The definition of endometriosis as a process in which benign growth of tissue occurs outside the uterine cavity, similar in morphological and functional properties to the endometrium, has remained unchanged over the last century. The treatment of endometriosis remains an unresolved scientific problem and is the subject of clinical research in many countries around the world [1, 2].
The most important clinical symptoms of endometriosis that determine indications for treatment are pelvic pain, disruption of normal menstrual blood loss, infertility, and dysfunction of the pelvic organs. The severity and set of manifestations of the disease vary individually. Symptoms characteristic of adenomyosis (endometriosis of the uterine body) - menometrorrhagia and perimenstrual bleeding - are caused by both cyclic transformations of the ectopic endometrium and a violation of the contractile function of the uterus. Pelvic pain, usually worsening the day before and during menstruation, is typical for both external endometriosis and adenomyosis. Another symptom characteristic of endometriosis (in the absence of other visible causes) is infertility, which accompanies this pathology in 46-50% of cases [3, 4]. Comparison of the effectiveness of diagnostic methods made it possible to determine that ultrasound is the optimal and generally available diagnostic method in the algorithm for examining patients with various forms of endometriosis [5, 6].
The current situation is indisputable: it is impossible to eliminate the anatomical substrate of endometriosis by any means other than surgery, after which it is advisable to carry out adjuvant hormonal therapy to prevent relapse of the disease [3, 7, 8]. However, despite the rapid development and widespread introduction of modern hormonal drugs into practice, it is not possible to achieve a complete cure for this disease, but it is possible to reduce the severity of such painful symptoms as bleeding, pain, dyspareunia, which undoubtedly improves the quality of life and reduces the risk of hysterectomy during reproductive age [7, 8].
Typically, endometriosis develops against the background of relative and absolute hyperestrogenism with progesterone deficiency. That is why the pathogenetic basis of hormonal therapy is a temporary inhibition of ovarian function, i.e., a decrease in the secretion of estradiol - the creation of pseudomenopause due to blockade of the pituitary-ovarian system with the initiation of hypoestrogenism, leading to regression of endometriosis foci [6, 9, 10]. For hormonal therapy of endometriosis, combined synthetic estrogen-gestagen drugs, progestins, antigestagens, antigonadotropins, antiestrogens, and androgens are most often used. Gonadotropin-releasing hormone (GnRh) agonists are currently the most effective drugs for the treatment of patients with endometriosis of late reproductive age in the postoperative period [7-11].
The purpose of this study is to study the effectiveness and safety of the drug "Buserelin-long FS" at a dose of 3.75 mg, a lyophilisate for the preparation of a suspension for intramuscular administration of prolonged action, produced by JSC "F-Sintez", Russia, in patients of late reproductive age with endometriosis of the uterus. This drug is a synthetic analogue of endogenous GnRH; it competitively binds to the receptors of the cells of the anterior pituitary gland, causing a short-term increase in the level of sex hormones in the blood plasma, which subsequently leads to a complete reversible blockade of the gonadotropic function of the pituitary gland, thus inhibiting the release of LH and FSH. As a result, there is a suppression of the synthesis of sex hormones in the gonads, which is manifested by a decrease in the concentration of estradiol in the blood plasma to postmenopausal values. After the first administration of buserelin, by day 21 in women, the concentration of estradiol decreases to a level corresponding to oophorectomy or postmenopause. The concentration of testosterone and estradiol remains reduced throughout the entire period of treatment, carried out every 28 days, which leads to growth inhibition and reversal of endometriosis foci. After cessation of treatment, physiological hormone secretion is restored.
The researchers were given the following tasks:
- assess the level of hormones LH, FSH, estradiol before treatment with Buserelin-long FS and during treatment;
— evaluate echographic data during transvaginal ultrasound examination of the uterus and appendages before treatment with Buserelin-long FS and during treatment;
— assess the condition and pathological changes of the endometrium before and after treatment with Buserelin-long FS using endometrial aspiration biopsy;
— to evaluate the safety of using the drug “Buserelin-long FS” at a dose of 3.75 mg, a prolonged-release lyophilisate produced in Russia.
