Materials and methods
The open prospective study included 98 women (mean age 68±9 years, mean duration of postmenopause 17±4 years) with postmenopausal AP, who were observed on an outpatient basis at the National Medical Research Center for Primary Care. In the anamnesis, a fracture of the proximal femur (PHB) was noted in 4, radius - in 8, compression fractures of the vertebrae - in 27. The median 10-year probability of major fractures according to FRAX in patients who had not previously received therapy was 14.9%, fracture femoral neck (FNC) - 3.7% (Table 1).
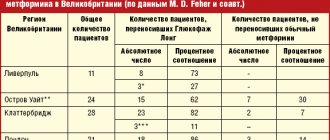
Table 1. Clinical and instrumental characteristics of the examined patients Note. Here and in the table. 2 NPs - those who had not previously taken anti-osteoporotic therapy; P - previously taken anti-osteoporotic therapy.
All patients received denosumab at a dose of 60 mg once every 6 months subcutaneously (in most cases in the abdominal area) for 12 months or more, as well as calcium and vitamin D supplements according to the instructions [12].
Before starting treatment with Prolia, the concentration of vitamin D (25 (OH)D) in the blood serum was measured. In order to increase the effectiveness and safety of therapy, vitamin D saturation was carried out (50,000 IU per week for 4 weeks) followed by a transition to maintenance intake (800-2000 IU/day) depending on the degree of vitamin D deficiency. The daily calcium intake was at least 1000-1200 mg [13].
Inclusion criteria: signed informed consent; duration of postmenopause (after natural or surgical menopause) ≥1 year; diagnosis of AP, according to WHO criteria: BMD ( T
-criterion) of lumbar vertebrae (LI—LIV) and/or PBC or SBC –2.5
SD
and below;
the presence of low-traumatic fractures of the vertebrae, the spinal vertebrae or the radius with a T
-criterion of –1.5
SD
or lower and a high 10-year risk of major fractures according to FRAX.
Exclusion criteria: other metabolic skeletal diseases; hypocalcemia; malignant neoplasms diagnosed within the last 5 years before the start of therapy; taking other drugs for the treatment of AP after inclusion in the study, except for calcium and vitamin D; taking replacement therapy with female sex hormones; inability to perform densitometry of at least two lumbar vertebrae.
Among the patients there were no persons systematically taking glucocorticosteroids. The following concomitant diseases were identified: type 2 diabetes mellitus - in 8, diseases of the gastrointestinal tract - in 20, hypothyroidism, which requires taking levothyroxine less than 100 mcg / day - in 8, hypertension - in 28, various disorders heart rhythm - in 8, coronary heart disease - in 16, kidney disease with a decrease in creatinine clearance to 27 ml/min - in 3, breast cancer and mastectomy more than 5 years before inclusion in the study - in 6; 3 patients were treated with aromatase inhibitors. Diseases such as diabetes mellitus, hypothyroidism with long-term use of replacement therapy, and a history of therapy for breast cancer could determine the mixed nature of AP.
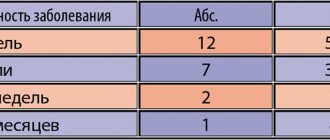
The maximum observation period was 4 years: 48 people received treatment for 12 months, 29 for 24 months, 11 for 36 months, 10 for 48 months.
Adverse events were assessed after the first administration of the drug, then after 6, 12, 24, 36 and 48 months of treatment based on questionnaires given to patients. In addition, the convenience of the scheme and form of drug administration was assessed using a 4-point system: very convenient, fairly convenient, satisfactory, unsatisfactory.
The patients were divided into 2 groups: 1st - 26 people who had previously received treatment with anti-osteoporotic drugs (15 aminoBP, 6 strontium ranelate, 10 active metabolites of vitamin D), and were transferred to denosumab therapy after consultation at the National Medical Research Center for PM due to the ineffectiveness of the drugs or poor tolerability no earlier than 3 months after the end of previous therapy; 2nd - 72 patients who had not received anti-osteoporotic therapy before denosumab was prescribed.
