Is Xeplion dangerous?
Xeplion
Paliperidone (9-hydroxyrisperidone) is the active metabolite of risperidone, originally marketed as an oral extended-release formulation (ORal Osmotic System, OROS®, Alza Corporation) (Invega®, Janssen). Paliperidone long-acting injection (PLAI) is currently formulated as a suspension of paliperidone palmitate nanocrystals in an aqueous formulation (Invega Sustenna®, Xeplion®) administered monthly intramuscularly (in the deltoid or gluteal region). PLAI doses can be expressed in either milligram equivalents (mg-eq) of paliperidone palmitate or milligrams of the active fraction of paliperidone. Recommended initiation regimen: 150 mg eq (234 mg) on day 1 and 100 mg eq (156 mg) on day 8 (both injected into the deltoid muscle), rapidly reaching therapeutic blood levels without the need for oral administration. Monthly maintenance doses of paliperidone palmitate range from 25 to 150 mg eq. (39–234 mg; recommended dose of 75 mg eq. injected into deltoid (using adjusted weight needle) or gluteal muscle (using 1.5" 22 G needle). Day 8 dose may be given +/- 2 days, and monthly doses +/- 7 days without clinically significant effects on plasma concentrations.
In patients with mild renal impairment (creatinine clearance [CrCL]: 50-80 ml/min), the dosage should be adjusted. In patients with mild or moderate hepatic impairment, no dose adjustment is required; There are currently no data regarding severe liver failure. Elderly patients with normal renal function should receive the same dose as younger adult patients with normal renal function. If CrCL decreases with age, dosage should be adjusted accordingly. Treatment with paliperidone palmitate can be started the day after previous oral antipsychotic treatment is discontinued.
Xeplion, maybe, has nothing to do with it?
It is known that the mortality rate due to schizophrenia is two to three times higher than that of the general population, which corresponds to a reduction in life expectancy of 10-25 years. Natural death accounts for about 60% of mortality in patients with schizophrenia, and such patients are more likely to die from coronary heart disease. Since it has been suggested that more than half of sudden deaths in patients with schizophrenia are of cardiac origin, sudden cardiac death is mainly responsible for the reduction in their life expectancy. Many factors play a role in the premature death of people with schizophrenia, including a higher prevalence of smoking, poor diet, a more sedentary lifestyle and a greater likelihood of alcoholism and substance abuse.
Dyslipidemia, diabetes, and comorbid dyslipidemia and diabetes were more common in the group of unexplained deaths of patients in a psychiatric hospital. It is interesting to note that unexplained sudden deaths were not associated with increased use of first- or second-generation antipsychotics. Additionally, more than 50% of people with schizophrenia have been shown to have a reduced chance of achieving psychosocial goals.
QT segment prolongation
A prolonged QTc interval can cause potentially life-threatening arrhythmias. Almost all drugs used in psychiatric practice can prolong the QTc interval. There are some indications that psychiatrists are not sufficiently aware of the risks of QTc prolongation. By listing the risk factors associated with QTc prolongation and adjusting these factors as much as possible, the overall risk of potentially fatal arrhythmias can be reduced and more appropriate pharmacological treatment can be prescribed.
The effect of antipsychotics on the cardiovascular system of patients with schizophrenia
The range of mechanisms by which antipsychotics can affect the cardiovascular system of patients with schizophrenia is very wide and includes: receptor blockade; conduction disturbances (eg, bundle branch block); slow ventricular repolarization (prolongation of the QTc interval); left ventricular dysfunction; sinus node abnormalities; myocarditis; postural hypotension; polydipsia-hyponatremia syndrome; weight gain; glucose intolerance. Of these, QTc prolongation with the risk of progression to the potentially fatal ventricular tachyarrhythmia Torsades de Pointes (TdP) is of particular concern because this arrhythmia is unpredictable and difficult to control.
