Palpitations and tachycardia: what is the difference?
Palpitations are a condition in which you feel your own heart beating—too fast, too slow, or irregular. You may feel like your heart is pounding or fluttering. They can be alarming, but do not always reflect serious heart disease.
A rapid heartbeat may have an obvious cause:
- physical activity
- emotional stress
- stopping medication
- caffeine
- nicotine
This type of heartbeat is usually not a cause for concern. However, it is important to distinguish palpitations caused by objective reasons from palpitations that may indicate an underlying heart disease. In everyday life, it is impossible to distinguish between these symptoms; if you feel your heart, it is better to consult a cardiologist. But here a difficulty arises, because symptoms may not appear at the appointment.
I recommend that patients combine an electrocardiogram (ECG) for symptoms of irregular heart rhythm with Holter monitoring. This is a portable device that the patient carries with him for 24 hours. It is connected to your chest with wires and seamlessly records your heart rate. A day later, the patient returns the monitor, and I decipher it. In 99% of cases, combining two studies is enough to determine the cause of rapid heartbeats.
Cardiologist at the Stimul Clinic Grachev Sergey Aleksandrovich
Tachycardia - symptoms and treatment
What to do during an attack
If a person is alone during a sudden attack of tachycardia, it is necessary to breathe deeply and also perform a Valsalva maneuver. To do this, close the glottis and strain the chest muscles for 10-15 seconds (can be compared to trying to push). For younger children, you can try exhaling from a syringe or drinking straw. For the same reaction in infants, you can apply ice packs to the face for a few seconds.
What actions should not be taken?
Without a thorough diagnosis and recommendations of the attending physician, you should not take any medications or dietary supplements. For some arrhythmic tachycardias, which are detected by electrocardiogram data, their use can be dangerous.
Elimination of the underlying disease
Treatment of prolonged tachycardia begins with eliminating the underlying disease of which it is a symptom, or some other causative factors. If the disease is known, then after appropriate treatment the tachycardia also stops.
For pheochromocytoma (adrenal tumor), which produces adrenaline, and sometimes for hyperthyroidism, treatment is surgery, after which one of the symptoms in the form of tachycardia disappears.
For thyroid diseases, treatment is either surgery or drug therapy.
For arterial hypertension, many drugs prescribed for its treatment not only reduce blood pressure, but also affect the heart rate, reducing it. If the use of such drugs is contraindicated, then cardiologists use a drug that acts only on the cells of the sinus node and exclusively slows down the pulse - ivabradine. The drug has a limited number of indications and is prohibited for independent use without consulting a specialist.
In case of anemia, restoration of hemoglobin levels and normalization of heart rate is facilitated by the administration of iron supplements (for iron deficiency anemia), vitamin B12 or folic acid (for B12-deficiency and folate-deficiency anemia), transfusion of blood components (for posthemorrhagic or aplastic anemia), as well as treatment of atrophic gastritis or parasitosis (diphyllobothriasis).
If tachycardia occurs in a healthy person and is associated with low physical development, then the solution is gradual endurance training. It includes increasing the activity of your lifestyle, increasing the complexity of physical training, performing static and dynamic exercises, walking at a moderate and fast pace, running at various distances with increasing difficulty, and swimming.
Treatment of supraventricular tachycardias
In the case of diagnosed supraventricular tachycardia (eg, atrial tachycardia, AVNRT, or atrial flutter), the first step is to assess blood pressure instability by the presence of the following signs:
- hypotension (low blood pressure);
- hypoxia (lack of oxygen in the body);
- dyspnea;
- chest pain;
- shock;
- signs of impaired perfusion (blood passing through the lungs).[2]
Electropulse therapy
If the patient is unstable, then immediate cardioversion is necessary - stimulating the heart with an electrical discharge. In this case, it is important that the defibrillator is in synchronization mode with the QRS complex (the main impulses on the ECG line). This mode allows the defibrillator to prevent shock transmission while the heart is depolarized (otherwise cardioversion could lead to polymorphic ventricular tachycardia).
Initial energy for synchronized cardiac pacing:
- in adults - 100-200 J, can be increased stepwise if there is no success;
- in children - 0.5-1 J/kg, can be increased to 2 J/kg with subsequent attempts.[5]
A patient with stable blood pressure should be prepared for chemical cardioversion - restoration of heart rhythm using drugs. To do this, it is recommended to stimulate the vagus nerve using the Valsalva maneuver and massage of the carotid artery. These methods stimulate the parasympathetic system, slow down the formation of an impulse in the sinus node and more.
For long-term treatment of recurrent supraventricular tachycardia, patients should be counseled on how to self-increase vagal tone.
Valsalva maneuver technique : closing the glottis and tensing the chest muscles for 10-15 seconds (can be compared to trying to push). For younger children, you can try exhaling from a syringe or drinking straw. For the same reaction in infants, you can apply ice packs to the face for a few seconds.