Material and methods
The clinical study was conducted in 2012 at several medical institutions in Russia, including in the gynecological department of the State Budgetary Healthcare Institution of the Moscow Region “Moscow Regional Research Institute of Obstetrics and Gynecology”.
The clinical study protocol included 50 patients aged 35 to 45 years (mean age was 39.28±3.37 years) with a follicle-stimulating hormone level ≤15 mIU/ml in the blood serum in the early follicular phase with a diagnosis of uterine endometriosis I, II , III stage, confirmed by echography and hysteroscopy, with or without uterine fibroids (including 4 patients with submucous uterine fibroids measuring more than 3 cm in the period of preparation for resection of the myomatous node), who met all inclusion criteria and did not have exclusion criteria, who agreed to inclusion into the study and signed the “Patient Informed Consent”. A mandatory condition was the use of barrier methods of contraception throughout the study.
The clinical study included a screening period (patient selection) and a study period.
• The screening period (from the initial visit to the patient's first administration of study drug) ranged from 1 to 30 days.
• The study period (from the 1st day of drug administration, which corresponded to the 2-5th day of the menstrual cycle following the screening period, until the final visit) included 112-116 days.
Patients who were screened and met the inclusion and exclusion criteria were included in the study. Treatment with the drug "Buserelin-long FS" began on the 2-5th day of the menstrual cycle following the screening period, and continued for 112-116 days (a total of 4 intramuscular injections of the drug with an interval of 28 days).
Screening period (visit 0)
Informed consent to participate in the clinical study was obtained from all patients before the start of screening procedures. Each patient who agreed to participate in the study personally signed and dated two copies of the Patient Information Sheet containing the informed consent form. After signing, one copy of the Patient Information Sheet with the informed consent form was left at the study center, and one copy was given to the patient.
The eligibility assessment was a collection of assessments performed within 1 to 30 days before the first dose of the drug to determine the eligibility of a particular patient for inclusion in the study.
The researcher interviewed the patient, during which her medical history was collected and her eligibility for inclusion in the study was assessed.
Pre-follow-up examination for drug efficacy and safety (visit 5)
The pre-follow-up examination for efficacy and safety of the drug was performed 28–32 days after the last administration (visit 4).
The purpose of this examination is to ensure that patients are receiving a favorable treatment effect and to confirm that all parameters determined during the compliance assessment are maintained within clinically acceptable limits. For values outside this range and of clinical significance, observation should be carried out until their normalization was achieved or their changes were adequately explained.
During the screening period, vital signs, including electrocardiogram (ECG), were found to be within normal limits for all participants. Height ranged from 152 to 178 cm and averaged 164.82±5.94 cm, and body weight ranged from 48 to 109 kg and averaged 66.93±13.16 kg. Hemodynamic parameters were also assessed. The average systolic blood pressure (SBP) was 113.3±8.06 mmHg, and the indicator itself ranged from 90 to 125 mmHg. Diastolic blood pressure (DBP) ranged from 60 to 85 mm Hg. (average 70.34±7.56 mmHg). Heart rate (HR) varied from 54 to 82 beats/min (average 70.38±6.17 beats/min). Body temperature ranged from 36 to 36.8 °C (average 36.51 ± 0.18 °C).
Also, during the screening period, the study protocol provided for hysteroscopy with biopsy. For some patients, by the decision of the investigator and agreement with the sponsor, hysteroscopy with biopsy was not performed, since the diagnosis of uterine endometriosis was clearly made based on ultrasound results and the clinical picture and was not in doubt, which allowed the patients to avoid a painful invasive procedure.
All patients included in the study had a verified diagnosis: stage I, II, III uterine endometriosis.
The average FSH value ranged from 6.28±3.39 mIU/ml, and the indicator itself ranged from 1.9 to 15.44 mIU/ml. One patient, in agreement with the sponsor, was accepted into the study despite an FSH value of 15.44 mIU/ml, since a slight deviation in the initial FSH level (less than 0.5 mIU/L) did not affect the study results. Thus, 49 of 50 screened patients met the inclusion criterion of “FSH level ≤15 mIU/ml in serum in the early follicular phase.”