Xeplion administration protocol
Xeplion is administered in doses of 150 mg on the first day, 100 mg on the 8th day and 75 mg after the 4th week. Almost 85% of patients respond positively to treatment. No exacerbation of psychopathological symptoms of schizophrenia was found during treatment with Xeplion. The onset of clinical response was 8 days in patients receiving the recommended initial 150 mg eq. dose of paliperidone palmitate intramuscularly into the deltoid muscle on day 1.
Causes of death during xeplion therapy
From the launch of the long-acting injectable antipsychotic paliperidone palmitate (XEPLION) in 2013 to 2014, there were 32 deaths (estimated user population of approximately 11,000 patients) recorded in early post-marketing. The most common cause of death was sudden death (12 cases were sudden death defined by ICD-10 codes 96.0 and 96.1, and 4 cases presumed to be sudden death), followed by suicide (7 cases) and neuroleptic malignant syndrome (4 cases). Several deaths have occurred in patients with serious medical conditions such as cancer or pneumonia. . The risk of all-cause mortality in XEPLION was low compared with other studies; the risk of sudden death may be higher with XEPLION than with ZODIAC.
pharmachologic effect
Mechanism of action
Paliperidone is a centrally acting antagonist of dopamine D2 receptors, which also has high antagonism of serotonin 5-HT2A receptors. In addition, paliperidone is an antagonist of alpha1 and alpha2 adrenergic receptors and histamine H1 receptors. Paliperidone does not have affinity for cholinergic, muscarinic, or beta1- and beta2-adrenergic receptors. The pharmacological activity of the (+) and (-) enantiomers of paliperidone is the same in qualitative and quantitative terms.
The antipsychotic effect is due to the blockade of D2-dopaminergic receptors of the mesolimbic and mesocortical systems. Causes less suppression of motor activity and induces catalepsy to a lesser extent than classical antipsychotics (neuroleptics).
Balanced central antagonism of serotonin and dopamine may reduce the propensity for extrapyramidal side effects and expand the therapeutic effect of the drug to cover negative and productive symptoms of schizophrenia.
Paliperidone has an effect on sleep structure: it reduces the latency period before falling asleep, reduces the number of awakenings after falling asleep, increases the total duration of sleep, increases sleep time and increases the sleep quality index. It has an antiemetic effect and may cause an increase in the concentration of prolactin in the blood plasma.
Drug interactions
Caution should be exercised when prescribing Invega with drugs that prolong the QT interval.
Effect of paliperidone on other drugs
Paliperidone is not likely to be involved in clinically significant pharmacokinetic interactions with drugs that are metabolized by cytochrome P450 isoenzymes. In vitro studies using human liver microsomes have shown that paliperidone does not significantly inhibit the bioconversion of drugs that are metabolized by cytochrome P450 isoenzymes, including CYP1A4, CYP2A6, CYP2C8/9/10, CYP2D6, CYP2E1, CYP3A4 and CYP3A5. Based on this, there is no reason to assume that paliperidone will inhibit to a clinically significant extent the clearance of drugs that are metabolized by these enzymes. In in vitro studies, paliperidone did not induce the activity of CYP1A2, CYP2C19 or CYP3A4.
At high concentrations, paliperidone is a weak inhibitor of P-glycoprotein. No in vivo data available, clinical significance unknown.
Given the fact that paliperidone acts primarily on the central nervous system, it should be used with caution in combination with other centrally acting drugs and alcohol. Paliperidone may counteract the effects of levodopa and other dopamine agonists. Due to the ability of paliperidone to cause orthostatic hypotension, additive effects may occur when the drug is used concomitantly with other drugs that cause orthostatic hypotension.
A pharmacokinetic interaction between paliperidone and lithium is unlikely.
The simultaneous administration of Invega at a dosage of 12 mg 1 time / day and divalproex sodium tablets of prolonged release (at a dosage of 500-2000 mg 1 time / day) does not affect the pharmacokinetics of valproate. In clinical studies in patients taking a constant dose of valproate, plasma valproate concentrations were no different from those in patients taking Invega 3–15 mg with valproate.