Applying pressure to the eyeballs can also stimulate the parasympathetic system, but this method is not recommended because excessive pressure can cause eye damage.[4][8]
Carotid artery massage technique : the patient lies on his back, neck extended, while using his fingers he presses on one carotid sinus for about 10 seconds. This massage is contraindicated in people with a single artery, patients who have suffered a transient ischemic attack or acute cerebrovascular accident within the last three months, or children or infants.[5]
Drug therapy
If the effect on the vagus nerve has no effect, then adenosine can be used to normalize the heartbeat. It must be administered intravenously. The initial dose is 6 mg (child dose - 0.1 mg/kg). If this dose is ineffective, then 12 mg can be administered (for children - 0.2 mg/kg). A second dose of adenosine (12 mg) may be given one more time if the desired effect is not achieved. Each dose of adenosine should be quickly rinsed with 10–20 ml of saline solution. If the patient is receiving carbamazepine or dipyridamole at the time of treatment, it is recommended to reduce the dose of adenosine to 3 mg.[1][11]
If the rhythm is misinterpreted, administering adenosine may help slow the heart rate for a long time. This will determine whether the tachycardia is caused by another subspecialty complex tachycardia (eg, atrial fibrillation or atrial flutter).
If adenosine is ineffective, you can use:
- diltiazem (0.25 mg/kg intravenously followed by 5-15 mg/hour infusion);
- esmolol (0.5 mg/kg intravenously, then 0.2-0.5 mg/kg per minute - must be repeated with each increase in titer);
- metoprolol (2.5-5 mg intravenously every 2-5 minutes, but not more than 15 mg over 10-15 minutes).
If the above drugs continue to be ineffective, pacing the heart at a rate faster than its own rate may eliminate supraventricular tachycardia. However, there is a risk of ventricular tachycardia or fibrillation and should be used with caution and with immediate availability of cardioversion.[4]
Patients with recurrent supraventricular tachycardia without preexcitation syndrome may require long-term treatment with oral beta-blockers or calcium channel blockers to maintain sinus rhythm. You may also need radiofrequency (catheter) ablation, a surgical treatment for arrhythmia using radiofrequency energy.
Treatment of AV nodal reentrant tachycardia
The primary treatment strategy for AVNRT also involves stimulation of the vagus nerve and administration of adenosine, which stops approximately 80% of arrhythmias. Second-line drugs include non-dihydropyridine calcium channel blockers, beta blockers, or digoxin.[8]
Surgery
If treatment with the above methods is unsuccessful, or medication is not possible due to side effects, then patients may choose catheter ablation as a one-time definitive treatment. This AVNRT treatment method is highly effective (successful in 95% of cases).
Chronic drug therapy using class III or IC antiarrhythmic agents (flecainide, propafenone, amiodarone, dofetilide or sotalol) may be used in cases where the body does not respond to calcium channel blockers or beta blockers, or if the patient refuses catheter ablation . The choice of these antiarrhythmics is usually related to comorbidities and side effect profile.[6][10]
Treatment of tachycardia with folk remedies
The use of traditional medicine often results in the patient not receiving timely, qualified treatment. With tachycardia, this can cause life-threatening complications such as stroke and myocardial infarction.
Causes of rapid heartbeat
Sinus tachycardia - rapid heartbeat without interruptions - is a normal variant. The reasons that trigger it are physiological and emotional stress.
But sometimes it can be associated with a systemic pathological process, for example:
- drop in blood sugar;
- increased body temperature;
- decreased blood pressure;
- adrenal tumor;
- anemia.
Also, sinus tachycardia can be provoked by the use of:
- coffee;
- energy workers;
- strong tea;
- some medications.
Other types of tachycardia are pathological. The main reasons in this case are:
- IHD;
- high blood pressure;
- atherosclerosis of myocardial vessels;
- myocarditis;
- cardiomyopathy;
- heart defects;
- chronic diseases of the bronchi and lungs;
- excess weight;
- sarcaidosis and amyloidosis;
- post-infarction cardiosclerosis;
- dysfunction of the thyroid gland.
How to relieve an attack of tachycardia?
Unbutton your clothing collar, open a window or balcony, inhale deeply and exhale very slowly; breathe like this for 5-10 minutes. Then hold your breath and, as it were, “push” the air into the lower abdomen - this stimulates the vagus nerve, as a result of which the heartbeat will slow down;
Take Corvalol or Valocordin: dissolve 15-20 drops of the drug in half a glass of water at room temperature;
Wash your face with cold water, lie down on a high pillow, place a towel soaked in cold water on your forehead, try to relax;
Close your eyes and simultaneously press on your eyeballs for 2-3 minutes: press for 10 seconds, break for 10 seconds;
Find the right carotid artery (immediately under the jaw, at this point it connects to the cervical artery) and gently, without pressure, massage it. This technique also stimulates the vagus nerve and slows the heart rate.
