What can spirometry determine?
Spirometry (spiro - breathing, metria - measurement) is a method that allows you to evaluate the volume of inhaled and exhaled air, as well as the speed of its passage through the respiratory tract in a calm and forced state.
With the help of this safe and painless study, possible pathologies of respiratory function and oxygen metabolism, the presence of bronchial asthma and chronic obstructive pulmonary disease are determined.
The study is carried out using a spirometer - a device for measuring the volume of air leaving the lungs during the greatest exhalation after the greatest inhalation.
What is the purpose of the study?
Any pathology in the tissues and organs of the respiratory system leads to breathing problems. Changes in the functional state of the bronchi and lungs are reflected in the spirogram. The disease can affect the chest, which acts as a kind of pump, the lung tissue, which is responsible for gas exchange and oxygenation of the blood, or the respiratory tract, through which air must pass freely.
In case of pathology, spirometry will show not only the fact of respiratory dysfunction, but will also help the doctor understand which part of the lungs is affected, how quickly the disease progresses, and what therapeutic measures will help best.
During the examination, several indicators are measured at once. Each of them depends on gender, age, height, body weight, heredity, physical activity and chronic diseases. Therefore, interpretation of the results should be made by a physician familiar with the patient's medical history. Typically, the patient is referred for this test by a pulmonologist, allergist or general practitioner.
Indications for spirometry
Pulmonary function testing is prescribed to:
- identify pathologies of the respiratory and cardiovascular systems;
- assess the impact of pathology of any organ or system on the function of external respiration;
- clarify or confirm the diagnosis of respiratory diseases;
- evaluate the effectiveness of the drugs used;
- identify the source of gas exchange disturbance;
- assess the level of bronchial obstruction;
- assess ability to work when working in hazardous working conditions;
- choose anesthesia method.
Spirometry reveals disturbances in the functioning of the respiratory system at the initial stages, which increases the chances of recovery.
Smokers, asthmatics and athletes are prescribed this examination on a regular basis to monitor their health and monitor the progress of treatment.
Spirography and spirometry
Table of contents
- Spirography (spirometry): what is this procedure?
- Indications for research
- Execution principle
- Advantages of spirography (spirometry) at MEDSI in Moscow
Diagnosis of external respiratory function
is a mandatory component of many general clinical examinations, which are carried out annually to monitor health status. For patients at risk, the intervals between diagnostic measures may be reduced.
In order to study external respiration, spirography is carried out today (including with a sample)
. The procedure is quick, safe and painless. The patient does not experience significant discomfort. In some cases, minor side effects occur: increased heart rate and tremors of the limbs, which go away on their own within a few minutes or hours.
Spirography (spirometry): what is this procedure?
The procedure allows us to identify pathologies not only of the respiratory system, but also of the cardiovascular system. Diagnosis is carried out using a special medical device. The device consists of a sensor that responds to air flow and computer systems. They determine all the characteristics important for the survey and convert them into digital format.
The spirometer records the volume of air from the lungs at maximum exhalation after maximum inhalation. When interpreting the examination results, the patient’s age is taken into account. This is due to the fact that the norm varies among people of different age categories.
Both spirography and breathing spirometry aim to measure lung function. During the first procedure, additional graphical recording of indicators is made. This is the slight difference between the methods.
Important! The quality and accuracy of diagnostic results depend on a number of factors, including:
- serviceability of equipment
- equipment settings feature
- the patient clearly follows the specialist’s instructions
- research methodology used
That is why it is very important to undergo the procedure in a modern clinic with experienced specialists. They will carry out all the manipulations and perform informative diagnostics.
It is very important to strictly follow all doctor’s recommendations! Only in this case will the assessment of lung function be carried out accurately and make it possible to make a diagnosis as soon as possible.
The tests examine the following indicators:
- Breathing rate.
This indicator represents the number of breathing movements that are performed within a minute. Normally, a person takes 16–17 breaths - Tidal volume.
This parameter determines the volume of air entering the lungs per breath - Minute breathing volume.
This indicator determines the volume of air entering the lungs within a minute. It varies from 4 to 10 liters
Also assessed:
- forced vital capacity
- forced expiratory volume per second
- maximum efficient ventilation
- air speed, etc.
Important! All indicators are assessed only as a whole. Only with a number of deviations from the norm can we speak of the presence of severe pathology. Any assessment is carried out exclusively by a doctor. We strongly do not recommend trying to diagnose yourself! You do not have all the knowledge and skills necessary for this.
Carrying out spirography today is relevant not only for therapists and pulmonologists, but also for cardiologists, allergists-immunologists and other doctors. Additionally, other examinations are performed. As a rule, only after a comprehensive diagnosis is it possible to identify even hidden pathologies of various organs and systems.
Indications for research
You should undergo spirometry to:
- diagnosis of bronchopulmonary diseases
- respiratory failure assessments
- work ability examination
- recording initial signs of respiratory disorders among workers in hazardous industries
- monitoring the treatment already carried out and the effectiveness of prescribed therapy or rehabilitation measures
- choosing the type of artificial ventilation or anesthesia before surgery
The main indications for the examination are:
- dyspnea
- feeling of incomplete inspiration and lack of oxygen
- prolonged (more than a month) cough
- acute allergic reactions
- many years of smoking experience
- neuromuscular diseases
- suspicion of bronchitis, tracheitis, bronchial asthma, etc.
