COVID-19✓ Safe
Silicosis is a “blockage” of the lungs due to inhalation of air containing sand dust (quartz). Silicosis is quite common, as a type of severe pneumoconiosis.
Thus, dust is transported into the lungs. It is absorbed by cells of the immune system. Next, malfunctions occur in the “machine”: the lung tissues become deformed and clogged, first into tiny nodules, and then into large masses. In places of compaction, gas exchange does not occur, and the blood is not enriched with oxygen. It just becomes difficult to breathe.
Why does the disease occur?
The main cause of the disease is inhalation of dust, which contains:
- silicon dioxide (quartz);
- silicates;
- talc.
Workers in the following professions are susceptible to pathology:
- miners;
- glass blowers;
- miners;
- potters;
- sandblasters;
- stone carvers;
- quarry workers, etc.
The speed and severity of the disease development depend on several factors:
- The disease develops more severely and quickly when inhaling the free crystalline form of silicon than the bound form.
- The duration and strength of the influence of the causative factor influences. The longer a person's contact with high dust conditions lasts and the higher the concentration of silicon in the air, the faster the pathology develops.
- The more time has passed since the dust has been crushed, the less aggressive it is.
- Uncoated silica particles cause pulmonary silicosis more quickly.
Prevention of silicosis
The most effective measures must be taken in the workplace where a person works. This includes the process of insulation, ventilation, dust removal from production premises, and the use of abrasives that do not contain quartz. Breathing masks provide some benefit, but do not provide adequate protection.
Monitoring of exposed workers using questionnaires, spirometry, and chest radiography is recommended. In those workers who inhale quartz, future development of non-tuberculous mycobacterial infections and pulmonary tuberculosis should be suspected. Miners are primarily at risk. People exposed to quartz but without silicosis have a 3 times higher risk of developing tuberculosis compared to others. Miners diagnosed with silicosis have a risk of tuberculosis 20 times or more higher than other people. They are also more likely to have pulmonary and extrapulmonary manifestations.
Patients exposed to silica and with a positive tuberculin test and negative sputum culture for tuberculosis should receive standard chemoprophylaxis with isoniazid. Therapy is the same as in other cases of tuberculosis treatment. Relapses of the disease in question more often occur in those who have silicotuberculosis. In some cases, longer courses are needed than are usually prescribed.
How does it manifest?
There are two forms:
- chronic - occurs most often;
- acute - develops as a result of intense influence of the causative factor over a short period, 1–2 months.
Chronic silicosis occurs for a long time without clinical manifestations. The first symptom is shortness of breath. At the initial stage, it occurs during intense work, and then appears at rest. The cough comes later, when the bronchi are involved in the pathological process. Smoking intensifies it.
Over time, as the disease progresses, respiratory failure develops, which leads to heart pathology.
Patients experience chronic hypoxia (lack of oxygen) in the following manifestations:
- fatigue;
- earthy complexion;
- fingers like drumsticks;
- weight loss;
- persistent dry cough;
- chest pain;
- decreased breathing;
- flattening of the nail plate and its acquisition of the shape of watch glasses;
- decreased performance.
Acute silicosis manifests itself in the same way, the only difference is the rate of progression of symptoms. If in the chronic form respiratory failure develops over decades, then in the acute form it takes just 1–2 years.
Symptoms of silicosis
Symptoms of stage 1 silicosis:
- shortness of breath on exertion;
- coughing;
- loss of appetite;
- chronic fatigue;
- chest pain.
Symptoms of stage 2 silicosis:
- shortness of breath with little physical exertion;
- increased cough;
- constant chest pain;
- rapid breathing at rest;
- hard breathing;
- dry wheezing.
Symptoms of stage three silicosis:
- severe shortness of breath;
- painful cough with sputum production;
- attacks of suffocation;
- multiple dry wheezing;
- foci of wet rales;
- tachycardia (increased heart rate);
- dysfunction of the gastrointestinal tract;
- severe and frequent headaches.
If you experience similar symptoms, consult your doctor
. It is easier to prevent a disease than to deal with the consequences.
What diseases can silicosis be confused with?
The following pathologies exhibit similar symptoms:
- pulmonary tuberculosis;
- oncological diseases;
- interstitial fibrosis;
- Chronical bronchitis;
- tuberculoma;
- sarcoidosis
All these conditions are characterized by the appearance of cough and shortness of breath, loss of body weight and the subsequent development of respiratory failure.