All patients underwent the following studies:
— examination and anthropometric study;
— dual-energy X-ray bone densitometry of the lumbar spine (LI-LIV) in the posteroanterior projection and POBC using Hologic Delpfi W (USA) and Lunar Expert (USA) devices. Dynamic measurements were carried out once a year on the same device. BMD indicators are unified and adjusted to the indicators used in the Hologic database using correction factors;
- laboratory tests: level of total calcium, creatinine, total alkaline phosphatase (TALP), C-terminal telopeptide of type I collagen (CTx, β-CrossCaps) in blood serum;
— survey about the presence of adverse events.
The 10-year probability of major osteoporotic fractures was assessed using the Russian FRAX model and bone resorption marker CTx once in 72 patients of group 2.
Statistical data processing was carried out using Microsoft Excel applications and the statistical data analysis package SPSS 20.0. Conventional methods of parametric and nonparametric analysis were used. Quantitative variables were described by the number of parameters, the arithmetic mean ( M
), standard deviation from the arithmetic mean (
σ
).
Qualitative variables were described in absolute and relative values (in percentages). Differences were considered statistically significant at p
<0.05. When comparing qualitative indicators, statistical analysis methods were used: Pearson's χ2 test, paired and unpaired Student's t-test. For parameters whose distribution differed from normal, nonparametric tests were used: when comparing two groups, paired Spearman correlation analysis was used to determine the two-sided significance of the indicators.
Results and discussion
During treatment with denosumab, a significant increase in BMD was observed in all measured skeletal areas (Fig. 1).
Rice.
1. Dynamics of BMD during treatment with denosumab. Here and in Fig. 2 * — p≤0.001. Thus, the increase in BMD in the lumbar spine after 12 months was 4.2%, after 24 months - 7.5%, after 36 months - 8.8%. In the ShBK there was an increase in BMD by 3.1, 3.9 and 5.3%, and in the entire PBC - by 2.8, 4.1 and 5%, in the forearm (1/3 of the radius) - by 0.9 , 1.4 and 2.6% respectively. The data obtained are consistent with the results of an axial phase III RCT assessing the effectiveness and safety of denosumab FREEDOM therapy. However, it should be noted that this study included women with T
-criterion of –2.5
SD
or less, but not less than –4
SD
, while in our study there were no restrictions and patients with a lower
T
-criterion were included.
Thus, in the first part of the FREEDOM study, which lasted for 3 years, BMD in the spine increased by 8.8%, in the BCD by 5.2%, and in the POB by 6.4% [14, 15]. The increase in radial bone BMD over 3 years of denosumab treatment was 3.5% ( p
≤0.0001) [7]. In addition, forearm BMD was measured in an extension study that included 115 patients in the FREEDOM placebo group who received calcium and vitamin D alone and subsequently switched to denosumab, which they received for 5 years in the FREEDOM extension study. Despite the decrease in BMD during the placebo period, at the end of the study there was an increase in BMD by 1.5%, which was important confirmation of the cessation of cortical bone loss [16]. Currently, denosumab is the only drug that increases BMD in the area of 1/3 of the forearm, indicating a clinically significant effect of the drug on cortical bone.
For a number of chronic non-infectious diseases and risk factors for their development, tactics are used to achieve target values of the studied indicators. For this purpose, biomarkers of the pathological process and their levels that must be achieved to prevent the development of complications have been identified. Thus, for a cerebral stroke, such a marker is the level of blood pressure, and its target level is 140/90 mmHg. [17]. Clinical guidelines for the treatment of AP currently do not identify special markers or define their target values. This is due to the fact that treatment with the most common antiresorptive drugs, BP, did not cause a constant and significant increase in bone mass, especially in the POBC, and the markers of bone turnover were characterized by very high variability. Currently, in the course of 5-, 6- and 10-year studies of FD, it has been shown that BMD increased maximally in the 3-4th year of treatment, and then remained at the same level or tended to decrease. This is probably due to the slowdown in bone mineralization during long-term use of BP, necessitating a temporary break in treatment [18, 19]. However, a meta-analysis of RCTs on the effectiveness and safety of various drugs for the treatment of AP has proven a statistically significant linear relationship between the increase in BMD in the vertebrae and femur and a decrease in the relative risk of fractures at a low level of injury [20]. The emergence of new antiresorptive (denosumab) drugs for the treatment of AP, which caused a continuous and significant increase in bone mass over 10 years, made it possible to consider BMD as a marker for achieving target values, i.e., transition from the “zone” of AP to the “zone” of osteopenia or overcoming the acceptable level of risk of fractures, which is T
-criterion –2.5
SD
.
