Pancreatitis is a disease of the pancreas associated with the development of an inflammatory process in the organ. With this disease, there is a disruption in the flow of enzymes involved in digestion from the pancreas to the duodenum. Digestive enzymes remain in the gland itself and destroy it. The main cause of this disease is improper and unbalanced nutrition. That is why the treatment of pancreatitis is based on a properly selected diet.
General rules. Duration of the diet.
Maintaining proper nutrition is the key to a quick recovery. With this diet, you must adhere to certain rules to eliminate the possibility of complications.
General diet rules:
- Overeating should be avoided
- Meals should be fractional, at least 5-6 times a day
- Food should be warm. It is necessary to completely exclude hot and cold foods.
- Eliminate raw vegetables and fruits and fiber-rich foods from your diet.
- Food should only be prepared using recommended methods.
Symptoms of pancreatitis
Main symptoms of pancreatitis :
- Feeling of fullness in the stomach after eating.
- Pain in the navel area.
- Constant heartburn, bloating and flatulence.
- Nausea.
- Bad breath.
- Belching.
- Swelling of the face (read a useful article on how to quickly get rid of swelling on the face).
- Fat stool.
- Dry skin.
- Redness of the skin.
In addition, a large number of toxins accumulate in the body, which can poison the body.
Nutrition for pancreatitis during exacerbation:
In case of exacerbation of pancreatitis, it is necessary to avoid eating any food for several days. During fasting, it is recommended to drink purified still water. The daily volume of water should be no more than 1.5-1.7 liters. After the pain and symptoms subside, you can add low-calorie food in small quantities to the diet (liquid cereals, vegetable soups, steamed fish or chicken cutlets).
If you do not follow a diet during acute pancreatitis, the disease can quickly become chronic.
Notice!
During the acute period, sanatorium-resort treatment is contraindicated: it is better to go to a hospital.
If you have a chronic
form, then you should regularly
carry out preventive treatment
.
Factors of occurrence and symptoms of pancreatitis
The course of pancreatitis is characterized by constant relapses, which occur due to the release of insufficient amounts of hormones and enzymes. The point is not even in constant relapses, but in the fact that with each subsequent one the condition worsens. The tissues are gradually destroyed, which subsequently threatens serious health problems.
It is very important to remember that inflammation of the pancreas can indicate the independence of the disease, or be a manifestation of other pathologies (liver cirrhosis, alcohol intoxication or atherosclerosis).
List of permitted products:
| Cereals (buckwheat, oatmeal, rice, semolina) | The cereal must be boiled in water, followed by the addition of milk and a small amount of butter. |
| vegetables | Vegetables can be consumed as first courses (vegetable soups, puree soup) or in the form of chopped boiled pieces. Allowed fruits include potatoes, carrots, green peas, zucchini, pumpkin, beets and cauliflower. |
| fruits | Raw fruits should not be eaten. You can eat fruit jams, marshmallows, baked apples, compotes, and jelly. |
| meat | You can eat lean meats: beef, veal, rabbit and chicken. The meat is steamed and prepared in the form of soufflés or minced meat cutlets. |
| fish | Steamed white river fish is allowed in the food. |
| egg | Allows you to prepare a steam omelet from 1 chicken egg or 3 quail eggs. |
| Dairy | Dairy products should have minimal fat content |
| bread | You can eat a small amount of wheat bread 2-3 days old |
Features of a special diet
What can you eat if you have inflammation of the pancreas ? The diet of a person who suffers from pancreatitis should contain a sufficient amount of protein. But fat should be present in minimal quantities. This optimizes the functioning of not only the pancreas, but also the gallbladder. If you add fat, it should only be of vegetable origin, and even then in small quantities. Protein will serve as a building material for restoring the structure of the pancreas. Such patients can consume carbohydrates. Only if the risk of developing diabetes is increased, then their quantity also needs to be moderated.
diet for pancreatitis
In addition, it is worth significantly limiting the level of salt in your diet. The fact is that with pancreatitis the gland swells, which causes pain. It is the reduction in the level of salt in the diet over three weeks that will lead to normalization of its size. In case of serious exacerbation of the pathology, you need to eat only pureed and gentle food. All food for pancreatitis should be warm so as not to cause irritation and is better absorbed. All food should be bland, no seasonings or spices. Only fresh and high-quality products.
Over time, you need to enrich your diet with meat, fish, egg whites and dry bread. But meals for pancreatitis should be small, although frequent. Eating up to six times a day is considered optimal.
List of fully or partially restricted products:
| Dates, grapes, bananas | Causes bloating |
| Mushrooms, legumes, white cabbage | Contains coarse fiber |
| Smoked, salted, fast food, products containing preservatives and dyes | Irritate the mucous membrane of the digestive tract |
| By-products (liver, tongue, heart, kidneys, etc.) | Contains a lot of cholesterol |
| Any fried or fatty foods | Lead to exacerbation of the disease |
| High fat dairy products | High risk of exacerbation or complication of the disease |
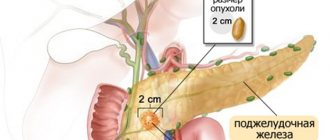
Anatomy and functions of the pancreas
Nutrition plays a huge role in the treatment of pancreas
The human pancreas is the most important mixed secretion gland. This organ releases hormones into the blood and synthesizes digestive enzymes, which are necessary for the absorption of proteins, carbohydrates and fats.