If the condition does not improve, the heart rate does not decrease, dizziness appears, a feeling of shortness of breath, darkened vision, call an ambulance.
Increased heart rate with blood pressure
High blood pressure
Quite often, tachycardia occurs when blood pressure rises. There is a direct relationship here - the more often the heart contracts, the higher the pressure in the arteries. High blood pressure and rapid heartbeat may have the same causes. Therefore, therapy aimed at stabilizing arterial division also normalizes the heartbeat.
Low pressure
A sharp decrease in pressure can be observed in various shock conditions - traumatic, anaphylactic, infectious-toxic, psychogenic, etc. In this case, the body accelerates the contraction of the heart to increase the pressure. Also, a similar compensatory mechanism is observed with significant blood losses.
Normal pressure
Tachycardia can be observed without pressure fluctuations. With normal indicators, a rapid heartbeat can be associated with anemia, thyroid pathologies, vegetative-vascular dystonia and other diseases. It is impossible to independently determine the cause of increased heart rate, much less self-medicate. If you experience heart palpitations, you should consult a doctor.
What factors affect heart rate?
The most common non-infectious pathology in all countries of the world is diseases of the circulatory system. Based on the results of epidemiological studies dating back to the late 90s of the 20th century, WHO experts came to the conclusion that an increase in heart rate (HR) at rest is one of the risk factors for the development of cardiovascular diseases in healthy people.
According to the national recommendations of the All-Russian Scientific Society of Cardiology, the resting heart rate of a healthy adult should be no more than 80-85 beats per minute and correspond to the pulse rate. The optimal heart rate for an adult at rest is from 60 to 80 beats per minute, while the specific heart rate is individual for each person and depends on a number of factors.
The first is gender. Women have higher normal heart rates than men. This is explained by the specific characteristics of hormonal and emotional backgrounds.
The second is age. In adults, the normal heart rate increases with age: at the age of up to 50 years, the average normal value is 70 beats per minute, at the age of 50-60 years - 74 beats per minute and 79 beats per minute in people over 60 years of age.
In addition, heart rate depends on lifestyle, including physical activity: trained people have a lower heart rate than those leading a sedentary lifestyle. Bad habits also have an impact - smoking, alcohol abuse.
And finally, this indicator correlates with external factors: heart rate increases with lack of sleep, nervous tension, after a heavy meal, increased ambient temperature, etc.
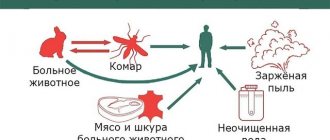
Tachycardia after coronavirus
If observations are made that the coronavirus that causes COVID-19 may also cause a rapid heartbeat called postural orthostatic tachycardia syndrome (POTS). This is a debilitating condition in which your heart speeds up at least 30 beats per minute after you move from a sitting or lying position to a standing position. Moreover, symptoms may not appear immediately, but 10-15 minutes after you get up. In addition to palpitations, you may experience dizziness or even faint.
This syndrome is little known and difficult to diagnose, since it also includes general signs of malaise after an illness:
- fatigue
- exercise intolerance
- gastrointestinal disorders
- headache
- sleep disturbance
At the Stimul clinic, we not only identify this syndrome, but also prescribe competent, effective treatment after examining the body. The therapy has an extremely positive result and leads to complete recovery in a short time.
Respiratory failure as a cause of tachycardia
Decreased function of the respiratory system affects the functioning of the heart. The mechanism of tachycardia is approximately the same as with anemia, because if lung function deteriorates, a lack of oxygen occurs. There are many diseases that lead to respiratory failure, and they all have their own symptoms. Their most common signs, along with rapid heartbeat, are:
- difficulty inhaling or exhaling,
- feeling of suffocation
- the need to strain additional muscles during breathing (abdominal muscles, shoulder girdle),
- sleep and memory disturbances,
- headache,
- cough.
If palpitations are accompanied by such symptoms, you should definitely consult a pulmonologist, and if this is not possible, then consult a therapist.
Diagnosis of heart palpitations
To find out the causes and make a diagnosis, the doctor conducts the following studies:
- interviewing the patient - what provokes tachycardia, how long an attack usually lasts, how often it occurs, what lifestyle the person leads, etc.;
- examination - listening with a stethoscope;
- ECG;
- daily monitoring - special devices are attached to the patient’s body, which during the day record the heart rhythm and changes in its work in familiar living conditions;
- blood tests;
- Ultrasound of the heart.
How to correctly calculate your pulse?