The average LH value was 6.18±6.55 mIU/ml, and the indicator itself ranged from 0.5 to 40 mIU/ml, estradiol - 461.6±352.9 pmol/l, and the indicator itself ranged from 69.75 up to 1755 pmol/l.
Ultrasound assessed the value of the median uterine echo (M-echo), which averaged 6.0±3.22 mm, the indicator itself varied from 1.1 to 13 mm. In 100% of patients, bacterioscopic parameters of the vaginal smear were within normal limits.
In most cases, endometriosis was combined with other gynecological pathology, which was noted in 41 (82%) participants, among them: with uterine fibroids - 39 (78%); with benign ovarian diseases - 2 (4%). Among all those examined, 5 (10%) suffered from infertility, 3 (60%) suffered from primary infertility, and 2 (40%) suffered from secondary infertility. 7 (14%) of 50 patients had a history of spontaneous miscarriages and non-developing pregnancies, and 2 (4%) had recurrent miscarriage.
Before the start of clinical studies, 35 patients underwent myomectomy. Indications for surgical treatment were: rapid tumor growth - in 32 (64%) patients; atypical location of myomatous nodes - in 25 (50%); large and gigantic size of the nodes in combination with a symptom of compression of adjacent organs and disruption of their function - in 6 (12%) and a pain symptom - in 29 (58%); with the symptom of bleeding leading to anemia - in 34 (68%) patients.
One patient withdrew her consent for personal reasons unrelated to the use of the drug and stopped participating in the study early. During the clinical trial, no serious adverse events associated with the use of the drug were recorded.
Results and discussion
List of efficiency parameters
The protocol provided for the following performance criteria:
1. Studies of hormone levels in the blood:
— decrease in LH level to 7.4±7.3 mIU/ml;
— decrease in FSH level to 7.0±5.6 mIU/ml;
- decrease in estradiol level <110 pmol/l.
2. Instrumental research:
- transvaginal ultrasound examination of the uterus and appendages - reducing the thickness of the median uterine echo to 4-6 mm. Changes in the pathological structures of the myometrium with varying degrees of adenomyosis during treatment;
- aspiration biopsy of the endometrium - changes in pathological structures in the endometrium or endometrial atrophy.
3. Assessment of health using the “Patient Questionnaire” - assessment of complaints, general condition, emotional state, physical condition, menopausal symptoms.
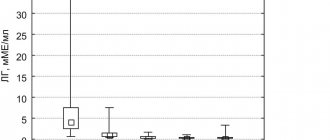
Dynamics of LH levels
. At the screening visit, as well as at visits 2–5, patients' blood was tested to determine LH levels (Fig. 1).
Rice.
1. Dynamics of LH levels during the use of the drug “Buserelin-long FS”. Achieving the target LH level <7.4±7.3 mIU/ml was achieved in 100% of patients by visit 2 after starting therapy with Buserelin-long FS.
By visit 5, there was a decrease in LH levels in all patients by an average of more than 6 times compared to the visit during the screening period.
Thus, 50 (100%) of 50 patients met the effectiveness criterion “Decrease in LH levels to 7.4±7.3 mIU/ml.”
Dynamics of FSH levels
. At the screening visit, as well as at visits 2–5, patients' blood was tested to determine FSH levels.
When analyzing the level of FSH during therapy with the drug "Buserelin-long FS" (Fig. 2), a statistically significant decrease in the level of this hormone was revealed at visits 2, 3, 4 and 5.
Rice. 2. Dynamics of FSH levels during the use of the drug “Buserelin-long FS”.
Thus, the patient population ( n
=50) generally satisfied the criterion “Decrease in FSH level to 7.0±5.6 mIU/ml”: the average FSH level in patients at visit 5 was 4.54±2.5 mIU/ml. A decrease in FSH levels by visit 5 was observed in 33 (66%) of 50 patients. Since, based on the literature, therapy with GnRH analogues does not always lead to a decrease in FSH levels in patients with endometriosis, other parameters of effectiveness should be taken into account when presenting a conclusion about the effectiveness of the drug.
