Often, during routine examinations, people are diagnosed with high cholesterol. Not everyone thinks that if its amount exceeds the norm, then this is a direct threat to cardiovascular disorders. Doctors prescribe a special diet and a set of physical activities, but such measures do not always lead to good results. Then Atorvastatin comes to the rescue. Practice has proven that the medicine produces an excellent effect in combination with therapeutic nutrition.
What does Atorvastatin help with?
Atorvastatin is a medicine that lowers blood cholesterol levels. The drug is often used for both primary and secondary prevention of cardiovascular complications. Atoris is exactly such a drug. The main active ingredient is atorvastatin. Like other statins, it suppresses the effect of an enzyme involved in the initial stage of cholesterol formation. Bad cholesterol forms atherosclerotic plaques on the walls of blood vessels, obstructing blood flow. The medicine stops cholesterol synthesis. Plaques do not grow, and atherosclerosis does not progress.
Taking this drug reduces the risk of a heart attack and prevents the development of angina pectoris. It is prescribed to patients with acute coronary syndrome. In people with ischemic stroke, Atorvastatin slightly reduces the risk of recurrence of cardiovascular changes.
Atorvastatin tablets - reviews
Olga
I read the reviews and I’m just confused, I felt some kind of shock. I’ve been taking this drug for 1.5 months and NO PROBLEMS WITH HEALTH HAPPENED. It’s true that there was low blood pressure and a rapid heartbeat. There is NO nausea, etc. as they write here. It’s true You need to take a blood test and find out cholistyrene, it was 6.2.. And so there are no health problems
Olesya
Both drugs do an excellent job of lowering cholesterol. I myself took atorvastatin-sz, now I take rosuvastatin-sz. In general, I already have 10 years of experience taking statins; in 2009, I was diagnosed with hypercholesterolemia + complications due to diabetes. I took Atorvastatin-sz for 7 years, and did not observe any side effects from the second month of taking 5.8-6.2. Then, in 2016, I was recommended rosuvastatin-sz, a next-generation statin drug. I switched over and didn’t feel any subjective changes; my cholesterol remained normal. So I think it’s the taste and color... maybe it’s more modern, maybe some processes are not felt.
Jan
I highly recommend the drug. My father took it for 7 years and only remembered about cholesterol once every six months, when he did a lipid profile. Now he is taking rosuvastatin-sz, a type of newer drug, and so he is very pleased with this. Yes, it’s also very convenient to take because... 1 tablet per day
Julia
Good drug. I took it myself for a long time and it also suited my husband well. Cholesterol has been normal for many years, it’s just a pity that you need to take statins for the rest of your life. A month ago, the doctor suggested that my husband switch to rosuvastatin-sz, which is supposedly more modern. I switched and my cholesterol remained normal. Now I’m thinking, maybe I should change the drug or stay on atorvastatin?
Tatiana
Are 1st and 2nd generation statins still used? I only saw 3 generations of atorvastatin at the pharmacy - I took it once, it’s a good drug. I myself have been taking 4th generation rosuvastatin-sz quite successfully for a year now. Cholesterol 4.5, no side effects.
Dmitriy
The drug is definitely good, I took it for 5 years. Cholesterol did not leave the normal range. 2 years ago they replaced it (all as prescribed by a doctor) with rosuvastatin-sz, supposedly newer, the result is the same - I didn’t notice a difference, but it works.
Svetlana
My father takes Atorvastatin, he was prescribed to take it for life. Cholesterol dropped well, the problem was with triglycerides. Now they also prescribed Dibicor, and triglycerides also began to decrease and the liver stopped acting up, Dibicor turns out to protect it.
Vitaly
I took atorvastatin for high cholesterol, it helped, but unfortunately it made me feel sick. I asked the doctor to choose something else, he advised me to try rosuvastatin-sz - this is like a newer generation. I've been taking it for a month, everything is fine.
Varya
I have been taking atorvastatin-sz for the second year, my cholesterol has almost returned to normal, and I also think it has helped me lose a few kg. It helped me a lot; I wouldn’t have lasted long on a diet alone.
Violet
Atorvastatin sz was prescribed to me to lower cholesterol. We have a family problem and I knew about it. I take it regularly in courses, my cholesterol does not rise, and I have not found any harm to my health.
Marusya
Everyone writes that diet helps with cholesterol, but this is not at all true - it has long been proven that the main cholesterol is produced in the body itself. Atorvastatin is a good tablet and helps in treatment, but this is the previous generation of statins; many new ones have now been developed. I take rosuvastatin-sz - the effect is just as good, and there are fewer side effects.
Nika
I didn’t even know that I had problems with cholesterol until a doctor accidentally discovered it. I took a course of Atorvastatin SZ and followed a diet. Cholesterol has decreased, so I recommend it.
Nonna
When the analysis revealed elevated cholesterol, I was prescribed Atorvastatin sz. I suffered more from having to go on a diet. But I finally managed to lose weight. The product is good, I’m happy with it.
