Fractures of the bones of the hand are injuries in which the integrity of the bones of the wrist, metacarpus or phalanges of the fingers is disrupted. These are common injuries, accounting for about a third of all bone fractures. This trend is associated both with the relative fragility of the hand, adapted for performing fine manipulations, and with its high activity. A fracture can occur as a result of a fall on a bent hand, a blow from a fist, the edge of the palm or fingers, or a direct blow to the hand.
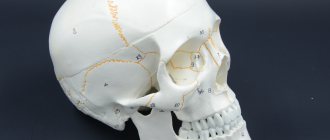
The bone apparatus of the hand consists of 27 bones of three sections - the wrist, metacarpus and fingers. The wrist consists of 8 spongy bones arranged in two rows - proximal, closer to the forearm, and distal, closer to the metacarpus. The first, proximal row, starting from the thumb, are the scaphoid, lunate and triquetral bones, which form an articulation with the radius bone of the forearm - the wrist joint. The fourth bone of the proximal row, the pisiform, does not participate in the formation of the wrist joint.
The second, distal row - the polygonal, trapezoid, capitate and hamate bones - connect to the five tubular bones of the metacarpus, radiating from the wrist. The distal ends of the metacarpal bones form five metacarpophalangeal joints - the connections of the metacarpus with the fingers. The first finger of the hand consists of two phalanges, the rest - of three. The phalanges of the fingers - short tubular bones - are connected to each other by interphalangeal joints.
The bones most susceptible to fractures are the phalanges and metacarpal bones. Wrist bones are broken quite rarely. The vast majority of injuries to the bones of the wrist occur as a result of a fracture of the scaphoid bone; the lunate and pisiform bones are less commonly affected. Fractures of the hamate and distal carpal bones are practically never encountered in clinical practice.
Fractures of the bones of the hand are accompanied by sharp pain and swelling in the area of damage; when bone fragments are displaced, deformation of the hand is possible. A hematoma may appear at the site of swelling. With some fractures, you can feel the displaced bone fragments under the skin or hear their crepitus. The diagnosis can be established by a traumatologist, who will clarify the complaints, ask in detail about the mechanism of injury, examine and palpate the fracture area, and check the preservation of movements in the joints. The diagnosis is confirmed by an X-ray examination of the hand, which can visualize the fracture line, assess the degree of displacement of fragments and, as a result, determine treatment tactics.
Treatment of hand fractures includes mandatory immobilization with a plaster cast for a period of 3 to 8 weeks. In case of displacement of fragments, closed reduction is performed; if it is ineffective, skeletal traction or osteosynthesis is performed. Careful comparison of fragments and consolidation of the fracture are important to preserve not only the aesthetics of the hand, but also its full function.
Classification of hand bone fractures
Depending on the presence or absence of skin damage over the fracture, the following are distinguished:
- closed fractures - the integrity of the skin is not compromised;
- open fractures - in the area of damage there is a wound in which bone fragments can be identified.
According to the position of bone fragments:
- without displacement - the broken bone maintains its position, the fragments exactly touch along the fracture line;
- with displacement - bone fragments diverge to the sides and, as a result, cannot heal along the fracture line without their comparison - reposition.
According to the involvement of articular structures in the fracture:
- extra-articular fractures - the fracture line passes outside the joint cavity;
- intra-articular fractures - the fracture line is located inside the joint cavity;
- fracture-dislocations - a violation of the integrity of the bone in combination with a dislocation in the adjacent joint.
According to the location of the fracture:
- wrist bone fractures;
- metacarpal bone fractures;
- fractures of the phalanges of the fingers.
You can also classify hand fractures depending on the number of fragments, degree of displacement, and infection. The etiology of the fracture is also important - whether it was traumatic or pathological - arising against the background of bone disease. All these factors influence the choice of treatment tactics for fractures and, ultimately, the possibility of completely restoring the function of the damaged hand.
