Home | About us | Delivery | Advertisers | Login | Registration
Delivery on Sundays and holidays does not work!
- Medicines
- dietary supplementsVitamins
- Categories from A to Z
- Brands from A to Z
- Products from A to Z
- Medical equipment
- beauty
- Child
- Care
- Honey products appointments
- Herbs and herbal teas
- Medical nutrition
- Journey
- Making medicinesStock
Pharmacy online is the best pharmacy in Almaty, delivering medicines to Almaty. An online pharmacy or online pharmacy provides the following types of services: delivery of medicines, medicines to your home. Online pharmacy Almaty or online pharmacy Almaty delivers medicines to your home, as well as home delivery of medicines in Almaty.
my basket
Apteka84.kz is an online pharmacy that offers its customers medicines, medicinal and decorative cosmetics, dietary supplements, vitamins, baby food, intimate products for adults, medical equipment and thousands of other medical and cosmetic products at low prices. All data presented on the Apteka84.kz website is for informational purposes only and is not a substitute for professional medical care. Apteka84.kz strongly recommends that you carefully read the instructions for use contained in each package of medicines and other products. If you currently have any symptoms of the disease, you should seek help from a doctor. You should always tell your doctor or pharmacist about all the medicines you take. If you feel you need further help, please consult your local pharmacist or contact our GP online or by telephone.
© 2022 Pharmacy 84.
Tripotassium bismuth dicitrate 120 mg 56 pcs. film-coated tablets
pharmachologic effect
A drug that has a protective effect on the mucous membrane of the stomach and duodenum. Antiulcer drug.
Composition and release form Bismuth tripotassium dicitrate 120 mg 56 pcs. film-coated tablets
Tablets - 1 tablet:
- Active substances: bismuth tripotassium dicitrate - 304.6 mg, which corresponds to the content of bismuth oxide - 120 mg;
- Excipients: corn starch - 71.1 mg, potassium polyacrylate - 23.6 mg, povidone K25 - 17.7 mg, macrogol 6000 - 6 mg, magnesium stearate - 2 mg;
- Film shell composition: hypromellose - 5.5 mg; titanium dioxide - 3 mg; macrogol-4000 - 1.5 mg.
7, 8, 10, 14, 28, 30, 50, 56, 60, 100, 112, 160 or 240 pcs. — cardboard cell packaging or polyethylene terephthalate cans (1, 2, 3, 4, 5, 6, 7, 8, 10, 16) — cardboard packs.
Description of the dosage form
Tablets, film-coated, white or almost white, round, biconvex, odorless or with a weak characteristic odor; two layers are visible on the cross section: a core of white or white with a yellowish tint and a film shell.
Directions for use and doses
Adults and children over 4 years old - orally 2-4 times a day 30 minutes before meals. The dose depends on the patient's age.
The course of treatment is 4-8 weeks. You should not take medications containing bismuth for the next 8 weeks.
To eradicate Helicobacter pylori, it is advisable to use bismuth tripotassium dicitrate in combination with antibacterial drugs that have anti-Helicobacter activity.
Pharmacodynamics
Antiulcer agent with bactericidal activity against Helicobacter pylori. It also has anti-inflammatory and astringent effects. In the acidic environment of the stomach, insoluble bismuth oxychloride and citrate are formed, and chelate compounds are formed with the protein substrate in the form of a protective film on the surface of ulcers and erosions. By increasing the synthesis of prostaglandin E, mucus formation and bicarbonate secretion, it stimulates the activity of cytoprotective mechanisms, increases the resistance of the gastrointestinal mucosa to the effects of pepsin, hydrochloric (hydrochloric) acid, enzymes and bile salts. Leads to the accumulation of epidermal growth factor in the defect area. Reduces the activity of pepsin and pepsinogen.
Pharmacokinetics
Bismuth tripotassium dicitrate is practically not absorbed from the gastrointestinal tract. However, small amounts of bismuth may enter the systemic circulation. It is excreted mainly in feces. A small amount of bismuth entering the plasma is excreted by the kidneys.
Indications for use Bismuth tripotassium dicitrate 120 mg 56 pcs. film-coated tablets
Peptic ulcer of the stomach and duodenum in the acute phase (including those associated with Helicobacter pylori); chronic gastritis and gastroduodenitis in the acute phase (including those associated with Helicobacter pylori); irritable bowel syndrome, which occurs predominantly with symptoms of diarrhea; functional dyspepsia not associated with organic gastrointestinal diseases.
Contraindications
Severe renal dysfunction, pregnancy, lactation, hypersensitivity to bismuth tripotassium dicitrate.
Application of Bismuth tripotassium dicitrate 120 mg 56 pcs. film-coated tablets during pregnancy and breastfeeding
Contraindicated for use during pregnancy and lactation (breastfeeding).
It is used in children over 4 years of age according to the dosage regimen.
special instructions
Should not be used for more than 8 weeks.
During treatment, it is not recommended to exceed the established daily doses for adults and children.