Marie
My mother takes Atorvastatin SZ. She has problems with cholesterol and stage 2 hypertension. Cholesterol really comes back to normal, we drink in courses. There are a lot of side effects in the instructions, but my mother hasn’t experienced any yet.
krasyuk
https://otzovik.com/review_5423711.html
Advantages:
- Helps lower blood cholesterol levels
Flaws:
- No cons
I began to feel dizzy, my blood pressure began to spike, and I felt lightheaded. and I went to the doctor, passed all the tests, had an ultrasound of the brain vessels, and the doctor prescribed me otorvostatin tablets. I started taking one 20-milligram tablet once a day at the same time, my condition began to improve, pressure surges decreased, etc. Every month I take tests to check the level of cholesterol in the blood and while I’m taking these tablets everything is normal, I recently replaced these pills with more effective ones, but it turned out that I was getting worse, so I went back to atorvostatin and I feel fine
General impression:
Very good pills that lower blood cholesterol levels
Natalia
https://zhivizdorovim.ru/lekarstva/serdechno-sosudistie/10818-atorvastatin.html#comment-7525
Atorvastatin helped a lot, cholesterol dropped from 6.4 to 3.8, I’ve been taking it for more than a year, slowly reducing the dosage from 40 mg to 10. I donate blood for testing every month. Now it is possible to take a maintenance dose, not daily, as before, but for example 2 times a week. Since after a stroke I have to take this drug for life!
Elena L.
https://protabletky.ru/atorvastatin/#otzivi
My mother drinks it, she was prescribed it for life. Her cholesterol was 9, which is a lot. When I started using Atorvastatin, after a month it turned out that my cholesterol had dropped to normal. But, since this is the case, they drink it constantly, since the body itself no longer regulates its level due to a metabolic failure. No side effects were observed.
Angela Ivanovna
https://instrukciya-otzyvy.ru/731-atorvastatin-po-primeneniyu-analogi-tabletki-teva-leksvm-statin-snizhenie-holesterina.html
Atorvastatin brought my cholesterol back to normal. Although I was previously elevated and a salt-free and fat-free diet did not help, but this medicine helped. I keep an eye on my muscles, as statins can destroy them and cause weakness. I advise all heart patients who take drugs from this group to do this.
(Anna22.04) Anna
https://www.imho24.ru/recommendation/55538/#review75624
Advantages:
- Price.
Flaws:
- Incompatible with many drugs.
This drug was prescribed to my grandmother, since, in addition to hypertension, she has high cholesterol. But, fortunately, this drug combines well with most antihypertensive drugs.
At the initial stage, the drug should be taken once a day, but it is very important to monitor the level of cholesterol in the blood, that is, get tested. After tests show that the drug acts without pathological manifestations, the dosage can be increased. It is necessary to strictly ensure that during the treatment period you do not use certain medications that can increase the active substance in the blood plasma, which can lead to unpleasant consequences. Such drugs include antibiotics, antifungals, and nicotinic acid.
By the end of the first month of taking it, my grandmother’s cholesterol dropped and became within the normal range.
Broodmother
https://otzyvy.pro/reviews/otzyvy-atorvastatin-135277.html
Advantages:
- helps
- it's inexpensive
Flaws:
- No
Unfortunately, the problem of high cholesterol affects many people today. If at a young age the body successfully copes with excess bad cholesterol, then after 35 years it is necessary to carefully monitor your health and all blood indicators. It is better to identify cholesterol immediately and not allow it to rise above the permissible norm. If you take tests every year, or more often, you can easily track the dynamics of cholesterol levels in your blood.
But if it so happens that cholesterol has gone beyond the normal range, then you should not put off treatment for a long time, you should take the appropriate medications. Atorvastatin is a well-known drug for lowering cholesterol levels.
The drug is inexpensive, costs around 160-180 rubles, is sold in every pharmacy, the price will most likely depend on the markup of a particular pharmacy chain.
Atorvastatin will be effective only in combination with an appropriate diet, this is written in the instructions, and the doctor repeated this when he prescribed Atorvastatin tablets.
It is very important to take tests before starting treatment to be sure how much your cholesterol levels are elevated; this is necessary in order to accurately calculate the dosage of the drug. In my case it was 1 tablet 3 times a day for a month. Dosages can be different, up to 8 tablets, but this is all prescribed and controlled by a specialist.
A month later, a blood test was scheduled to find out whether the drug worked or not. After this time, I donated blood again, as the results showed, there was an effect and there was a significant decrease in cholesterol, but its level was still outside the normal range, it was decided to take Atorvastatin for another 2 weeks with the same dosage and at the same time drink milk thistle meal for the liver. This dietary supplement also helps lower cholesterol.
After another 2 weeks, the tests came back to normal, I breathed a sigh of relief, but this is no reason to relax. Yes, the drug Atorvastatin was discontinued, but then only diet and constant monitoring of health.
Andrey Leonov
https://www.piluli.ru/product/Atorvastatin/review
The drug helped me personally, brought my cholesterol to normal, but you still have to follow a strict diet, otherwise there will be a chain reaction: cholesterol - Atorvastatin and vice versa, and then there are problems with the liver (read side effects). The drug is inexpensive, the effect is no worse than the imported one, but guys, you need to move away from chemistry and quit with butter, sausage and sweets and other joys. Eh..
Tatiana Prokofieva
https://www.medcentre.com.ua/atorvastatin.html?id=60723#otzyv
Diet for high cholesterol plays almost the most important role. My grandmother's total cholesterol was 10 mmol/l. The doctor advised to adhere to a certain diet: a minimum of animal fats (if meat, then lean chicken, turkey); more vegetables, fruits (preferably unsweetened fruits); maintain water and drinking regime. The medication she prescribed was Atorvastatin. My grandmother took the drug once a day. After six months, the following results were observed: weight decreased by 14 kg (proper nutrition played a role), cholesterol became normal. Now the threat of atherosclerosis has passed.
Side effects
The unpleasant effects that arise from taking statins are ambiguous. In a study of healthy people taking atorvastatin, no side effects occurred. They manifest themselves in citizens at risk. Negative phenomena may be associated with the development of the disease and with the simultaneous use of other medications. The most common manifestations are:
- nausea;
- bronchitis;
- arthritis;
- infection of the genitourinary system.