The pancreas is located in the abdominal cavity next to the stomach and small intestine. This organ is functionally connected to the duodenum, where enzymes are released during digestion.
Main functions of the organ:
- Breakdown of complex protein, lipid and carbohydrate substrates into simple components.
- Release of glucagon and insulin into the blood. These hormonal substances affect the metabolism of carbohydrates in the body.
- Damage to areas of the organ that synthesize insulin is one of the causes of diabetes mellitus.
The pancreas is often exposed to various pathological factors. This may be inflammation of the glandular tissue as a result of blockage of the excretory ducts, infection and the growth of malignant cells. In this case, diseases of the organ affect both digestive and metabolic functions.
Dietary goals
In the treatment process, it is important to protect the pancreatic gland as much as possible from the effects of stimulating substances in order to make it possible to restore the functioning of undamaged cells and compensate for the loss of replacement with fibrous tissue.
To do this, the diet for chronic pancreatitis must include:
- exclusion of irritating substances (animal fat, essential oils, extractives, salt, hot seasonings);
- a gentle effect on the stomach and intestines using food processing methods (grinding to grinding, boiling, steaming, stewing) while avoiding fried and smoked foods;
- temperature control - the patient is allowed to eat ready-made meals with a temperature of about 38 degrees, cold drinks, ice cream and too hot products are prohibited;
- to restore intestinal function, products that enhance fermentation processes and are rich in fiber are excluded from the diet;
- in order to support protein and fat metabolism, ensure energy reserves, the daily and weekly menu includes the required amount of carbohydrates, protein products, and reduces coarse fats;
- providing vitamins necessary to support the functioning of the body and restore immunity;
- maintaining a frequency of meals of at least 6 per day, reducing portions to 250–300 g, avoiding one-time overeating.
A diet for chronic pancreatitis in adults requires a complete abstinence from alcoholic beverages (including beer), dry food, and canned foods.
Forms of pathology
There are several forms of pancreatic inflammation. People of any age can suffer from them: children, adults and the elderly.
- Acute pancreatitis. Develops over several hours, usually after eating a large amount of food. Patients experience severe nausea with vomiting, pain in the upper abdomen, accompanied by diarrhea, bloating and belching. Severe fever is likely: heavy sweating, high body temperature, weakness. During the destructive process, abscesses and foci of necrosis arise, requiring immediate surgical intervention.
- Reactive interstitial pancreatitis is a type of acute form of inflammation, more typical for childhood. It is manifested by high anxiety temperature with sharp abdominal pain, accompanied by swelling of the gland and the release of the enzyme trypsin, which destroys its tissue. This process is reversible, unlike necrotizing, but also requires urgent medical intervention.
- Chronic pancreatitis. It may not make itself felt for decades, and the period of remission is asymptomatic. During exacerbations, it is manifested by severe dyspepsia, abdominal pain, loss of appetite, general intoxication, and fever. Often accompanied by chronic cholecystitis or gastritis, it requires regular maintenance therapy and lifestyle adjustments.
Pancreatitis causes disturbances in the functioning of the liver, gastrointestinal tract, vascular system, and kidneys. In most cases, the inflammatory process does not affect the endocrine functions of the gland and is not associated with the development of diabetes mellitus.
What is recommended to avoid?
Prohibited foods for pancreatitis include those that are difficult and take a long time to digest, and are also strong irritants of the gastrointestinal tract and, accordingly, the pancreas:
- rich meat, fish and mushroom broths and soups;
- smoked varieties of sausages and smoked products in general;
- canned food and marinades;
- fresh baked goods and bread;
- spinach, sorrel, garlic, radish, radish;
- raw vegetables;
- vinegar, mustard, pepper;
- hot and spicy sauces and seasonings;
- alcohol, strong tea and coffee.
This list is general; it can be expanded due to the characteristics of the body, the course of the disease, the form of pancreatitis (acute or chronic in remission), as well as the age and nutritional status of the patient.
Sample menu
Pancreatitis and nutrition are interconnected things, so it is necessary to follow dietary nutrition constantly. If an adult or a child has an aggravated disease, then for the first 24 hours it is recommended to stop eating food altogether. Then for the next 3 days you should follow a strict diet, which is described in the table.
Diet for 3 days for acute pancreatitis
The doctor should also tell you about a sample menu for acute pancreatitis. As for food that can be consumed during the remission stage of the disease, it must be said that it can be prepared from all of the above products. You can prepare various soufflés, salads, soups, etc. If you don’t have enough imagination and you can’t create a diet yourself, you can use the following menu, which will allow you to diversify your diet throughout the week.
Menu for the week
Every person should understand that everything depends on nutrition during pancreatitis. If you just constantly take pills and eat everything, it will be impossible to achieve positive dynamics.