- diseases of the cardiovascular system that occur with insufficient blood circulation
- chest injuries or abnormalities of its development
In addition, spirometry should be done as part of a comprehensive examination of athletes and other categories of patients.
Execution principle
Testing can be carried out in two positions: standing or sitting. During the procedure, a clamp is placed on the patient's nose, which prevents the passage of air. A special device is attached to a mouthpiece placed in the oral cavity. Spirography is provided at maximum exhalation, at rest, with increased air circulation through the lungs.
In some cases, a study is carried out with the additional use of special drugs. It is relevant when specific diseases are suspected.
- Spirometry with bronchodilator.
This diagnosis allows us to identify bronchospasm. The procedure is also relevant when treatment has already been prescribed and monitoring its effectiveness. - Testing with methacholine.
This test spirometry is aimed at identifying asthma. The examination also reveals a tendency to bronchospasm.
Diagnosis is carried out in stages. At first, the patient is in a relaxed state, and at the request of the doctor, he performs some breathing manipulations.
- Tidal volume testing.
The patient performs normal relaxed inhalations and exhalations - Determination of expiratory reserve volume.
During natural inhalation, intense exhalation is performed - Measurement of inspiratory reserve volume.
Intensive inhalation follows natural exhalation - Determination of vital capacity of the lungs.
During this test, the patient exhales deeply and inhales calmly.
At the end of the main part of the examination, the mouthpiece is removed and the patient rests. In order to eliminate errors, diagnostics can be repeated several times.
Can also be performed:
- Measurement of forced vital capacity.
In this test, the patient inhales air, holds it in, and then, with some effort, quickly exhales. Important! The duration of exhalation should be at least 6 seconds - Determination of maximum ventilation.
To perform this test, you need to breathe as often and deeply as possible for a minute. Important! At this stage of diagnosis, some side effects may occur: darkening of the eyes and dizziness - Bronchodilation tests.
For such tests, medications that have a bronchodilator effect are additionally used. They are administered by inhalation. Testing takes approximately 15–30 minutes
Advantages of spirography (spirometry) at MEDSI in Moscow
- Modern equipment.
To perform the examination, expert-class installations are used. To increase the information content and accuracy of research, equipment is regularly maintained - Experienced doctors.
Specialists in the field of functional diagnostics have all the skills and knowledge that allow them to carry out accurate examinations. Our doctors regularly improve their qualifications and master the necessary spirometry techniques - No queues and the ability to make an appointment at a convenient time.
You can get tested during our clinic opening hours. It is enough to sign up for diagnostics in advance. We do not delay in deciphering the results - Possibility of complex diagnostics.
If necessary, the patient is additionally referred for laboratory tests and other examinations. This allows you to make an accurate diagnosis in a short time - Possibility of examining adults and children.
We accept patients of all ages and provide comfortable conditions for everyone - Possibility of treatment immediately after receiving the results.
We are ready to provide comprehensive therapy for pathologies. If necessary, hospitalization in a hospital is provided
If you are planning to do spirometry (spirography) in Moscow in our clinic, or want to find out the price of the examination, call +7 (495) 7-800-500. A specialist will answer all questions and make an appointment at a convenient time.
How to prepare for spirometry?
Half an hour before the start of the procedure, you need to calm down, relax and restore your breathing.
For maximum reliability of the results, the doctor may stop taking bronchodilators a day or several hours before the diagnosis.
It is also recommended to wear comfortable clothing that does not restrict movement.
The medical professional will check the patient’s height, weight and age, what medications have been taken and in what dosages recently. All this information can influence the results, and they will be taken into account when deciphering the spirogram.
Spirometry: where to do the test?
Today there are a huge number of clinics where spirometry is performed. The price in Moscow may be slightly higher than in other regions of Russia and, on average, is about 1,300 rubles.
The highest quality diagnostics of respiratory system diseases is carried out at the Yusupov Hospital. The clinic is equipped with all the necessary modern diagnostic equipment, thanks to which examination errors are minimized. Interpretation of spirometry results with maximum accuracy and in the shortest possible time is performed by highly qualified diagnosticians. Thanks to reliable diagnostics, experienced pulmonologists at the Yusupov Hospital Therapy Clinic - doctors of the highest category - select effective individual therapeutic tactics for each patient.
How is the spirometry procedure performed?
The patient sits in front of the spirometer. A disposable mouthpiece is attached to the device. The subject tightly clasps his lips and lightly presses the mouthpiece with his teeth. To fully record the volume and speed of inhaled and exhaled air, the medical worker applies a nose clip to the patient through an individual napkin.
The patient is explained what breathing maneuver needs to be done: maximum calm inhalation and exhalation; calm inhale and exhale as forcefully as possible, etc. Each test is performed three times. Rest between breathing maneuvers is 1 – 2 minutes.