Rarely, taking statins can provoke:
- diabetes;
- muscle pain;
- liver damage.
From the nervous system you can observe:
- headache;
- increased fatigue;
- dizziness;
- redness of the eyes;
- noise in ears;
- amnesia and other undesirable effects.
And:
- increased blood pressure;
- arrhythmia;
- angina pectoris;
- rhinitis;
- sinusitis;
- diarrhea;
- constipation;
- nausea;
- vomiting;
- manifestation of infections.
The problems end after stopping the drug.
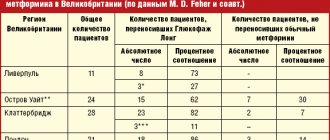
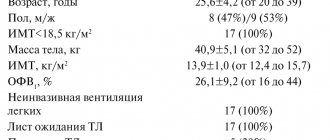
Why does atorvastatin have advantages on the “restricted” lists?
Comparative effectiveness of statins Today, no one doubts the direct correlation between the level of cholesterol (C) and low-density lipoprotein cholesterol (LDL-C) in the blood and cardiovascular mortality. Therefore, the main goal of lipid-lowering therapy is to reduce LDL cholesterol. Recent meta-analyses show that the most effective drugs for the treatment of severe lipid metabolism disorders are synthetic statins [7] (atorvastatin in a daily dose of 10 mg reduces LDL levels by an average of 39%, lovastatin and pravastatin in a dose of 40 mg - by 31%, simvastatin 40 mg – by 35–41%, fluvastatin 40–80 mg – by 25–35%, rosuvastatin 10 mg – 39–45%) [15]. Obviously, the use of 10 mg of atorvastatin is equivalent to 20 mg of simvastatin, 40 mg of lovastatin and pravastatin, 80 mg of fluvastatin. At these doses, comparable statins [10] reduce the concentration of LDL cholesterol by an average of 34%, and total cholesterol by 27%, while atorvastatin reduces them by 55% (and according to a number of studies, by 61%) and by 46 % respectively. A distinctive feature of atorvastatin is its ability to effectively reduce triglyceride levels by 23–45%, which is comparable to the effect of rosuvastatin. Not only rosuvastatin, but also atorvastatin reduces CRP levels and affects HDL levels. The results of the largest JUPITER study showed that rosuvastatin in the first 12 months. increased HDL content by only 4%. At the same time, atorvastatin has shown high efficiency in a wide range of dosages (from 5 to 80 mg per day), which is extremely important when conducting aggressive lipid-lowering therapy. Comparison of the results of large clinical trials (Fig. 1) allows us to conclude that atorvastatin can most often achieve target lipid levels. Evidence base for the use of statins. As Graham Jackson put it, the world has come close to the threshold of the “great statin war.” As criteria for the preference of a particular statin, as a rule, they appeal either to laboratory and biochemical effectiveness, or to the ability to reduce overall and cardiovascular mortality. Although when prescribing many statins, it is possible to achieve normalization of blood lipid parameters with the correct dosage, a large evidence base has been accumulated according to which atorvastatin is much more effective than simvastatin and rozyvastatin in reducing cardiovascular complications. Based on the results of large multicenter randomized studies (CARE and WOSCOPS - pravastatin, 4S - simvastatin), they state a reduction in the risk of coronary mortality by 20–42%, the incidence of myocardial infarction by 25–37%, and the incidence of stroke by 28–31% . However, it should be noted that the dosage regimen and initial cholesterol level in these studies were fundamentally different (in the CARE and WOSCOPS studies, pravastatin [18] was prescribed to patients with a total blood cholesterol level of 4.0–6.2 mmol/l at a dose of 40 mg per day, and in the 4S study [14], simvastatin was prescribed for hypercholesterolemia of 5.5–8.0 mmol/l and a daily dose of 20–40 mg). It seems that this approach of indirectly comparing the effectiveness of drugs does not comply with the principles of evidence-based medicine. And besides this, data on the effect of statins on other clinically important surrogate points and other pathologies concomitant with hyperlipidemia are ignored. If we compare the results of the GREACE [1] and 4S studies, it turns out that atorvastatin reduces overall mortality, mortality from coronary artery disease, and the number of heart attacks and strokes almost 2 times more significantly than simvastatin (Fig. 2). Moreover, a clear advantage of atorvastatin over simvastatin in terms of the rate of reduction in the risk of developing cardiovascular complications is revealed: atorvastatin reduces the risk of their development after just three months of taking the drug, and simvastatin only after 1.5 years. Without going into a discussion about the advisability of using higher doses of statins from the very beginning of treatment with them, it is important to keep in mind the results of the GREACE study [1], in which the initial dose of atorvastatin was 20 mg per day (average dose 24 mg per day). 95% of patients on this dose of atorvastatin achieved target LDL cholesterol levels, while only 3% of patients in the usual care group did so. Of particular interest to clinicians is the ability of statins not only to prevent or slow the development, but also to reduce the size of existing atherosclerotic plaque. Atorvastatin has been shown to slow down and regress atherosclerotic plaque in at least two large studies using intravascular ultrasound, REVERSAL [11] and ESTABLISH [13]. It is very interesting to compare the results of the ESTABLISH (atorvastatin) and ASTEROID (rosuvastatin) studies [12]. 6-month therapy with atorvastatin at a dose of 20 mg per day led to a decrease in atheroma size by 13.1%, while 24-month therapy with rosuvastatin at a dose of 40 mg per day was accompanied by a decrease in atheroma size by 6.8%. Noteworthy is the fact that the average therapeutic dose of atorvastatin in terms of severity and rate of reduction of atheroma looked at least no worse than a high dose of rosuvastatin. If we analyze the number of studies on statins (www.medlinks.ru/aticle.php?sid=10855) with “hard” endpoints (overall mortality, cardiovascular mortality, myocardial infarction, stroke) and the number of patients included in them, then atorvastatin leads in the number of works, along with simvastatin and pravastatin, despite the fact that it appeared on the market much later than them. So, we can conclude that atorvastatin allows not only to achieve a pronounced and persistent reduction in atherogenic lipid fractions and improve the lipid profile in general, significantly slowing the progression of