0.39). The largest average decreases in body temperature were observed during the first 5 hours of the study. In the group with ibuprofen, the maximum average decrease in temperature from the initial level was 2 °C at the 3rd hour of the study, and in the group with paracetamol - 1.7 °C at the 2nd, 3rd and 4th hours of the study. Changes in real average body temperature are presented in Fig. 1. After 36 hours of follow-up, very few patients remained in the study, so the average reductions over subsequent time periods are not shown.
During the present study, temperatures fell below 37.5°C in 73 (96%) of 76 patients in the ibuprofen group and 66 (89%) of 74 patients in the paracetamol group. There were no significant differences between both treatment groups in: a) the distribution of time during which the temperature dropped below 37.5 °C (median time was 2 hours for the ibuprofen group and 1.4 hours for the paracetamol group, p = 0 ,25); b) distribution of time elapsed before taking the second dose (median time was 6 hours for both treatment groups, p = 0.44). Only 14 children in the ibuprofen group and 13 children in the paracetamol group received more than 4 doses of the test drugs - most of the other children did not need this due to recovery (in terms of fever) and withdrawal from the study.
Assessment of palatability, irritability, clinical status and overall effectiveness
From the table 2 shows that there are no significant differences between the selected groups, with the exception of changes in irritability. Although the mean change from baseline in irritability in both groups was 0, more children in the paracetamol group showed a decrease in irritability: this parameter was reduced in 21 of 56 (38%) children in the paracetamol and paracetamol group. 9 out of 50 (18%) children in the ibuprofen group (p = 0.047). However, it is necessary to pay attention to the fact that under initial conditions the median irritability in those patients who subsequently took ibuprofen and paracetamol was 2 points (not irritable) and 1 point (slightly irritable), respectively. From this it appears that the positive effect observed in the paracetamol group was due to a greater tendency of the children themselves to improve rather than to any additional benefits of paracetamol.
Among other cooling methods, stripping (removing clothes) was the most frequently used method in both groups of children. This approach was used at least once in 42 (60%) of 70 children in the ibuprofen group and 55 (79%) of 70 children in the paracetamol group.
Tolerability of drugs
A total of 66 (87%) of 76 children receiving ibuprofen and 64 (87%) of 74 children receiving paracetamol were withdrawn from the study due to a decrease in temperature to normal levels. An additional 7 patients treated with ibuprofen and 8 patients treated with paracetamol were withdrawn from the study due to complications and/or lack of efficacy. Of these, 4 patients receiving ibuprofen had the following complications: hives, vomiting, abdominal and throat pain, 1 patient was hospitalized with a diagnosis of “irritable hip” (toxic synovitis - Translator's note), requiring surgical intervention. In 3 patients receiving paracetamol, discontinuation of the study was associated with the following complications: epistaxis, the appearance of purple spots at the site of the blood pressure cuff, meningococcal meningitis. An additional 3 patients in the ibuprofen group and 2 patients in the paracetamol group withdrew from the study for other reasons.
Twenty-one of 150 children in the study experienced 34 complications: 10 of 76 (13%) children in the ibuprofen group had 16 complications and 14 of 74 (19%) children in the paracetamol group had 18 complications. The number of observed complications did not differ significantly between both treatment groups (p = 0.34). Most complications were relatively mild and had a questionable relationship with the treatment, or there was no such relationship at all. Of the 34 complications that developed during this study, 14 were not related to the treatment. Information about the remaining 20 complications is reflected in table. 3.
None of the patients developed asthma attacks during the study, but two patients in the paracetamol group had mild wheezing. One had no history of wheezing but was enrolled in the study with a respiratory tract infection, and the other had a history of wheezing.
Discussion
Despite the arguments of some researchers regarding the positive protective role of fever [6], it is generally accepted that a decrease in temperature does not prolong the duration of the disease or have an adverse effect on its outcome [7]. Along with prescribing the main treatment for the disease that caused the fever, antipyretic drugs are widely used, since they can significantly improve the well-being of children during illness. Therefore, drugs used to reduce fever must be effective and safe. Confidence in paracetamol, the most commonly used antipyretic in children, is associated with extensive experience in its use for this purpose. Aspirin was also used for a long time to reduce fever, but was removed from the list of antipyretics in the United States after reports of a possible connection with the occurrence of Reye's syndrome [2].
Beginning in 1990, ibuprofen became available as an antipyretic agent in children. It is a non-steroidal anti-inflammatory drug and, therefore, may cause gastrointestinal and renal complications [8], and may also be undesirable in patients with asthma [9]. Previous studies have found that ibuprofen has a good safety profile when used in children with juvenile arthritis [10, 11]. Its antipyretic properties were also established [13–15], but in these studies only one dose of the drug was tested and children under 2 years of age were excluded from observation. Those studies that examined different doses of ibuprofen also did not include children under 2 years of age [15, 16]. Many studies excluded children of any age who had wheezing or asthma. The problem, however, is that very often the antipyretic drug must be prescribed to a child under 2 years of age or to children with fever and wheezing due to a respiratory tract infection.
In the present study, we attempted to evaluate the effectiveness and safety of paracetamol and ibuprofen in a manner that reflected the conditions of real medical practice. Children receiving ibuprofen spanned a wide age range (0.4 to 11.6 years); 26% of children were 12 months of age or younger; they had a wide range of conditions typically encountered in pediatric practice, 14% had a primary diagnosis of wheezing/asthma, and 28% had a history of wheezing or asthma.
As a result, paracetamol and ibuprofen were found to be equally effective antipyretics. They tasted the same. Significantly more children receiving paracetamol had reduced irritability. However, this effect appeared to be due to the children themselves being more likely to improve rather than to any additional benefits of paracetamol. At study endpoints, there were no statistically significant differences in changes in clinical status (median 3 points (improved) in both groups) or overall effectiveness (median 2 points (good effect) in both groups). There were no significant differences between the two groups in the number of children who developed complications. In the ibuprofen group, 10 of 76 patients (13%) had 16 complications; in the paracetamol group, 14 of 74 patients (19%) had 18 complications. Complications were mild, and in most cases the relationship with the treatment was questionable or completely absent. Among patients taking ibuprofen, there were no respiratory complications associated with taking this drug. Due to previously raised concerns regarding the use of non-steroidal anti-inflammatory drugs in asthma [9], further research is needed to evaluate the use of ibuprofen in children with wheezing/asthma.
In conclusion, at the doses used, ibuprofen and paracetamol were equally effective and well tolerated in the treatment of fever in young children. Although both treatments have been shown to be equally safe, caregivers must remain vigilant until ibuprofen gains the same credibility as paracetamol.