Finger bones
Each finger consists of three phalanges: proximal, middle and distal. The exception is the first finger, which has only two phalanges - proximal and distal. The proximal phalanges are the longest, the distal phalanges the shortest. Each phalanx has a middle part - a body and two ends - proximal and distal. At the proximal end is the base of the phalanx, and at the distal end is the head of the phalanx. At each end of the phalanx there are articular surfaces for articulation with adjacent bones.
Wrist fractures
The bones of the wrist, due to their shape, structure and position, are broken quite rarely. The most susceptible bone to fracture is the scaphoid, the large bone at the base of the big toe. Injuries to the lunate and pisiform bones of the wrist also occur. The triquetral bone, as well as the bones of the distal row - polygonal, trapezoid, capitate and hamate - are subject to fractures extremely rarely; usually their fractures are combined with dislocations in the corresponding joints.
Scaphoid fractures
The cause is a fall on a bent hand, a blow with a fist, or a direct injury to the wrist. The following options are possible:
- intra-articular fracture of the scaphoid - the fracture line is located inside the cavity of the wrist joint;
- extra-articular fracture - separation of the tubercle of the scaphoid;
- de Quervain's fracture-dislocation - a simultaneous fracture of the scaphoid and dislocation of its proximal fragment and the lunate from the wrist joint.
Symptoms are pain and swelling at the base of the thumb, inability to move the hand at the wrist joint, or clench the hand into a fist. The diagnosis is established based on the patient’s complaints, data on the nature of the injury, examination and radiography of the hand bones. Sometimes, in the absence of displacement of fragments, the fracture line with all its signs is not determined. In this case, immobilization is still carried out with repeated radiography after 7-10 days, when, due to the activation of regenerative processes, the fracture line becomes clearly visible.
Treatment is immobilization with a plaster cast for a period of 4 weeks, followed by monitoring and prolongation of immobilization in case of insufficient consolidation of the fracture. In case of displacement of fragments and fracture dislocation, closed reduction is ineffective; fixation of fragments of the scaphoid bone with a wire is indicated. Fractures of the scaphoid are often complicated by the development of a false joint or lysis of bone fragments due to damage to the blood vessels supplying them during injury. Therefore, it is important to follow all the doctor’s recommendations and take control photographs in a timely manner to avoid complications and deterioration in the function of the wrist joint. After restoring the integrity of the scaphoid bone, physiotherapeutic treatment and exercise therapy are indicated to restore hand function.
Lunate fractures
The cause is a fall on a bent hand or direct injury, a blow to the wrist. It manifests itself as pain and swelling, intensifying with movements in the third, fourth and fifth fingers and with extension of the hand. The diagnosis is established taking into account complaints, the mechanism of injury, an objective examination of the area of damage and the results of an x-ray examination. To treat a lunate fracture, a plaster cast is applied for 4-8 weeks. Recovery usually proceeds without complications.
Fractures of the pisiform bone
The cause is a blow with the edge of the palm or direct injury. It manifests itself as pain and swelling of the wrist on the little finger side, increasing pain when it moves. The diagnosis is made taking into account complaints, anamnesis of injury, examination of the area of damage and radiography of the bones of the hand. For complete consolidation of a fracture of the pisiform bone, 4-5 weeks of immobilization are sufficient. The injury is rarely complicated.
Structure of the wrist bones
The hand performs a large number of tasks.
This is achieved due to the peculiarities of its structure. Bones and joints form a unique motor system. This article will examine in detail the issue of the structure of the carpal bones. The hand is a complex set of joints, which is a distant structural link of the upper limb girdle.
Articular wrist complex
The grasping abilities of the hand directly depend on the wrist joint complex. The ideal position of the hand is ensured thanks to the well-coordinated cooperation of the two joints that make up the wrist complex:
- wrist;
- midcarpal.
The spatial orientation of the hand is provided by the auxiliary abilities of the distal epiphyses of the forearm. The inferior radioulnar joint unites the ends of the ulna and radius bones. Although it does not belong to the hand, it plays an important role in its functioning, namely, it ensures its rotation. This strikingly distinguishes the human hand from the skeletal formations of animals.