atherosclerosis, but also, most importantly, it has been proven to reduce the risk of developing cardiovascular disease. At the same time, it is atorvastatin that most closely corresponds to the principle of treating atherosclerosis: we treat not high cholesterol, but a patient with a high risk of developing cardiovascular complications. Clinically significant interactions between statins and other drugs Since the advent of statins, the issue of possible positive synergistic effects on endpoints when combined with antihypertensive drugs has been actively discussed. Disappointment after the publication of the results of the ALLHAT-LLA substudy (pravastatin was added to antihypertensive therapy) was dispelled only after the completion of the ASCOT-LLA trial [16,17]. In the ASCOT-LLA study, during therapy with amlodipine + perindopril, a reduction in the incidence of the primary endpoint by 36%, as well as secondary endpoints (fatal and non-fatal stroke - by 27%, all cardiovascular events and procedures - by 21%, of all coronary events – by 29%). At the same time, in the group of patients who received the treatment regimen amlodipine + perindopril + atorvastatin, the relative risk of reducing the development of non-fatal myocardial infarction and fatal ischemic heart disease was 48%, and fatal and non-fatal stroke was 44%. Apparently, it is the combination of amlodipine and atorvastatin that is most optimal for realizing a synergistic interaction [2]. One study showed that it is the combination of amlodipine and atorvastatin that best ensures not only the achievement of target lipid levels, but also blood pressure [3,8]. There are several explanations for this fact. First of all, amlodipine and atorvastatin are the undoubted leaders in their drug classes. In addition, the combination of amlodipine + atorvastatin has a beneficial effect on interleukin (IL-6), tumor necrosis factor-alpha (TNF-alpha) and insulin sensitivity (IR). It was shown that y 50 patients with normal cholesterol levels (total cholesterol <5.2 mmol/l], body mass index >/=30 kg/m2 and increased DBP >90 and <105 mmHg and SBP >140 and <180 mmHg) in a cross-over design after 12 weeks there are significant differences between the two compared treatment regimens (amlodipine 10 mg and amlodipine 10 mg + atorvastatin 20 mg). During monotherapy with amlodipine, there was a decrease in SBP and DBP (by 17.1 and 14.3 mm Hg, respectively, p = 0.008), TNF-alpha (from 3.66 ± 1.6 to 3.09 ± 1, 1 pkg/ml, p=0.045) and IR (from 4.58±0.7 to 3.88±0.6, p=0.007). When using the combination of amlodipine + atorvastatin, a decrease in SBP and DBP was detected (by 22.5 and 17.7 mm Hg, respectively; p = 0.04 when compared with amlodipine monotherapy), TNF-alpha (by 2.59 ± 0 .9 pkg/ml; p=0.038 when compared with amlodipine, IR (by 2.86±0.4; p=0.007 when compared with amlodipine), IL-6 (from 7.93±1.9 to 5.59±1 .2 pkg/ml; p=0.007 compared with amlodipine) and total cholesterol (from 4.3±0.5 to 3.6±0.4 mmol/l; p=0.008 compared with amlodipine).It is obvious that the combination of amlodipine + atorvastatin not only has a more pronounced antihypertensive effect, but also significantly reduces the manifestations of insulin resistance and inflammation [5].Many authors believe that there is a possible interaction between amlodipine and statins at the molecular level, which leads to the stabilization of the atherosclerotic plaque and causes a more pronounced reducing the risk of coronary events [3,8] Pharmacoeconomics of statins The effectiveness/cost ratio of lipid-lowering therapy is of great practical interest. The large-scale CURVES study showed that the high effectiveness of atorvastatin in influencing LDL cholesterol levels determines its better pharmacoeconomic indicators compared to other statins. It is fundamentally important to emphasize that all of the above, from lowering lipid levels to stabilization and regression of atherosclerotic plaque, concerned exclusively the original atorvastatin - Liprimar (), and it is impossible to automatically extrapolate these data to the numerous generics of atorvastatin existing in Russia. Of course, there are high-quality drugs among them, but they must prove their clinical and therapeutic effectiveness (at least in terms of their effect on the main, surrogate points) in direct comparative studies. As confirmation of the above about the advantages of Liprimar, we can cite the results of an analysis of 80 thousand patients from the Real World database on reducing the risk of developing cardiovascular complications in comparison with simvastatin. A retrospective Buena Vista analysis of a large US database found that patients treated with Liprimar (atorvastatin calcium) had a 14% lower risk of cardiovascular events, including myocardial infarction and stroke, compared with patients treated with simvastatin even after dose adjustment. The analysis included 61,324 patients taking Liprimar and 19,585 taking simvastatin who had not received a statin in the 6 months before the start of the study. The primary endpoint was defined as hospitalization due to myocardial infarction, stroke, mini-stroke (transient ischemic attack), chest pain (angina) or coronary heart disease, vascular disease or other conditions requiring cardiac surgery, and was assessed after taking a statin for at least 3 months of therapy. In an analysis that took into account the reduction in the risk of cardiovascular events, starting from the first day of treatment with Liprimar, compared with the simvastatin group, there was a 26% lower risk reduction. Differences in the clinical effect in patients taking Liprimar or simvastatin were evident within the first 3 months and increased accordingly during the further observation period. Interestingly, an earlier similar study in the Netherlands involving 3,500 patients and based on data from general practitioners showed that patients receiving Liprimar had a 30% greater reduction in the risk of cardiovascular events than those receiving other statins ( simvastatin, pravastatin, fluvastatin and cerivastatin). Thus, today atorvastatin (Liprimar) is the only statin that combines a reduction in LDL levels from 39 to 60% and an evidence base in the form of more than 400 ongoing and completed clinical studies involving more than 80 thousand patients (of which more than 50 thousand patients took participation in more than 10 endpoint studies focused on reducing the risk of cardiovascular events).