The ability of other drugs to affect paliperidone
Paliperidone is not a substrate of the isoenzymes CYP1A2, CYP2A6, CYP2C9, CYP2C19 and CYP3A5. This indicates a low probability of its interaction with inhibitors or inducers of these enzymes. In vitro studies have revealed minimal involvement of the CYP2D6 and CYP3A4 isoenzymes in the metabolism of paliperidone, however, there is no evidence that these isoenzymes play a significant role in the metabolism of paliperidone in vitro or in vivo. In vitro studies have shown that paliperidone is a substrate of P-glycoprotein.
Paliperidone is metabolized to a limited extent by the CYP2D6 isoenzyme. In a study in adult volunteers, the interaction of paliperidone with paroxetine, a potential inhibitor of the CYP2D6 isoenzyme, did not observe a clinically significant change in the pharmacokinetics of paliperidone.
Coadministration of paliperidone with carbamazepine 200 mg twice daily caused a decrease in paliperidone Cmax and AUC by approximately 37%. This decrease was caused by a 35% increase in paliperidone clearance as a result of carbamazepine induction of renal P-glycoprotein. The small decrease in the amount of drug excreted unchanged suggests that carbamazepine has little effect on CYP metabolism or the bioavailability of paliperidone when coadministered. When prescribing carbamazepine, the dose of paliperidone should be re-evaluated and increased if necessary. Conversely, when carbamazepine is discontinued, the dose of paliperidone should be re-evaluated and reduced if necessary.
Paliperidone, which is a cation at physiological pH values, is excreted predominantly unchanged by the kidneys; in this case, about half of the excretion is due to filtration and about half is due to active secretion. The use of paliperidone concomitantly with trimethoprim, which is known to inhibit the active renal transport of cationic drugs, did not affect the pharmacokinetics of paliperidone.
When Invegav was co-administered at a dosage of 12 mg once daily and divalproex extended-release sodium tablets (2 tablets of 500 mg once daily), an increase in Cmax and AUC of paliperidone by 50% was observed. Consideration should be given to reducing the dose of Invega when co-administered with valproate based on the clinical assessment of the patient.
The concomitant use of paliperidone and risperidone has not been the subject of scientific research. Paliperidone is an active metabolite of risperidone and therefore increased paliperidone blood levels may occur when paliperidone and risperidone are used concomitantly.
Overdose
In general, objective and subjective symptoms of paliperidone overdose are increased pharmacologic effects of this drug, i.e., drowsiness and sedation, tachycardia and hypotension, QT prolongation, and extrapyramidal symptoms. Bidirectional tachycardia and ventricular fibrillation have been observed with overdose of oral paliperidone. In case of acute overdose, it is necessary to consider the possibility of toxic effects of several drugs.
When assessing the therapeutic needs of the patient and the effectiveness of overdose relief, it must be remembered that Invega is a drug with a prolonged release of the active substance. There is no specific antidote for paliperidone. Generally accepted supportive measures should be implemented. A good airway, as well as adequate oxygenation and ventilation, should be established and maintained. It is necessary to immediately organize monitoring of cardiovascular activity (ECG monitoring to identify possible arrhythmias). Arterial hypotension and collaptoid conditions are treated with intravenous administration of plasma-substituting solutions and/or sympathomimetic agents. In certain situations, gastric lavage is indicated (after intubation, if the patient is unconscious), administration of activated charcoal and laxatives. If severe extrapyramidal symptoms occur, m-anticholinergic blockers must be administered. Monitoring the patient's condition and monitoring basic physiological functions must be continued until the effects of the overdose are completely eliminated.
special instructions
Neuroleptic malignant syndrome
Antipsychotics, including paliperidone, are known to cause neuroleptic malignant syndrome (NMS), which is characterized by hyperthermia, muscle rigidity, instability of the autonomic nervous system, depression of consciousness, and increased serum concentrations of creatine phosphokinase. Myoglobinuria (rhabdomyolysis) and acute renal failure may also occur in patients with NMS. If a patient experiences objective or subjective symptoms of NMS, all antipsychotic medications, including paliperidone, should be immediately discontinued.