Brief description of the wrist joint
The wrist joint looks like an ellipse. Its anatomical features are as follows:
- The lower epiphysis of the wrist joint (from the side of the forearm) is formed from the radius.
- The wrist joint is formed from the three bones of the nearest row on the side of the wrist. These are the lunate, scaphoid and triquetral bones.
- The three bones are covered with a hyaline plate, resulting in a solid articular surface.
Characteristics of the midcarpal joint
This is an atypical joint, which is located between two rows of carpal bones, forming a solid plane. Movement of the joint is possible due to the characteristics of the lunate bone. Its significance is compared to the axis around which movement is carried out, which has a limited scope. The stability of these processes is achieved thanks to the work of the ligamentous apparatus.
Interestingly, the strength of the ligaments is very high. If damaged, it is more likely that one of the small carpal bones will dislocate or, in extreme cases, break, than the ligaments will tear.
Imagine the structure of the wrist with its small bones, like a bag filled with small stones. Thus, it is easier to understand the nature of movements and interosseous interaction, possible thanks to the work of ligaments that guarantee the stable functioning of this connection.
All joints that make up the wrist take part in every movement. Flexion of the hand by 50º is possible due to the work of the wrist joint. 35º flexion is provided by the midcarpal joint. In turn, extension of the hand by 50º is achieved thanks to the mid-carpal joint, and by 35º – by the wrist.
Physiological and anatomical characteristics of the hand
Modification of the shape of the hand is the main condition for performing the grasping function. Therefore, in order to grasp an object and hold it, the hand must form a concavity or flatten when resting on a flat surface. Thanks to this, 3 arches are formed, which are located in different planes:
- Due to the concavity of the wrist, a transverse arch is formed.
- An inclined arch is formed due to the opposition of the thumb to the other fingers. This movement creates a palmar depression.
- The longitudinal arch is formed by the carpal bones, which arise from the metacarpophalangeal joints.
The joints of the wrist and metacarpus contribute to the development of the arch of the palm. They are connected by a ligamentous apparatus, and are also highly mobile and consist of the distal carpal joints and the proximal metacarpal bones. On the side of the wrist, the trapezoid bone is associated with the first and second metacarpal bones. The first trapezio-metacarpal joint provides the thumb with a counterpoint to its fellows. This joint differs from the others in its saddle-shaped shape. The main difference between the joint is that it has greater freedom and range of movement, which is possible due to the fact that the capsule is not stretched. There is also a drawback: such freedom leads to the fact that dislocation of the thumb occurs more often than in others.
The conjugation of the metacarpophalangeal joints ensures the flexion and extension of the fingers with a considerable range. The joints are saddle-shaped. The head of the metacarpal bone is biconvex, and the base of the first phalanx is biconvex, but the area of the base of the phalanx is less than that of the metacarpal bone.
It is noteworthy that if the planes of the joints were more equal, then the likelihood of their displacement relative to each other would decrease. Moreover, such a situation would significantly worsen the dexterity of the hand, which, of course, is unacceptable.
The metacarpophalangeal joint allows for a wide range of movement. Interestingly, the muscles and tendons of the fingers turn them into circular ones. The index finger has the greatest ability to move to the right and left.
Brief description of interphalangeal joints
Interphalangeal joints allow human hands to hold tools. The activity of the joints is supported by the thumb. His task is to press the object into the palm of his hand and hold it. The interphalangeal joints resemble balls in appearance, which allows the fingers to bend/extend.
There is a block-like concavity in the middle of the base of the phalanx. The head of the next phalanx has two small projections that are covered with hyaline cartilage. In the middle of the phalanx head is the central ridge. A distinctive characteristic of the joint is that the range of flexion exceeds 90º. However, the ligaments of the phalanges and interphalangeal joints prevent the joint from bending as much.