References 1. Athyros V, Papageorgiou A, Mercouris B. Treatment with atorvastatin to the National Cholesterol Educational Program goal versus “usual” care in secondary coronary heart disease prevention. The GREACE study. Current Medical Research and Opinion; 2002; 18, 4: 220–228 2. Blank RA single–pill combination of amlodipine besylate and atorvastatin calcium. Drugs Today (Barc). 2006; 42(3):157–75. 3. Dorval JF, Anderson T, Buithieu J, Chan S. et al. Reaching recommended lipid and blood pressure targets with amlodipine/atorvastatin combination in patients with coronary heart disease. Am J Cardiol. 2005; 95(2):249–53. 4. European guidelines on cardiovascular disease prevention in clinical practice. Third Joint Task Force of European and other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of eight societies and invited experts). Eur Heart J 2003; 24: 1601–10 5. Fogari R, Preti P, Zoppi A, Lazzari P, Corradi L, Fogari E, Ciccarelli L, Derosa G. Effects of amlodipine–atorvastatin combination on inflammation markers and insulin sensitivity in normocholesterolemic obese hypertensive patients. Eur. J. Clin. Pharmacol. 2006; 6: 178–81. 6. Garcia MJ, Reinoso RF, Sanchez Navarro A, Prous JR. Clinical pharmacokinetics of statins. Methods Find Exp Clin Pharmacol. 2003;25(6):457–81 7. Istvan E. Statin inhibition of HMG–CoA reductase: a 3-dimensional view Atherosclerosis 2003;Suppl. 4:3–8 8. Jukema JW, van der Hoorn JW. Amlodipine and atorvastatin in atherosclerosis: a review of the potential of combination therapy. Expert Opinion on Pharmacotherapy. 2004; 5:459–468. 9. Lennernas H. Clinical pharmacokinetics of atorvastatin. Clin Pharmacokinet. 2003;42(13):1141–60. 10. Moghadasian MH, Mancini & Frohlich. Pharmacotherapy of hypercholesterolaemia: statins in clinical practice. // Exp.Opin.Pharmakother.(2000) 1(4), p.683–695 11. Nissen S, Tuzcu M, Schoenhagen P. Effect of Intensive Compared With Moderate Lipid–Lowering Therapy on Progression of Coronary Atherosclerosis. JAMA. 2004;291:1071–1080 12. Nissen S, Nicholls S, Sipahi I. Effect of very high-intensity statin therapy on regression of coronary atherosclerosis. The ASTERIOD trial. JAMA. 2006;295:1556–1565 13. Okazaki S, Yokoyama T, Miyauchi K Early Statin Treatment in Patients With Acute Coronary Syndrome. Demonstration of the Beneficial Effect on Atherosclerotic Lesions by Serial Volumetric Intravascular Ultrasound Analysis During Half a Year After Coronary Event: The ESTABLISH Study. Circulation. 2004;110:1061–1068. 14. Randomized trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S) Lancet. 1994;344(8934):1383–9 15. Schaefer EJ, McNamara JR, Tayler T et al., Comparisons of effects of statins (atorvastatin, fluvastatin, lovastatin, pravastatin, and simvastatin) on fasting and postprandial lipoproteins in patients with coronary disease heart disease versus control subjects. Am J Cardiol. 2004;93(1):31–9 16. Sever P on behalf of the ASCOT investigators. ASCOT–LLA revisited: Interaction of antihypertensive and lipid–lowering therapy. American Heart Association Scientific Sessions; November 14, 2005; Dallas, TX. 17. Sever PS, Dahlof B, Poulter NP, Wedel H. Anglo–Scandinavian Cardiac Outcomes Trial: Lipid Lowering Arm (ASCOT LLA) revisited: interaction of antihypertensive and lipid lowering therapy. Circulation 2005; 112 (17 Suppl.): II–134. Abstract 730. 18. West of Scotland Coronary Prevention Study: implications for clinical practice. The WOSCOPS Study Group. Eur Heart J 1996 Feb;17(2):163–4
Contraindications
Atorvastatin should not be taken:
- people who have severe liver diseases - chronic hepatitis, liver failure, cirrhosis;
- women of reproductive age;
- children under 18 years of age.
The therapeutic effect after taking the medicine is not immediately noticeable. This drug prevents the formation of atherosclerotic formations, but does not resolve them. The body itself copes with the gradual removal of plaques. How quickly the process moves depends on the individual. Some will need more time, some less.
Do not stop taking the medication without consulting a doctor.
Who is Atorvastatin useful for?
Statins are indicated for people at risk. Healthy patients are not recommended to take them as prophylaxis. The issue has not been fully studied, and there are no effective clinical trial data. The drug is prescribed when diet, exercise, or other weight loss measures have not helped.