Tardive dyskinesia
Drugs with dopamine receptor antagonist properties can cause tardive dyskinesia, which is characterized by rhythmic involuntary movements, mainly of the tongue and/or facial muscles. If a patient experiences objective or subjective symptoms indicating tardive dyskinesia, the advisability of discontinuing all antipsychotic drugs, including paliperidone, should be considered.
QT prolongation
As with other antipsychotics, caution should be exercised when prescribing Invega to patients with a history of cardiac arrhythmias, congenital QT prolongation, and concomitant use with drugs that prolong the QT interval.
Hyperglycemia and diabetes mellitus
Hyperglycemia, diabetes mellitus, and exacerbation of existing diabetes mellitus were observed during treatment with Invega. Establishing a relationship between the use of atypical antipsychotic drugs and disorders of glucose metabolism is complicated by the increased risk of developing diabetes mellitus in patients with schizophrenia and the prevalence of diabetes mellitus in the general population. Given these factors, the relationship between the use of atypical antipsychotic drugs and the development of side effects associated with hyperglycemia is not fully established. In patients diagnosed with diabetes mellitus, glucose levels should be regularly monitored. Patients with risk factors for diabetes mellitus (eg, obesity, family history of diabetes) should have fasting blood glucose levels monitored at the start of treatment and periodically during treatment. All patients should be clinically monitored for symptoms of hyperglycemia and diabetes mellitus. Patients who develop symptoms of hyperglycemia while being treated with atypical antipsychotics should have their blood glucose levels monitored. In some cases, symptoms of hyperglycemia have resolved with discontinuation of atypical antipsychotic medications, but some patients require antidiabetic treatment despite discontinuation of the suspected drug.
Weight gain
Significant weight gain was observed during treatment with atypical antipsychotics. It is necessary to monitor patients' body weight.
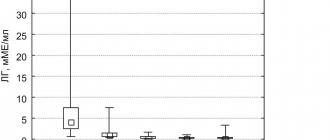
Hyperprolactinemia
Like other D2-dopamine receptor antagonists, paliperidone increases prolactin levels and this increase persists throughout drug administration. The effect of paliperidone is comparable to that of risperidone, the drug with the greatest effect on prolactin levels among other antipsychotic drugs.
Hyperprolactinemia, regardless of etiology, can suppress the expression of GnRH (gonadotropin-releasing hormone) in the hypothalamus, which leads to a decrease in the secretion of gonadotropins by the pituitary gland. This, in turn, can suppress reproductive function, reducing sexual steroidogenesis in women and men. Galactorrhea, amenorrhea, gynecomastia and impotence have been reported in patients taking drugs that increase prolactin levels. Long-term hyperprolactinemia associated with hypogonadism can lead to decreased bone density in women and men.
In vitro tissue culture studies have shown that approximately one third of human breast cancers are prolactin-dependent. This should be taken into account when prescribing drugs that increase prolactin levels to patients with previously diagnosed breast cancer. Clinical and epidemiological studies conducted to date have shown no association between atypical antipsychotic drugs and tumor formation in humans. However, the available data are too limited to draw definitive conclusions.
Orthostatic hypotension
Paliperidone has alpha-blocking activity and may therefore cause orthostatic hypotension in some patients. Paliperidone should be used with caution in patients with cardiovascular disease (for example, heart failure, myocardial infarction or ischemia, cardiac conduction disorders), cerebrovascular disease, and with conditions that contribute to arterial hypotension (for example, dehydration, hypovolemia and therapy with antihypertensive drugs ).
Body temperature regulation
Antipsychotic drugs are associated with such undesirable effects as disruption of the body's ability to regulate temperature. Caution should be exercised when prescribing paliperidone to patients with conditions that may contribute to an increase in core body temperature, such as intense exercise, dehydration, exposure to high external temperatures, or concomitant use of drugs with anticholinergic activity.