Dynamics of estradiol levels
. At the screening visit, as well as at visits 2–5, patients' blood was tested to determine estradiol levels.
Already by visit 2, a statistically significant decrease in estradiol levels was registered, which persisted throughout the entire course of therapy (Fig. 3).
Rice. 3. Dynamics of estradiol levels during the use of the drug “Buserelin-long FS”.
Of the 50 patients, 32 (64%) achieved target estradiol levels of ≤110 pmol/L. In a study by U. Cirkel et al. [12] the level of estradiol in patients with endometriosis treated with buserelin decreased to an average of 164±32 pmol/l after 3 months of treatment, and in a study by W. Dmowski et al. [13] - up to 132±18 pmol/l, which is slightly higher than the 110 pmol/l value chosen as the end point in this study.
In 4 patients, a significant increase in estradiol levels was detected by visit 5, with a significant decrease in its levels by visits 3-4. In 1 patient, there was no significant increase/decrease in estradiol levels by visit 5, with a significant decrease in its level by visits 3-4. The reason could be a deviation in the date of visit 5 or the so-called “rebound effect,” when a short-term significant increase in the concentration of sex hormones is observed shortly after stopping the use of GnRH agonists.
Thus, 32 (64%) of 50 patients met the effectiveness criterion “Decrease in estradiol levels ≤110 pmol/l.” In general, for 45 (90%) patients out of 50, treatment with Buserelin-long FS was effective in terms of reducing estradiol levels, based on a significant decrease in estradiol levels relative to the initial level.
M-echo parameters
. At the visit during the screening period, as well as at visits 2–5, a transvaginal ultrasound examination of the uterus and appendages was performed to identify changes in the pathological structures of the myometrium in various degrees of endometriosis during treatment.
During treatment with Buserelin-long FS, a statistically significant decrease in endometrial thickness was observed already by visit 2 (Fig. 4).
Rice. 4. Changes in endometrial thickness during therapy with Buserelin-long FS.
Thus, 49 (98%) of 50 patients met the effectiveness criterion “Reducing the thickness of the median uterine echo to 4-6 mm.”
Results of endometrial aspiration biopsy
. To identify changes in the endometrium or endometrial atrophy during treatment with Buserelin-long FS, an endometrial biopsy was performed in patients during the screening visit and at visit 5. Based on the results of aspiration biopsy, in 33 out of 50 patients at visit 5, it can be concluded that in the majority of patients - 29 (88%) out of 33 - endometrial atrophy or a decrease in the degree of endometrial hyperplasia was observed at visit 5 in relation to the visit during the screening period.
Patient survey data.
At each visit, including the screening visit, patients completed a questionnaire. The questionnaire consisted of several questions, some of which made it possible to assess changes in the subjective perception of pain symptoms, in the physical and emotional state of the patients’ own health (“1. How would you rate the state of your health?”, “2. How would you rate the state of your health now compared to 4 weeks ago?", "3.1. To what extent does your health condition limit you from performing strenuous physical activities (lifting and carrying heavy objects, running, climbing several flights of stairs, walking several kilometers)? ", "3.2. To what extent does your health condition limit you from performing moderate physical activity (climbing one flight of stairs, walking several hundred meters, vacuuming or mopping the floor yourself)?", "3.3. To what extent does your health condition limits you from performing light physical activities (walking 100 m, dusting, getting dressed)?”, “4. How would you rate your physical condition now compared to 4 weeks ago?”, “5. How would you rate your emotional state compared to what it was 4 weeks ago?”, “6. How much physical pain have you experienced over the past 4 weeks?"). Patients could choose only one answer to each question.
Buserelin Depot or Long – which is better?
The manufacturer is the main point in which Buserelin Long and Depot differ from each other. The manufacturer Buserelin-depot purchases the active substance in China, and simply packages it in the Russian Federation. For Buserelin-long, everything is created in our own laboratory and is not purchased anywhere. From a clinical point of view, there is practically no difference - both drugs will work and have their effect. Which drug to choose depends entirely on the attending physician and the patient: some want to save money, others do not trust Chinese manufacturers or want to support domestic companies. In all other respects, both drugs are completely similar.