The main diseases for which atorvastatin is prescribed are:
- combined hyperlipidemia;
- primary or hereditary hypercholesterolemia;
- familial endogenous hypertriglyceridemia.
But the main purpose is cardiac ischemia (CHD).
In pregnant women, Atorvastatin crosses the placenta and reaches high concentrations in the fetal liver. It was not tested in humans, but in rats it was established that the survival rate of offspring was reduced. Among the surviving rodents, a decrease in body weight and developmental delays were noted.
If Atorvastatin is used simultaneously with antibiotics and clarithromycin, myopathy may progress, and the concentration of the substance in the blood plasma can increase by 40%.
Antacids - medicines used to treat the stomach - reduce the concentration of atorvastatin in the blood by 35%.
Atorvastatin
During treatment with HMG-CoA reductase inhibitors, with simultaneous use of cyclosporine, fibrates, nicotinic acid in lipid-lowering doses (more than 1 g / day) or inhibitors of the CYP3A4 isoenzyme / transport protein (for example, erythromycin, clarithromycin, antifungal agents - azole derivatives), the risk increases myopathy (see section “Special instructions”).
CYP3A4 isoenzyme inhibitors
Since atorvastatin is metabolized by the CYP3A4 isoenzyme, co-administration of atorvastatin with inhibitors of the CYP3A4 isoenzyme may lead to increased plasma concentrations of atorvastatin. The degree of interaction and potentiation effect is determined by the variability of the effect on the CYP3A4 isoenzyme.
It was found that potent inhibitors of the CYP3A4 isoenzyme lead to a significant increase in the concentration of atorvastatin in the blood plasma. The simultaneous use of strong inhibitors of the CYP3A4 isoenzyme (for example, cyclosporine, telithromycin, clarithromycin, delavirdine, stiripentol, ketoconazole, voriconazole, itraconazole, posaconazole and HIV protease inhibitors, including ritonavir, lopinavir, atazanavir, indinavir, darunavir, etc.) should be avoided whenever possible. If concomitant use of these drugs is necessary, initiating therapy at the lowest dose should be considered and the possibility of reducing the maximum dose of atorvastatin should be evaluated.
Moderate inhibitors of the CYP3A4 isoenzyme (for example, erythromycin, diltiazem, verapamil and fluconazole) may lead to increased plasma concentrations of atorvastatin. With the simultaneous use of HMG-CoA reductase inhibitors (statins) and erythromycin, an increased risk of developing myopathy was noted. Interaction studies between amiodarone or verapamil and atorvastatin have not been conducted. Both amiodarone and verapamil are known to inhibit the activity of the CYP3A4 isoenzyme, and simultaneous use of these drugs with atorvastatin may lead to increased exposure to atorvastatin. In this regard, it is recommended to reduce the maximum dose of atorvastatin and carry out appropriate monitoring of the patient's condition when used simultaneously with moderate inhibitors of the CYP3A4 isoenzyme. Monitoring should be carried out after the start of therapy and against the background of changing the dose of the inhibitor.
Gemfibrozil/fibrates
With the use of fibrates in monotherapy, adverse reactions, including rhabdomyolysis, affecting the musculoskeletal system were periodically noted. The risk of such reactions increases with simultaneous use of fibrates and atorvastatin. If the simultaneous use of these drugs cannot be avoided, the minimum effective dose of atorvastatin should be used, and the patient's condition should be regularly monitored.
Ezetimibe
The use of ezetimibe is associated with the development of adverse reactions, including rhabdomyolysis, from the musculoskeletal system. The risk of such reactions increases with simultaneous use of ezetimibe and atorvastatin. For such patients, careful monitoring is recommended.
Erythromycin/clarithromycin
With the simultaneous use of atorvastatin and erythromycin (500 mg 4 times a day) or clarithromycin (500 mg 2 times a day), inhibitors of the CYP3A4 isoenzyme, an increase in the concentration of atorvastatin in the blood plasma was observed (see sections "Special instructions" and "Pharmacokinetics" ).
Protease inhibitors
The simultaneous use of atorvastatin with protease inhibitors, known as inhibitors of the CYP3A4 isoenzyme, is accompanied by an increase in the concentration of atorvastatin in the blood plasma.
Diltiazem
The combined use of atorvastatin at a dose of 40 mg with diltiazem at a dose of 240 mg leads to an increase in the concentration of atorvastatin in the blood plasma (see section “Pharmacokinetics”).
Cimetidine
No clinically significant interaction of atorvastatin with cimetidine was detected (see section “Pharmacokinetics”).
Itraconazole
The simultaneous use of atorvastatin in doses from 20 mg to 40 mg and itraconazole in a dose of 200 mg led to an increase in the AUC value of atorvastatin (see section "Pharmacokinetics").
Grapefruit juice
Since grapefruit juice contains one or 1 more components; which inhibit the CYP3A4 isoenzyme, its excessive consumption (more than 1.2 liters per day) may cause an increase in the concentration of atorvastatin in the blood plasma (see section “Pharmacokinetics”).
Transport protein inhibitors
Atorvastatin is a substrate of liver enzyme transporters (see section "Pharmacokinetics").
Co-administration of atorvastatin 10 mg and cyclosporine 5.2 mg/kg/day resulted in increased atorvastatin exposure (AUC ratio: 8.7) (see Pharmacokinetics section).