Antiemetic effect
Preclinical studies have demonstrated the antiemetic effect of paliperidone. This effect, when observed in humans, may mask objective and subjective symptoms of overdose of some drugs, as well as diseases such as intestinal obstruction, Reye's syndrome, and brain tumors.
Priapism
Drugs with alpha-blocking effects can cause priapism. Priapism has been reported in post-marketing studies of paliperidone.
Suicide attempts
The possibility of suicide attempts is characteristic of mental illness, so treatment of patients at high risk should be carried out under close supervision. In these cases, Invega should be prescribed in a minimum number of tablets to reduce the risk of overdose.
Leukopenia, neutropenia, agranulocytosis
Leukopenia, neutropenia and agranulocytosis have been observed with the use of antipsychotics, including the use of Invega. Agranulocytosis has been observed very rarely during post-marketing surveillance. In patients with a history of a clinically significant decrease in white blood cell count or drug-related leukopenia/neutropenia, a full blood count is recommended during the first months of therapy, and discontinuation of treatment with Invega should be considered at the first clinically significant decrease in the white blood cell count in the absence of other possible causes. Patients with clinically significant neutropenia are advised to be monitored for fever or symptoms of infection and to initiate treatment immediately if such symptoms occur. Patients with severe neutropenia (absolute neutrophil count less than 1 x 109/L) should discontinue use of Invega until the white blood cell count normalizes.
Venous thromboembolism
Cases of venous thromboembolism have been reported with the use of antipsychotic drugs. Since patients taking antipsychotic drugs are often at risk of developing venous thromboembolism, all possible risk factors should be identified before and during treatment with Invega and preventive measures should be taken.
Intraoperative floppy iris syndrome (ISID)
ISDR was observed during surgery for the presence of cataracts in patients receiving therapy with drugs of the α1-adrenergic receptor antagonist group.
ISDR increases the risk of complications associated with the organ of vision during and after surgery. The doctor performing such an operation should be informed in advance that the patient has taken or is currently taking drugs that have α1-adrenergic receptor antagonist activity. The potential benefit of discontinuing α1-adrenergic antagonist therapy before surgery has not been established and should be weighed against the risks associated with discontinuing antipsychotic therapy.
Pregnancy and child care
The patient should notify their physician of pregnancy or planning to become pregnant during treatment with Invega. Caution should be exercised when prescribing Invega to nursing mothers.
Alcohol consumption
Patients should avoid drinking alcohol during treatment with Invega.
Conditions leading to a decrease in the presence of the drug in the gastrointestinal tract
Conditions leading to a decrease in the presence of the drug in the gastrointestinal tract, for example, diseases associated with chronic diarrhea, may cause a decrease in the absorption of paliperidone.
Invega tablets are manufactured using osmotic release technology, in which osmotic pressure releases paliperidone at a controlled rate. The system, which looks like a capsule-shaped tablet, consists of an osmotically active three-layer core surrounded by an intermediate shell and a semi-permeable membrane. The three-layer core consists of two medicinal layers containing the drug substance and excipients, as well as an ejector layer containing osmotically active components. On the dome side of the drug layers there are two outlet holes made using a laser. In the gastrointestinal tract, the colored shell quickly dissolves, and water begins to flow into the tablet through a semi-permeable control membrane. The membrane controls the level of water intake, and this, in turn, controls the level of drug release.
The hydrophilic polymers in the tablet core absorb water and swell into a gel containing paliperidone, which is then expelled through holes in the dome. The insoluble components of the tablet are excreted from the body in the stool. Patients should not worry if they notice something that looks like a pill in their stool.
Impact on the ability to drive vehicles and operate machinery
Paliperidone may interfere with activities requiring rapid mental response and may also have visual effects, so patients should avoid driving or operating machinery until their individual sensitivity to paliperidone has been established.