They can be distinguished by conducting additional examination. Therefore, if you experience similar complaints, be sure to seek help from a doctor.
Preventing disease[edit]
Since the disease is incurable and irreversible
, then the only way to prevent it is to prevent excessive amounts of quartz from entering the respiratory system:
- The use of effective ventilation[8][9][10], air showers and other means to reduce the inhalation of dust containing quartz; remote control of machines.
- The use of sand-replacing materials during abrasive blasting, for example, cooper slag.
- Automation of technological processes and use of remote control
- Effective monitoring of the degree of air pollution using personal samplers, including personal PDM dust meters operating in real time [11] (which makes it possible to timely detect exceeding MPCs and take adequate corrective measures.
Respirators do not provide reliable protection from dust - “Coal” No. 3 2015
The use of respirators does not provide protection against silicosis. Causes:
- Due to insufficient attention to reducing dust in the air, dust concentrations can be very high.
- In the USSR and the CIS, miners are usually given half-mask respirators without forced air supply to protect them from dust. Their protective properties are unstable and low - in the USA, legislation prohibits their use when dust levels are > 10 MAC (see Expected degree of respirator protection). The quality of many masks developed half a century ago is very low. When you install a plastic bag instead of a filter in the F-62Sh (with a knitted seal) and moderate tension on the straps, you can breathe, all the air passes through the gaps between the mask and the face.
- Repeated measurements of the effectiveness of half-mask respirators in England and the USA during the actual work of miners have shown that workers cannot use them continuously - whenever required due to increased air pollution (need to talk, etc.). Therefore, in practice, the use of half masks reduces the pollution of inhaled air by an average of 3-8 times, which, given high air pollution, is not enough to reliably protect health.
Because different people have different shapes and sizes of faces, the same respirator fits differently on different workers' faces. If the face fits the mask, then there will be little unfiltered air leakage through the gaps between the mask and the face (the main reason for the low average efficiency) and ( this
worker) a respirator will provide reliable protection. The fact that respirators sometimes reliably protect some workers is confusing and makes it difficult to establish the overall ineffectiveness of the RPE used[12].
How to confirm the diagnosis?
A diagnosis of silicosis can be assumed if a person works in hazardous conditions. The presence of a causative factor together with typical symptoms should prompt a search for an occupational disease.
Pathology can be confirmed using imaging methods:
- computed tomography;
- X-ray examination of the chest organs.
In this case, the image will show small foci of darkening measuring 1–3 mm, mostly in the upper lobes of the lungs.
To differentiate silicosis from other diseases, bacteriological and cytological examination of sputum is performed.
To determine the severity of respiratory failure and the stage of development of the disease, spirometry is additionally performed, and the level of blood oxygen saturation is also examined.
Treatment:
A pulmonologist selects an individual treatment program based on the results of laboratory tests, diagnosis and severity of the disease. Although silicosis cannot be cured, its progression can be stopped. To do this, you need to “catch” the disease at an early stage and stop contact with sand.
The doctor may prescribe inhaled bronchodilators, steroid therapy, anti-inflammatory, immunomodulatory, and antiviral drugs. Often the attending physician prescribes vitamin therapy, physical therapy, diet, infusion, oxygen and drainage therapy.
Silicosis: treatment
The first thing to do to prevent the development of silicosis is to eliminate the influence of the causative factor - silicon dioxide.
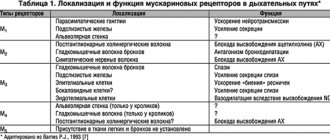
There is no treatment that would completely eliminate the disease. The main therapy is aimed at eliminating symptoms. Mainly used:
I. Bronchodilators to reduce shortness of breath and improve the quality of life of patients.
- Beta2 agonists:
- salbutamol;
- formoterol;
- salmeterol;
- fenoterol
- M-anticholinergics:
- short-acting: ipratropium bromide;
- long-acting: tiatropium bromide.
II. Anti-inflammatory therapy aimed at inhibiting the progression of inflammation and fibrosis:
- Inhaled glucocorticosteroids:
- budesonide;
- beclomethasone dipropionate;
- fluticasone propionate;
- mometasone furoate;
- ciclesonide;
- flunisolide.