Cyclosporine is an inhibitor of organic anion transport polypeptide 1B1 (OATP1B1), OATP1B3, multidrug resistance-associated protein 1 (MDR1) and breast cancer resistance protein, as well as CYP3A4, and therefore increases the exposure of atorvastatin. The daily dose of atorvastatin should not exceed 10 mg (see section “Dosage and Administration”).
Glecaprevir and pibrentasvir are inhibitors of OATP1B1, OATP1B3, MDR1 and breast cancer resistance protein, and therefore increase the exposure of atorvastatin. The daily dose of atorvastatin should not exceed 10 mg (see section “Dosage and Administration”).
Co-administration of atorvastatin 20 mg and letermovir 480 mg daily resulted in increased atorvastatin exposure (AUC ratio: 3.29) (see Pharmacokinetics section).
Letermovir is an inhibitor of the transporters P-gp, BCRP, MRP2, OAT2 and the hepatic transporter OATP1B1/1B3, thus increasing the level of exposure to atorvastatin. The daily dose of atorvastatin should not exceed 20 mg (see section “Dosage and Administration”).
The magnitude of indirect drug interactions between CYP3A and OATP1B1/1B3 on co-administration of drugs may differ when letermovir is co-administered with cyclosporine. It is not recommended to use atorvastatin in patients receiving letermovir therapy in combination with cyclosporine.
Elbasvir and grazoprevir are inhibitors of OATP1B1, OATP1B3, MDR1 and breast cancer resistance protein and therefore increase the exposure of atorvastatin. Should be used with caution and at the lowest dose required (see section "Dosage and Administration").
Inducers of the CYP3A4 isoenzyme
The combined use of atorvastatin with inducers of the CYP3A4 isoenzyme (for example, efavirenz, rifampicin or St. John's wort preparations) may lead to a decrease in the concentration of atorvastatin in the blood plasma. Due to the dual mechanism of interaction with rifampicin (an inducer of the CYP3A4 isoenzyme and an inhibitor of the hepatocyte transport protein OATP1B1), simultaneous use of atorvastatin and rifampicin is recommended, since delayed administration of atorvastatin after taking rifampicin leads to a significant decrease in the concentration of atorvastatin in the blood plasma (see section “Pharmacokinetics”).
However, the effect of rifampicin on the concentration of atorvastatin in hepatocytes is unknown and if concomitant use cannot be avoided, the effectiveness of this combination should be carefully monitored during therapy.
Antacids
Simultaneous oral administration of a suspension containing magnesium hydroxide and aluminum hydroxide reduced the concentration of atorvastatin in the blood plasma (change in AUC: 0.66), but the degree of reduction in the concentration of LDL-C did not change.
Phenazone
Atorvastatin does not affect the pharmacokinetics of phenazone, so interaction with other drugs metabolized by the same cytochrome isoenzymes is not expected.
Colestipol
With simultaneous use of colestipol, the concentration of atorvastatin in the blood plasma decreased (change in AUC: 0.74); however, the lipid-lowering effect of the combination of atorvastatin and colestipol was superior to that of each drug alone.
Digoxin
With repeated administration of digoxin and atorvastatin at a dose of 10 mg, the equilibrium concentrations of digoxin in the blood plasma did not change. However, when digoxin was used in combination with atorvastatin at a dose of 80 mg/day, digoxin concentrations increased (AUC change: 1.15). Patients receiving digoxin in combination with atorvastatin require appropriate monitoring.
Azithromycin
With simultaneous use of atorvastatin at a dose of 10 mg 1 time per day and azithromycin at a dose of 500 mg 1 time per day, the concentration of atorvastatin in the blood plasma did not change.
Oral contraceptives
With simultaneous use of atorvastatin and oral contraceptives containing norethisterone and ethinyl estradiol, increased concentrations of norethisterone (AUC change 1.28) and ethinyl estradiol (AUC change 1.19) were observed. This effect should be taken into account when choosing an oral contraceptive for a woman taking atorvastatin.
Terfenadine
With simultaneous use of atorvastatin and terfenadine, no clinically significant changes in the pharmacokinetics of terfenadine were detected.
Warfarin
In a clinical study in patients regularly receiving warfarin therapy, concomitant use of atorvastatin at a dose of 80 mg per day resulted in a slight increase in prothrombin time of approximately 1.7 s during the first 4 days of therapy. The indicator returned to normal within 15 days of atorvastatin therapy. Although significant interactions affecting anticoagulant function have been observed only in rare cases, the prothrombin time should be determined before initiating atorvastatin therapy in patients receiving coumarin anticoagulant therapy and frequently enough during therapy to prevent a significant change in the prothrombin time. Once stable prothrombin time values are observed, its monitoring can be carried out in the same way as recommended for patients receiving coumarin anticoagulants. When changing the dose of atorvastatin or discontinuing therapy, prothrombin time should be monitored according to the same principles as described above. Atorvastatin therapy was not associated with bleeding or changes in prothrombin time in patients not receiving anticoagulant treatment.
Colchicine
Although studies have not been conducted on the simultaneous use of colchicine and atorvastatin, there are reports of the development of myopathy when using this combination. Caution should be exercised when atorvastatin and colchicine are used concomitantly.
Amlodipine
In a drug interaction study in healthy subjects, coadministration of atorvastatin 80 mg and amlodipine 10 mg resulted in a clinically insignificant increase in atorvastatin concentrations (AUC change: 1.18).
Fusidic acid
During post-marketing studies, cases of rhabdomyolysis have been reported in patients taking concomitant statins, including atorvastatin and fusidic acid. The mechanism of this interaction is unknown. In patients for whom the use of fusidic acid is considered necessary, statin treatment should be discontinued for the entire period of use of fusidic acid. Statin therapy can be resumed 7 days after the last dose of fusidic acid.