Among 98 patients, according to the results of spinal densitometry, BMD according to T
-criterion below –2.5
SD
were detected in 79, the median
T
-criterion was –2.8
SD
.
After 12 months of therapy, this indicator increased in 23 (29%) women, and the median T
-score was –2.4
SD
, which corresponds to osteopenia.
In 56 patients, the T
-criterion for the spine area was low before the start of therapy, the median
T
-criterion was –3.4
SD
, and after 12 months of treatment it increased to a value of –2.9
SD
, but did not enter the “zone” of osteopenia. After 24 months, 25 people showed a transition from the “zone” of AP to the “zone” of osteopenia.
When analyzing the dynamics of BMD of the SBK, out of 47 people with identified AP in this skeletal area, 12 moved into the “zone” of osteopenia after 12 months of treatment. In the remaining 35 patients with the lowest BMD before treatment, median T
-criterion was –3.0
SD
, and after 12 months of therapy –2.8
SD
, which was also regarded as positive dynamics.
The study included 11 patients who at the first visit, according to densitometry, had osteopenia, but had a history of low-energy fractures, as well as a high risk of major fractures according to FRAX. Among them, 5 people had previously received anti-osteoporotic therapy and were switched to denosumab treatment. In 6 patients who had not previously received treatment, median T
-criteria before the start of the study was –1.5
SD
, –1.4
SD
, and after a year of therapy this indicator at both points was –1.2
SD
.
Achievement of target BMD was assessed over an 8-year period of treatment with denosumab in the FREEDOM study and concluded that many women with AP achieved non-osteoporotic T
-criteria (from 11 to 82%). Based on the results obtained, the authors called for the use of tactics to achieve target values in the treatment of AP [21].
An assessment of the dynamics of BMD after 12 months of therapy in 26 women who had previously taken anti-osteoporotic therapy showed a similar increase in bone mass as in the group of untreated patients, i.e., an additional positive effect was obtained when switching to denosumab (Table 2).
Table 2. Dynamics of BMD in 72 patients who did not receive and 26 who received anti-osteoporotic therapy before the start of the study. The data obtained confirm the results of studies that showed a more significant increase in BMD when patients were transferred from tablet BP or anabolic therapy with teriparatide to denosumab [22, 23].
A significant decrease in serum CTx concentration was noted 6 months after the start of denosumab therapy by 54% ( p
<0.001) and after 12 months - by 72% (
p
<0.001). Subsequently, when monitoring the CTx concentration once a year for 48 months, this level was maintained. These data are consistent with the results of the FREEDOM studies, in which the reduction in CTx concentrations reached 86 and 72% (after 1 and 36 months, respectively) and DECIDE (74% after 1 year of treatment) [8, 11] (Fig. 2).
Rice.
2. Dynamics of CTx levels during treatment with denosumab. In addition, a decrease in the level of total calcium in the blood was recorded after 6 months by 3.6% and after 12 months by 7.6% ( p
≤0.001). It should be noted that when assessing calcium metabolism before the start of therapy, 12 people showed slight and clinically insignificant hypercalcemia, which was not detected after 12 months of treatment. Subsequently, throughout the entire period of treatment, total calcium levels remained within normal limits. The hypocalcemic effect of denosumab in this case may indicate the manifestation of its pronounced antiresorptive effect. The decrease in the level of TAP in the blood did not reach statistical significance throughout the treatment. This is apparently due to the fact that ALP includes several isoenzymes, in addition to bone, reflecting the rate of bone remodeling. The average creatinine level did not change throughout treatment. In patients with reduced glomerular filtration of the kidneys, there was no increase in creatinine concentration in the blood. Currently, Prolia is the only drug for the treatment of AP approved for use in patients even with severe renal impairment. Due to its unique targeted mechanism of action, Prolia is not excreted in the urine and does not necessitate dose adjustment in chronic kidney disease. Special studies have shown that the degree of renal failure does not affect the pharmacokinetics and pharmacodynamics of the drug, and this provides an advantage to prescribing Prolia in this population [24].