- Methylxanthines:
- short-acting: aminophylline;
- long-term: theophylline, theotard, teopec.
If tuberculosis or bronchitis occurs, antibiotics and anti-tuberculosis drugs may be indicated. For a productive cough, use mucolytics: ambroxol, mucaltin and others.
The selection of the dosage of medications, course of treatment and regimens is carried out by a doctor specializing in occupational pathologies.
Pathophysiology of silicosis
Alveolar macrophages take up inhaled free quartz particles and enter the interstitial and lymphatic tissues. Macrophages promote the release of growth factors (tumor growth factor TNF-beta), cytokines (tumor necrosis factor TNF-alpha, IL-1) and oxidants, stimulate collagen synthesis, parenchymal inflammation and fibrosis.
After death, macrophages release silica into the interstitial tissue around small bronchioles, leading to the formation of a pathognomonic silicotic nodule. Such nodules contain mast cells, macrophages, lymphocytes, and fibroblasts with disorganized clumps of collagen and scattered biconvex particles, clearly visible under polarized light microscopy. When they mature, the nodule centers develop into dense balls of fibrous tissue with the classic onion skin appearance, which are surrounded by a layer of inflammatory cells.
If the effects are short-term or not intense, the nodules remain discrete and do not cause functional changes in the lung - simple chronic silicosis. But if there is a high intensity or prolonged exposure time (complicated chronic silicosis), the nodules merge, which becomes the cause of progressive fibrosis and reduction in lung volume (VOL, VC). Sometimes they form large masses - progressive massive fibrosis.
In the case of acute silicosis caused by intense exposure to quartz dust over a short period of time, the alveolar spaces are filled with PAS-positive protein-like substrates, similar to those detected in silicoproteinosis. The alveolar septa are saturated with mononuclear cells. An occupational history of short-term exposure is required to differentiate silicoproteinosis from idiopathic changes.
Alternative Methods
To improve the condition and general health of patients with occupational diseases, sanatorium treatment, inhalations and physiotherapy are recommended. To improve the cleansing of dust from the respiratory tract, alkaline and alkaline-salt inhalations are performed. This helps to liquefy sputum, activate the integumentary epithelium of the bronchi and remove dust. The procedure is done using a nebulizer; a 2% sodium bicarbonate solution is poured into the device. Breathe the medicine for 5–7 minutes. The course of treatment is 14–20 days and is repeated regularly throughout the year.
Physiotherapy uses UHF (high frequency electric field rays).
Prevention
Prevention of silicosis involves the following actions:
- carrying out anti-dust measures;
- use of personal protective equipment against dust;
- shortened working hours for people working in risk areas;
- early retirement;
- consumption of dairy products, which contribute to the rapid removal of harmful substances from the body;
- regular preventive examinations by specialists. a pulmonologist
twice a year . - treatment and recovery in a sanatorium.
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice.
The most common complications of silicosis
Without proper treatment and control of the disease, it becomes more complicated:
- pulmonary hypertension (increased pressure in the blood vessels of the lungs);
- emphysema (increased airiness of the lung tissue as a result of loss of elasticity of the alveoli);
- respiratory and heart failure;
- nocardiosis;
- systemic sclerosis;
- tuberculosis;
- spontaneous pneumothorax;
- chronic kidney pathology;
- lung cancer.
The risk of developing tuberculosis in patients with silicosis of any form is 30 times higher compared to other diseases.
Diagnostics
The X-ray method is used and an anamnesis is collected. A biopsy is appropriate for confirmation if radiography provides confusing or inaccurate findings. If there is any doubt whether it is silicosis or another disease, the doctor may prescribe any additional tests.
Chest x-ray or CT scan shows multiple round infiltrates or nodules that range in size from 1 to 3 mm. Their usual location is the upper pulmonary fields. Computed tomography (CT) is considered a more sensitive method than x-rays, especially if spiral CT or high-resolution CT is used.
The severity of the disease is determined using a standardized scale created by the International Labor Organization. A similar scale for CT has not been created. Calcified lymph nodes of the roots and mediastinum are often found; in some cases they may have the appearance of an eggshell. Pleural thickenings are rarely found; The exception is cases when severe damage to the parenchyma is not adjacent to the pleura. Rarely, calcified pleural lesions occur in patients in whom a small area of parenchyma is affected.