For self-counting, the most common method is palpation (palpation) of the radial artery of the wrist. You need to count your pulse at rest, no earlier than 2 hours after eating, bathing, or massage. The accuracy of the result depends on the correct counting technique.
First, you need to take a watch or stopwatch. Sit down with your hand on a horizontal surface, palm up. Place the index, middle and ring fingers of the opposite hand on the wrist approximately 3 centimeters from the base of the thumb;
When you feel the pulsation, you need to lightly press the artery to the inside of the radius. There is no need to press with force, as the pulse wave may disappear under pressure.
Then you need to count the number of blood pulses within 1 minute. Pulse waves should follow each other at regular intervals; then count the pulse on the second hand.
An increase in heart rate at rest greater than 90 beats per minute is considered tachycardia.
Why is tachycardia dangerous?
Long-term disruption of the heart leads to a disorder of myocardial contractility and right ventricular cardiomyopathy. Insufficient nutrition of the heart muscle can cause coronary heart disease and acute myocardial infarction.
The most dangerous tachycardia is considered to be increased heart rate in the following pathologies:
- ischemia;
- accumulation of fluid in the lungs;
- cardiogenic shock;
- ventricular fibrillation;
- chronic heart failure.
Why should tachycardia be eliminated?
Rapid heartbeat is a rather dangerous symptom that must be eliminated as soon as possible. Due to frequent contractions, the heart does not get enough rest and quickly becomes exhausted. The result is heart failure - a discrepancy between the body's oxygen needs and the work of the heart.
Therefore, if tachycardia occurs, you should consult a doctor. Even in the absence of specific symptoms that would accompany a rapid heartbeat, it is enough to first visit a therapist. After conducting the necessary examinations, he will refer you to the appropriate specialist.
Treatment for palpitations
Treatment for palpitations depends on the underlying cause. If it is physiological, for example, an increase in temperature, you just need to eliminate this factor.
In mild cases, preparations based on mint, valerian, and motherwort help. Sometimes your doctor may prescribe medications to slow your pulse.
If tachycardia is provoked by chronic pathologies, the doctor prescribes medications individually. In this case, treatment may take a long time.
Without concomitant pathologies, tachycardia does not lead to a deterioration in a person’s condition, but can still cause many dangerous complications. If attacks occur against the background of heart pathologies, there is a real risk of their progression. A person who experiences recurring attacks should definitely contact a cardiologist to identify possible disorders.
Rhythm under control
The doctor selects an antiarrhythmic treatment strategy. The main option for normalizing cardiac arrhythmias are antiarrhythmic drugs. Drug therapy is prescribed on a strictly individual basis. It depends on the form of tachycardia, existing chronic diseases and disorders, as well as on the causes that caused this condition! There are different groups of antiarrhythmic drugs depending on the main mechanism of action. Due to individual characteristics in the prescription of therapy, it is strictly forbidden to self-medicate. In difficult cases, urgent medical intervention is necessary to stop the attack.
Additionally, the cardiologist evaluates risk factors that may worsen the patient's condition. This may be family history, old age, arterial hypertension, some chronic diseases, lifestyle, etc. Simple rules for an adequate work and rest regime have a positive effect. This includes proper and restful sleep, good nutrition, limiting stressful situations, and the right approach to physical activity. If you have tachycardia, you should not smoke or drink alcohol. Alcohol and nicotine can independently affect the heart rhythm, and also become provocateurs of more serious pathologies. If palpitations occur, it is very important to always follow all doctor’s orders and regularly come for routine examinations. The specialist will evaluate the effectiveness of the prescribed therapy and clarify your well-being. Do not stop prescribed medications yourself. Only a cardiologist will help you choose the right tactics and take control of your heart rhythm.
The cardiologist at the EXPERT Clinic prescribes individual drug therapy only after a thorough assessment of the patient’s condition. A careful comprehensive approach and correct diagnosis guarantee effective treatment! Frequent heartbeat will no longer bother you.
If you have tachycardia, what should you do?
Many people begin to panic during tachycardia and do not know what to do. At the first symptoms of tachycardia, try to calm down and unfasten your collar to ensure air flow. You can take medicine - tincture of valerian or motherwort helps with tachycardia. There are more effective medications, but they can only be taken as prescribed by a doctor.
In addition, during an attack of tachycardia, washing with ice water or a cold compress on the forehead will help. You should breathe as deeply as possible - this will lower your heart rate.
If attacks recur, you should consult a doctor.
Prevention of tachycardia
Instead of regularly taking tablets for tachycardia, to prevent the disease, you should give up smoking, alcohol, strong black tea and coffee. You should also follow a daily routine - go to bed and wake up according to the schedule. Limiting physical activity will also help get rid of unwanted attacks of tachycardia.
Our cardiology department has modern equipment that will allow you to undergo a full examination and accurately determine the cause of tachycardia.