Among the 98 patients who received the first injection of Prolia, no independent refusal to continue treatment was noted. The different number of patients after 24 months or more is associated with the period of analysis of the material, and not with the cessation of therapy, therefore in this article we do not draw conclusions about patients’ compliance with the prescribed treatment regimen.
The adverse events encountered were assessed as mild to moderate in severity. They are mainly associated with the musculoskeletal system: arthralgia was noted in 3 patients, the appearance or intensification of back pain - in 16, pain in the bones of the extremities - in 7. It should be noted that similar pain sensations in these patients were periodically observed before the start of therapy and Upon detailed questioning, women could not with complete confidence associate these manifestations with taking denosumab. In 2 patients, dermatitis was observed at a distance from the injection site 1 and 3 months after the first injection of denosumab, which resolved spontaneously. Both patients did not have a history of allergies and the cause of dermatitis could not be identified. All noted adverse events did not require discontinuation of the drug. During the observation period, 3 patients had fractures: one had a fracture of the radius in a typical place 2 months after the first injection, the second had a fracture of the ankle 3.5 months after the first injection, the third had deformities of 2 vertebrae 46 months after the start. treatment with denosumab. All patients were diagnosed with severe AP with a history of fractures, and new fractures were associated with low bone strength, and not with insufficient effect of the drug.
According to the survey, 86 patients found the drug administration regimen very convenient, 8 – quite convenient, 6 – satisfactory.
Benefits of denosumab for osteoporosis
ABOUT. ERSHOVA
, Doctor of Medical Sciences, Professor, Yaroslavl State Medical Academy,
A.V.
NAZAROVA , Candidate of Medical Sciences,
GUZ YaO KB SMP im.
N.V. Solovyova (Review of literature data)
Today, in the arsenal of a practicing doctor there is a sufficient number of effective drugs used for pathogenetic therapy of osteoporosis. According to the latest recommendations of the Russian Osteoporosis Association, the first-choice drugs for the treatment of osteoporosis, along with nitrogen-containing bisphosphonates and strontium ranelate, also include denosumab, the clinical effectiveness of which in reducing the risk of non-vertebral and vertebral fractures has been proven in long-term multicenter clinical trials.
The following drugs are registered in the Russian Federation for the treatment of osteoporosis (Table 1) [1]:
1st line drugs – alendronate, risedronate, ibandronate, zoledronic acid, strontium ranelate, denosumab; The 2nd line drug, salmon calcitonin, is currently prohibited for use in AP.
All first-line drugs act primarily by suppressing pathologically active resorption and are antiresorptive drugs, while strontium ranelate is a bidirectional drug that simultaneously suppresses increased resorption and activates bone formation.
Undoubtedly, all drugs have their advantages and disadvantages. Thus, bisphosphonates irreversibly suppress resorption, therefore, when prescribing them for a long period, it is always necessary to remember the possibility of the formation of so-called “frozen bone” [2] with a certain probability of atypical fractures (1 case per 1000 patients per year), which limits the time period of their use [3, 4, 5].
Denosumab is a fully human monoclonal antibody against RANK ligand. Denosumab is the first antiresorptive drug whose action is based on the regulation of the RANK-L-RANK-OPG bone remodeling system. Due to its unique pharmacokinetics, denosumab has certain advantages over other drugs used in the treatment of osteoporosis.
It has been approved for use in postmenopausal osteoporosis since June 2010. In the process of developing denosumab, a new opportunity has emerged to clarify the mechanisms of bone tissue remodeling in the interaction between competitive molecules RANK ligand (RANK-L), osteoprotegerin (OPG) and osteoclast receptors produced by osteoblasts. RANK) [6].
It was found that the main mechanism of bone loss and the development of fractures is an increase in osteoclastogenesis and bone resorption, because under conditions of estrogen deficiency, the balance in the RANK-L-RANK-OPG system is disturbed, and the amount of RANK-L exceeds the amount of osteoprotegerin. When the concentration of RANK-L in the bone microenvironment significantly exceeds the concentration of OPG, then more RANK ligand can bind to its receptor on the osteoclast, RANK. This RANK-L–RANK interaction results in a marked increase in osteoclast differentiation and activation, and thus increases bone resorption. If the concentration of OPG produced by osteoblasts exceeds the concentration of RANK-L, then less RANK ligand binds to the osteoclast receptor (RANK), as a result of which osteoclast differentiation and activation do not occur, and the process of bone resorption slows down. Therefore, the balance between RANK-L and OPG produced by osteoblasts is the determining internal factor of the bone microenvironment that regulates resorption [7].