The structure of the bones of the wrist improves the grasping capabilities of the palm. No living creature can perform such complex manipulations with a brush that are accessible to humans.
Metacarpal fractures
The long, thin metacarpal bones are often broken by a punch or direct trauma. Muscle traction and movements in the hand until the fracture is immobilized often lead to displacement of bone fragments. There are epiphyseal fractures, when the fracture line is localized in the area of the bone heads, and diaphyseal fractures, when the fracture line is located in the bone body.
First metacarpal fracture
The cause is a blow with a bent first finger, less often a direct blow to the first metacarpal bone.
Fracture of the base of the first metacarpal bone . A typical injury for boxers and MMA fighters. A Bennett fracture is a separation of the base of the first metacarpal bone, which is held by ligaments, with simultaneous dislocation of most of it in the carpometacarpal joint. Rolando's fracture is a comminuted fracture-dislocation of the first metacarpal bone. Both injuries present with pain, deformation and swelling in the “anatomical snuffbox” area - the area under the base of the first finger - with increased pain when moving or trying to make a fist. Diagnosis is carried out taking into account complaints, trauma history, examination of the area of injury and x-ray of the hand. Bennett and Rolando fractures are treated surgically using osteosynthesis - restoring bone integrity by fixing fragments with metal knitting needles, pins or plates.
Fracture of the middle part of the first metacarpal bone . More often it occurs due to a direct blow to the bone. It manifests itself as pain, swelling and deformation in the area of the first metacarpal bone. The diagnosis is established taking into account the patient's complaints, information about the mechanism of injury, examination of the area of the first metacarpal bone and x-ray examination of the bones of the hand. Treatment is plaster immobilization for a period of 4-5 weeks; if the fragments are displaced, preliminary closed reposition is required. If conservative reduction is ineffective, an operation - pin osteosynthesis - is performed to compare the fragments.
An example of Dr. Valeev’s operation to restore after a fracture of the first metacarpal bone:
Before surgery:
After operation:
Fracture of II, III, IV, V metacarpal bones
The cause is a blow with a fist or a fall on fingers clenched into a fist. They can be single, but more often several metacarpal bones are broken, usually the fourth and fifth. It manifests itself as pain, swelling and deformation of the hand, and a hematoma often occurs. Diagnosed on the basis of complaints, history of injury, objective examination and X-ray results of the bones of the hand. To treat a non-displaced fracture, immobilization is performed for a period of 4-5 weeks. If fragments are displaced, closed reduction is indicated, and if it is ineffective, skeletal traction or pin osteosynthesis is indicated.
Metacarpal bones
The metacarpus consists of five tubular metacarpal bones. The metacarpal bone of the first finger is shorter than the others, but is distinguished by its massiveness. The longest is the second metacarpal bone. The following bones towards the ulnar edge of the hand decrease in length. Each metacarpal bone has a base, a body and a head.
The bases of the metacarpal bones articulate with the bones of the wrist. The bases of the first and fifth metacarpal bones have saddle-shaped articular surfaces, and the rest have flat articular surfaces. The heads of the metacarpal bones have a hemispherical articular surface and articulate with the proximal phalanges of the fingers.
Fracture of the phalanges of the fingers
The cause is a blow with the fingers, an injury while fixing the fingers, or a direct blow to the phalanges. Fractures of the phalanges of the fingers can be:
- intra-articular;
- extra-articular;
- single;
- multiple - within one finger or several;
- combined with dislocations in the metacarpophalangeal or interphalangeal joints.
Symptoms: pain, swelling, hematoma, deformity. The pain intensifies when you try to move your fingers. The diagnosis is established on the basis of complaints, trauma history, objective examination and X-ray results. To treat a fracture of the phalanges of the fingers without displacement, fixation is performed with a plaster cast for 3-4 weeks. In case of fracture-dislocations, joint reduction is performed; in case of displacement of fragments, closed reduction is performed. If it is not possible to compare the fragments using a closed method, skeletal traction or pin osteosynthesis is indicated.