Bulls are usually created around conglomerates. There may be tracheal deviation if the conglomerates become large and lead to volume loss. True cavities may indicate the development of tuberculosis. The radiograph for many diseases is the same as for chronic silicosis. Therefore, silicosis is differentiated from the following diseases:
- hemosiderosis
- welders' siderosis
- chronic beryllium disease
- sarcoidosis
- coal workers pneumoconiosis
- hypersensitivity pneumonitis
- metastatic tumors in the lungs
- fungal infections
- miliary tuberculosis
Eggshell-like calcification of the hilar and mediastinal lymph nodes may help distinguish silicosis from other pulmonary diseases. Often this sign is not detected.
Rapidly progressive silicosis gives the same radiographic data as S. in its chronic form. It differs only in its rapid development.
Acute silicosis is characterized by rapid development of manifestations and diffuse alveolar infiltrates in the basal parts of the lungs on radiographs due to filling of the alveoli with fluid. Computed tomography reveals areas of ground-glass density that consist of reticular infiltration and areas of focal consolidation and heterogeneity. Multiple round opacities that doctors detect in progressive and chronic silicosis are not detected in the acute form of the disease in question.
Silicosis conglomerate is recognized by confluent darkening more than 10 mm in diameter against the background of chronic silicosis.
Additional research in silicosis
Computed tomography of the chest can be used to differentially diagnose (distinguish) silicosis and asbestosis. Although often for these purposes it is enough to collect an anamnesis (the impact of disease-causing factors on the patient’s body is determined) and x-ray examination. CT is recognized as a more informative method that detects the transition of simple silicosis to silicosis conglomerate.
In recognizing silicosis and disseminated tuberculosis or malignant neoplasm, the following studies are important:
- sputum analysis
- tuberculin test
- cytological examination
- PAT
- CT
- bronchoscopy
Pulmonary function tests (PFTs) and gas exchange are used not for diagnosis, but to monitor the development of the disease. In early chronic silicosis, there may be reduced lung volumes that are at the lower limit of normal, with normal functional residual volume and capacity. In silicosis conglomerates, pulmonary function tests show reduced lung volumes, DL, and airway obstruction. Arterial blood gases reveal hypoxemia, usually without CO2 retention. Testing gas exchange during exercise using pulse oximetry or, preferably, an arterial catheter is one of the most sensitive measures of deterioration in pulmonary function.
Antinuclear antibodies and increased rheumatoid factor are also found in some cases. They may indicate that the patient also has a connective tissue disease. There is an additional risk of progression to systemic sclerosis in those diagnosed with silicosis. Some patients develop rheumatoid arthritis, and pulmonary rheumatoid nodules are formed, 3-5 mm in size. They can be detected during a computed tomography or x-ray examination.
Popular questions about silicosis
How dangerous is the disease?
The development of respiratory and heart failure, which worsens the quality of life and reduces its duration.
How does it manifest?
The chronic form can be asymptomatic for a long time. Subsequently, shortness of breath and dry/wet cough appear. For acute silicosis, the symptoms are the same, but develop faster.
Can it be cured?
No, but you can improve your quality of life and slow down the progression of the disease.
general description
Silicosis (from the Latin silicium - “silicon”) is a pathological condition that develops as a result of prolonged inhalation of dust particles, including free silicon dioxide. Silicon dust is produced during many industrial processes: gold, tin and copper mines, stone cutting and polishing, glass production, metal smelting, pottery and porcelain production. Miners, foundry workers, stonemasons, potters and sandblasting workers, and drillers are susceptible to the disease. Silicosis is the most common occupational lung disease, occurring mainly in adults over 40 years of age.
Silicon dust has a chemical effect on the protoplasm of cells, leading to its necrosis. Silicon particles accumulate in the peribronchial lymphatic system. Subsequently, inflammation occurs, which ends in fibrosis of blood vessels and bronchi. Due to the development of fibrosis, they are compressed and atelectasis, bronchiectasis are formed, and pulmonary emphysema appears. The process affects both lungs evenly and simultaneously, somewhat less in the area of poorly ventilated apexes. It is believed that 15 years of work in hazardous production conditions without respiratory protection is guaranteed to lead to the development of silicosis. If the dust concentration is high, the disease can develop within one year. In this case they talk about acute silicosis. Often the disease occurs years after stopping contact with silica dust. This type of silicosis is called acute.