Denosumab, a fully human monoclonal antibody to RANK-L, was the first product developed to reduce bone resorption by blocking the anchoring of RANK-L to RANK. Its mechanism of action is shown in Figure 1. A four-year phase II study [8] showed that the effect of denosumab was completely reversible based on time course analysis of DXA and bone markers (CTX). However, the reasons for the return of CTX and bone mineral density (BMD) to baseline values after denosumab discontinuation are unknown, which may be due to a bone mechanostatic mechanism.
It is known that bisphosphonates must be taken up by osteoclasts and are mainly located on the bone surface. Unlike bisphosphonates, denosumab does not bind to bone tissue. It circulates in the intercellular fluid, binding RANKL, inhibiting the formation, maturation, functioning and survival of osteoclasts. This fact explains why patients with osteoporosis who are already being treated with bisphosphonates may benefit from switching to denosumab therapy. A comparative study showed that switching to denosumab resulted in a greater increase in BMD and a greater reduction in bone resorption than with continued alendronate therapy [9, 17].
Similar results (a significantly greater increase in BMD during denosumab therapy) were demonstrated by comparative studies with ibadronate and risedronate among women in whom bisphosphonate therapy was not sufficiently effective [18, 19]. The FREEDOM study showed that denosumab compared with placebo reduced the risk of vertebral, non-vertebral and hip fractures by -68%, -20% and -40%, respectively [20].
Moreover, in patients over 75 years of age, the reduction in the risk of hip fractures reached 62% [21]. According to a review by Sutton EE and Riche DM [11], in a number of clinical trials, the effectiveness of denosumab in increasing bone mineral density is comparable to the effectiveness of alendronate, but is associated with a lower risk of osteonecrosis of the jaw and atypical fractures, but with a greater risk of infections and neoplasms.
However, another systematic review of four heterogeneous randomized controlled trials combining data from 1942 women found low-quality evidence for the hypothesis that denosumab reduces the risk of fractures more than alendronate, and the incidence of neoplasms and infections was similar in the denosumab and alendronate groups [12 ].
Denosumab may be recommended for use in patients after taking bisphosphonates if they are intolerant or ineffective, as well as for the period of the so-called. "medicinal holidays"
It should be noted that denosumab is an IgG 2 fully monoclonal antibody, so neutralizing antibodies are not formed to it. In addition, denosumab does not bind to TNF ligand - an inducer of apoptosis (TRAIL - a survival factor for tumor cells), and has no significant effect on the number of lymphocytes (CD3), T cells (CD 4, CD 8, CD 54) , or B-cells (CD 20) [13].
Most drugs have limitations for use in patients with low creatinine clearance values. For bisphosphonates, according to the instructions for use, with a creatinine clearance <35 ml/min, the risk of accumulation increases, and therefore there are restrictions on use, and the use of strontium ranelate with a creatinine clearance <30 ml/min is contraindicated. Denosumab, on the contrary, can be used even in patients with severe chronic renal failure. Meanwhile, according to the Public Health and Nutrition Examination Survey (NHANES) III, 85% of women with osteoporosis have mild or moderate renal dysfunction [14].
In order to determine the safety and effectiveness of the use of denosumab in patients with osteoporosis and impaired renal function, Jamal SA et al. [15] reanalyzed data in postmenopausal women with varying levels of renal impairment (FREEDOM RCT). The analysis included 7808 women aged 60 to 90 years with T-score BMD values between -2.5 SD and -4.0 SD at the lumbar spine or total hip. Exclusion criteria included hyper- or hypoparathyroidism, current hypocalcemia (albumin-corrected serum calcium concentration less than 2.13 mmol/L) or vitamin D deficiency (25-hydroxyvitamin D level less than 30 nmol/L). At the same time, 3902 women received denosumab and 3906 received placebo for 36 months. Serum creatinine and albumin-corrected calcium were measured every 6 months.