Don't worry if you feel dizzy - this is a normal reaction that goes away after a few minutes.
Rules for preparing for spirography
To get the most accurate result, the patient needs to take into account some preparatory manipulations. The day before spirography, you should avoid active physical activity. It is better to avoid intense cardio or strength training in the gym, replacing them with yoga, stretching, or limit yourself to quick morning exercises. Smoking is prohibited 4 hours before the procedure, and eating food is prohibited 2 hours before the procedure. You should also avoid taking medications that can cause dilation of the bronchi. If necessary, the doctor himself will suggest an individually selected medicine. If it is impossible to cancel therapy, the results are assessed taking into account the characteristics of the patient and the functions of his respiratory system. The day before the test, it is recommended to replace tea/coffee/other caffeine-containing drinks with regular filtered water or freshly squeezed juice. Immediately before starting the study, it is better to loosen your tie, belt, and remove jewelry that interferes with free inhalation and exhalation. Typically, the patient is given from 15 to 30 minutes to adapt, relax, listen to instructions and tune in to spirography.
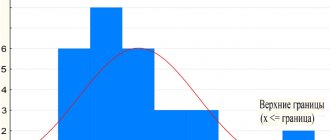
Evaluating the results and comparing them with the norm
Most modern spirographs are equipped with special programs that facilitate the interpretation of research results. During the procedure, you can immediately set the age, gender, height and weight of the subject, and the data obtained will be immediately compared with accepted standards.
The assessment of the received materials is carried out by comparison with a table of actual indicators with standards, that is, values “accepted as the ideal standard”
In healthy people, FEV1, VC, MVL, FVC and IT are often over 80% (but do not exceed 120%) of generally accepted figures. Values below 70% of the norm are considered a manifestation of pathology. Indicators in the range of 80–70%, as a rule, are interpreted individually for each person who underwent the procedure. For older patients, such values do not indicate the presence of pathology, while for children, young people and middle-aged people they may be symptoms of the initial stages of obstruction.
In such situations, additional diagnostics using medication will be required. The conclusion about the deterioration of the ventilation conductivity of the lungs is initially based on the indicators of FEV1 and MVL, but when determining the type of ventilation pathologies, the combination of the indicators FEV1, MVL and VC occupies a dominant place.
Research methodology
To take a spirogram, the patient must be seated as comfortably as possible. His clothing should not compress the chest and interfere with free breathing. The seat on which the subject sits and the oral tube are installed in accordance with his height, so that he does not have to bend over or stretch his neck upward. You also need to control the position of your torso when exhaling - do not let your body lean forward.
When performing spirography, it is necessary to sit the patient so that it is comfortable for him to perform breathing tests
The test analyzes oral airflow measurements and requires the patient to use a nose clip and hold the mouthpiece tightly to prevent air leakage. If the subject has dentures installed, they cannot be removed, as this will disrupt the quality fixation of the mouthpiece.
First, several primary tests are carried out - measuring tidal volume (TI), which is calculated based on the average of six or more respiratory cycles at rest. Then, in a calm state, the respiratory rate (RR) is determined. The product of these values will give the minute volume of breathing. A new type of spirograph, equipped with software, automatically provides all calculations.
The spirograph processes information immediately during the study and produces a tape with recorded results. At the signal from the diagnostician, the examinee inhales as completely as possible, and then exhales as sharply and as long as possible. The exhalation time should take at least 6 seconds and the patient should maintain maximum effort throughout the exhalation until completion.
Often, individuals undergoing testing are unable to inhale and exhale properly the first time, so the test is carried out using several attempts under the control of a recorded curve. Then the subject needs to breathe with maximum depth and frequency for 12 seconds. In certain cases, in some patients, such tests can cause dizziness, “floaters” before the eyes or darkening and even fainting, but the latter conditions are diagnosed quite rarely.
Spirometric monitoring for respiratory diseases
Multi-day and repeated spirometric measurements (eg, morning and evening values in children with asthma), the pattern of results can be important for identifying specific aspects of the child's disease.
Typical patterns are: the morning bear pattern in some asthmatics due to a drop in the early morning hours and a decrease in PEFR (peak expiratory flow) during the week, improving on weekends and holidays, as occurs in occupational asthma. Isolated reductions in PEFR due to specific allergens or triggers can help identify and quantify them. A downward trend in PEFR and an increase in its variability may indicate worsening asthma and can be used by the clinician or patient to change therapy. Monitoring of peak expiratory flow is especially useful for children with asthma, who cannot yet assess the severity of their condition, for subsequent assessment of response to treatment.
Spirometry with bronchodilator
One of the options for conducting FVD is a study with an inhalation test. This study is similar to regular spirometry, but the values are measured after inhalation of a special aerosol drug containing a bronchodilator. A bronchodilator is a drug that dilates the bronchi. The study will show whether there is hidden bronchospasm, and will also help you choose the appropriate bronchodilators for treatment.
As a rule, the study takes no more than 20 minutes. The doctor will tell you what and how to do during the procedure. Spirometry with a bronchodilator is also completely harmless and does not cause any discomfort.