In exceptional cases where long-term systemic therapy with fusidic acid is necessary, for example for the treatment of severe infections, the need for concomitant use of atorvastatin and fusidic acid should be considered on a case-by-case basis and under close medical supervision. The patient should seek immediate medical attention if symptoms of muscle weakness, tenderness, or pain occur.
Other concomitant therapy
In clinical studies, atorvastatin was used in combination with antihypertensive agents and estrogens as part of hormone replacement therapy. There were no signs of clinically significant adverse interactions; No interaction studies with specific drugs have been conducted.
In addition, an increase in the concentration of atorvastatin was observed when used simultaneously with HIV protease inhibitors (combinations of lopinavir and ritonavir, saquinavir and ritonavir, darunavir and ritonavir, fosamprenavir, fosamprenavir with ritonavir and nelfinavir), hepatitis C protease inhibitors (boceprevir, elbasvir/grazoprevir, simeprevir) , clarithromycin and itraconazole. Caution should be exercised when using these drugs together and the lowest effective dose of atorvastatin should be used.
Analogs
All generics of atorvastatin are available in the form of film-coated tablets.
The price of the original drug varies from 120 to 580 rubles.
- Atorvastatin Teva has moved a little higher in terms of monitoring, and the cost is lower than the original drug.
- The drug Atoris deserves more attention, but its price is from 300 to 1000 rubles.
- Tarvocard, according to experts, is more effective than Atoris, but its cost reaches 1,400 rubles.
- The undisputed leader among doctors is Liprimar. A reflection of his primacy can be seen in the price tag: from 600 to 2500 rubles.
Expert advice
Atorvastatin is produced by many pharmaceutical companies, but not all of them show good results. Cheap analogues often have an annoying property - frequent side effects. It is difficult to understand the production technology of companies that are not drug developers. They sometimes carefully hide secrets.
Doctors recommend choosing only those medications that have positive results of therapeutic equivalence analysis. Atoris, for example, a studied analogue, is popular with doctors. “Faceless” tablets priced from 100 to 200 rubles should raise concerns: side effects can strike with enormous force, and the desired therapeutic result will never be achieved. When choosing a drug, it is better to trust your doctor. Most of them still want to cure the patient, and only they can know which medicine is suitable in a particular case.
Atorvastatin-Teva tab 20mg N30 (Teva)
Before starting Atorvastatin therapy, the patient must be prescribed a standard cholesterol-lowering diet, which he must follow during the entire treatment period. The use of HMG-CoA reductase inhibitors to reduce blood lipid levels can lead to changes in biochemical parameters reflecting liver function. Liver function should be monitored before starting therapy, 6 weeks, 12 weeks after starting Atorvastatin and after each dose increase, and periodically, for example, every 6 months. An increase in the activity of liver enzymes in the blood serum may be observed during therapy with Atorvastatin. Patients who experience elevated enzyme levels should be monitored until enzyme levels return to normal. If alanine aminotransferase (ALT) or aspartic aminotransferase (AST) values are more than 3 times the upper acceptable limit, it is recommended to reduce the dose of Atorvastatin or discontinue treatment. Atorvastatin should be used with caution in patients who abuse alcohol and/or have liver disease . Active liver disease or persistent increases in aminotransferase activity of unknown origin are contraindications to the use of Atorvastatin. Treatment with Atorvastatin may cause myopathy. The diagnosis of myopathy (muscle pain and weakness in combination with an increase in creatine phosphokinase (CPK) activity more than 10 times the upper limit of normal) should be considered in patients with widespread myalgia, muscle soreness or weakness, and/or a marked increase in CPK activity. Patients should be warned that they should immediately tell their doctor if they experience unexplained muscle pain or weakness if they are accompanied by malaise or fever. Atorvastatin therapy should be discontinued in the event of a marked increase in CPK activity or in the presence of confirmed or suspected myopathy. The risk of myopathy during treatment with other drugs in this class was increased with concomitant use of cyclosporine, fibrates, erythromycin, niacin, or azole antifungals. Many of these drugs inhibit cytochrome P450 3A4-mediated metabolism and/or drug transport. Atorvastatin is biotransformed by CYP 3A4. When prescribing Atorvastatin in combination with fibrates, erythromycin, immunosuppressive agents, azole antifungals or nicotinic acid in lipid-lowering doses, the expected benefits and risks of treatment should be carefully weighed and patients should be regularly monitored to detect muscle pain or weakness, especially during the first months of treatment and during periods of increasing the dose of any drug. In such situations, periodic determination of CPK activity can be recommended, although such monitoring does not prevent the development of severe myopathy. When using Atorvastatin, as well as other drugs of this class, cases of rhabdomyolysis with acute renal failure caused by myoglobinuria have been described. Atorvastatin therapy should be temporarily discontinued or completely discontinued if signs of possible myopathy occur or if there is a risk factor for the development of renal failure due to rhabdomyolysis (for example, severe acute infection, hypotension, major surgery, trauma, severe metabolic, endocrine and electrolyte disturbances, and uncontrolled seizures). Before initiating therapy with Atorvastatin, attempts should be made to control hypercholesterolemia through adequate dietary therapy, increased physical activity, weight loss in obese patients, and treatment of other conditions. Patients should be warned to seek immediate medical attention if unexplained muscle pain or weakness occurs. , especially if they are accompanied by malaise or fever. Effects on the ability to drive a car and use machines. Adverse effects of Atorvastatin on the ability to drive a car and use machines have not been reported.