Based on the classification of the National Society of Chronic Kidney Diseases (K/DOQI Guidelines 2002), stages of renal dysfunction were assessed: stage 1 (normal renal function or renal damage with normal or increased glomerular filtration) - eGFR 90 ml/minute or more; stage 2 (renal damage with moderate decrease in glomerular filtration) - eGFR 60 - 89 ml/minute, stage 3 (moderate decrease in glomerular filtration) - eGFR 30 - 59 ml/minute, stage 4 (severe decrease in glomerular filtration) - eGFR 15 - 29 ml/minute. When calculated using the Cockcroft-Gault formula, 73 women had stage 4 chronic renal failure, 2817 had stage 3, 4069 had stage 2, and the remaining 842 women had stage 1 renal impairment. When calculated using the MDRD formula, 17 women had stage 4, 1078 had stage 3, 5413 had stage 2, and another 1298 women had stage 1.
When calculating the risk of vertebral and non-vertebral fractures depending on the stage of chronic kidney disease (CKD), no statistically significant relationships were identified; the reduction in the risk of fracture did not depend on the level of kidney function. The incidence of vertebral fractures was lower in the denosumab group compared with placebo for all stages of CKD, but this reduction was not statistically significant in the stage 4 CKD group. Also, the incidence of nonvertebral fractures was lower in the denosumab group compared with placebo, but this was not statistically significant for CKD stages 3 and 4. Due to the small number of proximal femoral fractures (43 in the placebo group and 26 in the denosumab group), differences by CKD stage were not calculated. The increase in BMD was also independent of kidney function, and there were no statistically significant differences depending on the stage of CKD.
The investigators found no differences in the incidence of adverse events, serious adverse events, serious adverse events related to infection, or cardiovascular events between the denosumab and placebo groups, stratified by CKD stage of CKD. In addition, there were no changes in glomerular filtration rate calculated using both formulas over 36 months of follow-up.
In addition, a 16-week open-label clinical trial was conducted at 12 US centers to evaluate the pharmacokinetics, pharmacodynamics and safety of denosumab in patients with varying degrees of decreased renal function [16]. The study included 55 patients: 12 with normal renal function, 13 with mild CKD, 13 with moderate CKD, 9 with severe CKD, 8 with severe renal failure (dialysis group). The proportion of women (51%) to men (49%) was similar, and the majority of patients (69%) were white. The average age of the participants was 64+15 years. Subjects received a single subcutaneous injection of 60 mg denosumab. Renal function in the groups was calculated using the Cockcroft-Gault equation and a formula developed by the US Food and Drug Administration (FDA), where the study was designed. Our results indicate that renal function did not significantly influence the pharmacokinetics or pharmacodynamics of denosumab, suggesting that denosumab dose adjustment based on glomerular filtration rate is not necessary. A rapid decrease in serum concentrations of the bone resorption marker 1C-telopeptide (CTX) was recorded throughout the study in all groups. The most common adverse events were: hypocalcemia (15%), pain in the extremities (15%) and nausea (11%). Most adverse events were rated by investigators as mild to moderate in severity. Administration of calcium and vitamin D supplements was not an original requirement of the study protocol but was implemented during the trial. Hypocalcemia was not reported in any patient while taking calcium and vitamin D. In seven patients, serum calcium was 7.5 – 8.0 mg/dl (1.9 – 2.0 mmol/l), in 5 patients (four of them with progressive kidney disease) calcium was below 7.5 mg/l dl (<1.9 mmol/l). Two patients (1 with symptomatic, 1 with asymptomatic hypocalcemia) were hospitalized for intravenous treatment with calcium gluconate.
Thus, denosumab has an important advantage over bisphosphonates - no effect on renal function, the drug is not excreted by the kidneys, and there is no need for dose adjustment in patients with reduced renal function. Supplemental calcium and vitamin D should be recommended in patients initiating denosumab therapy, especially in patients with reduced renal function.
Denosumab is a 1 ml subcutaneous solution containing 60 mg of active substance, administered once every 6 months. Indications for treatment with Denosumab are: postmenopausal osteoporosis; treatment of bone loss in women receiving aromatase inhibitor therapy for breast cancer and in men with prostate cancer receiving hormone deprivation therapy; treatment of senile osteoporosis in men. There are few contraindications: hypersensitivity to any of the components of the drug; hypocalcemia. During the course of treatment, it is recommended to additionally take calcium supplements and vitamin D.
Bibliography
1. Clinical recommendations for the prevention and management of patients with osteoporosis. Ed. Lesnyak O.M. Yaroslavl 2012– 24 p. 2. Aspenberg P., Schilcher J., Fahlgren A. Histology of an undisplaced femoral fatigue fracture in association with bisphosphonate treatment. Frozen bonewith remodeling at the crack. Acta Orthop. 2010;81(4):460–462. 3. Rizzoli R., Akesson K., Bouxsein M. et al. Subtrochanteric fractures after long-term treatment with bisphosphonates: a European Society on Clinical and Economic Aspects of Osteoporosis and Osteoarthritis, and International Osteoporosis Foundation Working Group Report. Osteoporos Int. 2011;22:373–390. 4. Shane E., Burr D., Ebeling PR et al. Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2010;25:2267–2294. 5. Schilcher J., Aspenberg P. Incidence of stress fractures of the femoral shaft in women treated with bisphosphonate. Acta Orthop 2009; 80(4):413–415. 6. Miller PD A review of the efficacy and safety of denosumab in postmenopausal women with osteoporosis. Ther Adv Musculoskel Dis 2011; 3(6): 271–282. 7. Boyle, W. J., Simonet, W. S. and Lacey, D. L. Osteoclast differentiation and activation. Nature 2003; 423:337–342. 8. Miller, PD, Bolognese, MA, Lewiecki, EM et al. Effect of denosumab on bone density and turnover in postmenopausal women with low bone mass after long-term continued, discontinued, and restarting of therapy: a randomized blinded phase 2 clinical trial. Bone 2008; 43(2): 222–229. 9. Muschitz C., Fahrleitner-Pammer A., Huber J. et al. Update on denosumab in postmenopausal osteoporosis—recent clinical data. Wien Med Wochenschr. 2012;162(17-18): 374–379. 10. Lippuner K. The future of osteoporosis treatment - a research update. Swiss Med Wkly 2012;142:w13624. 11. Sutton EE, Riche DM Denosumab, a RANK ligand inhibitor, for postmenopausal women with osteoporosis. Ann Pharmacother. 2012; 46(7-8):1000–1009. 12. Lin T., Wang C., Cai XZ et al. Comparison of clinical efficacy and safety between denosumab and alendronate in postmenopausal women with osteoporosis: a meta-analysis. Int J Clin Pract. 2012; 66(4):399–408. 13. Suda, T., Takahashi, N., Udagawa, N. U. et al. Modulation of osteoclast differentiation and function by the new members of the tumor necrosis factor receptor and ligand families. Endocr Rev. 1999; 20: 345–357. 14. Klawansky S., Komaroff E., Cavanaugh PFJ et al. Relationship between age, renal function and bone mineral density in the US population. Osteoporos Int. 2003;14:570–576. 15. Jamal SA, Ljunggren O, Stehman-Breen C et al. Effects of denosumab on fracture and bone mineral density by level of kidney function. J Bone Miner Res. 2011; 26(8):1829–1835. 16. Block GA, Bone HG, Fang L., Lee E., Padhi D. A single-dose study of denosumab in patients with various degrees of renal impairment. J Bone Miner Res. 2012;27(7):1471–1479. 17. Kendler DL, Roux C, Benhamou CL, et al. Effects of denosumab on bone mineral density and bone turnover in postmenopausal women transitioning from alendronate therapy. J Bone Miner Res. 2010;25:72-81. 18. C. Roux, A. Fahrleitner-Pammer et al. A Randomized Study to Evaluate the Safety and Efficacy of Denosumab and Rezidronate in Postmenopausal Women ASBMR; Minneapolis, MN; October 12–15, 2012. 19. Recknor et al. A Randomized Open-label Study to Evaluate the Safety and Efficacy of Denosumab and Ibandronate in Postmenopausal Women Suboptimally Treated With Daily or Weekly Bishosphonates (TTI study) ASBMR; Minneapolis, MN; October 12–15, 2012. 20. Cummings SR, San Martin J, McClung MR, et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361:756-765. 21. Boonen S, Adachi JD, Man Z et al. Treatment with denosumab reduces the incidence of new vertebral and hip fractures in postmenopausal women at high risk. J Clin Endocrin Metab. 2011;96:1727-1736.