At the end of the course of treatment in recommended doses, the concentration of the active substance in the blood plasma does not exceed 3-58 μg/l, and intoxication is observed only at a concentration of more than 100 μg/l.
During use, stool may turn black due to the formation of bismuth sulfide. Sometimes there is a slight darkening of the tongue.
Side effects of Bismuth tripotassium dicitrate 120 mg 56 pcs. film-coated tablets
From the digestive system: transient effects are possible - nausea, vomiting, increased bowel movements, constipation.
Dermatological reactions: skin rash, itching.
From the side of the central nervous system: with long-term use in high doses - encephalopathy associated with the accumulation of bismuth in the central nervous system.
Drug interactions
If you take other medicines at the same time, as well as food and liquids, in particular antacids, milk, fruit and fruit juices, the effectiveness of bismuth tripotassium dicitrate may change.
Clarithromycin
Clarithromycin, a 14-member macrolide, is a derivative of erythromycin with a similar spectrum of activity and indications for use. However, unlike erythromycin, it is more acid resistant and has a longer half-life. The results of studies showing that the triple eradication therapy regimen for Helicobacter pylori using clarithromycin gives a positive result in 90% of cases, led to the widespread use of the antibiotic.
In this regard, an increase in the prevalence of clarithromycin-resistant strains of H. pylori has been recorded in recent years. There is no evidence that increasing the dose of clarithromycin will overcome the problem of antibiotic resistance to the drug.
One of the significant problems of gastroenterology is cholelithiasis (GSD). This is due to the widespread prevalence of the disease and the steady increase in the number of patients, including those of working age [2]. Despite the existence of conservative methods, the main treatment method for cholelithiasis remains cholecystectomy (CCE) [3, 8]. However, removal of the gallbladder (GB) does not always relieve patients from suffering. From 5 to 40% of patients at various times after surgery experience pain in the upper abdomen and dyspeptic disorders, in the development of which pathology of the esophagogastroduodenal zone (EGDZ) plays an important role [3, 8, 12]. According to Ilchenko A.A. (1998) and Grafova A.A. (2006), diseases of the esophagus, stomach, duodenum (DU) are diagnosed in 11.3–51.9% of patients with cholelithiasis and in 31–84.6% of patients after CCE. At the same time, the structural and functional features of EGDZ in persons without GB are not fully covered in the literature.
A number of studies indicate a decrease in the secretory function of the stomach and duodenogastric reflux (DGR) often developing after surgery, caused by motor-evacuation disorders of the duodenum [11, 12]. Decreased acid production, according to V.N. Sotnikov. et al. (2005), is associated with atrophic changes in the gastric mucosa (GM) and contributes to the occurrence of intestinal metaplasia, polyps and gastric cancer. In this regard, it seems relevant to study not only the morphological features of EGD in individuals without GB, but also the motor-secretory activity of the gastroduodenal complex using 24-hour pH measurements. The advantages of the method include long-term pH recording close to physiological conditions, low invasiveness, good tolerability, and the possibility of an individual approach to therapy [9, 10, 13].
The use of cytoprotectors of different classes, for example bismuth preparations, is promising in the treatment of gastroduodenal pathology. The mechanism of action of bismuth tripotassium dicitrate (BTD) is associated with the precipitation of insoluble bismuth salts (oxychloride and citrate) and the formation of chelate compounds with a protein substrate, creating an insoluble protective coating at the site of the ulcer [7]. VTD increases mucus formation and bicarbonate secretion by accelerating the synthesis of prostaglandin E, reduces the activity of pepsin and pepsinogen, and stimulates the activity of cytoprotective mechanisms [5, 14]. It suppresses the processes of lipid peroxidation while protecting DNA [15]. It is fundamentally important that these effects are realized without interfering with the physiology of the stomach, primarily in the regulation of hydrochloric acid production.
The purpose of the work was to identify the structural and functional features of the EGD and to evaluate the effectiveness of the use of VTD in people with removed GB, taking into account the results of 24-hour pH measurements.
Material and methods
The study was carried out in two stages. At the first stage, to determine the frequency of occurrence of signs of EGD pathology in people with removed GB, 625 people with a history of cholecystectomy were questioned. Of these, 335 (53.6%) people were on outpatient or inpatient treatment, 290 (46.4%) did not contact a gastroenterologist, but voluntarily agreed to take part in the survey.
At the second stage, 94 patients without GB were prospectively examined, who were divided into two groups depending on the time elapsed after cholecystectomy: 43 patients who underwent CCE from 1 to 3 years, 51 - more than 3 years ago. The ratio of women to men among people in the main group was 3.3: 1.0. The average age of patients without GB in the period from 1 to 3 years after CCE was 60.60 ± 2.55 years, in terms of more than 3 years – 60.7 ± 1.97 years. For a more complete picture of the incidence of EGD pathology in people without GB, the study included both patients with gastroenterological complaints (64 people) and without them (30 people). The comparison group consisted of 62 patients with moderate exacerbation of chronic calculous cholecystitis (ratio of women to men - 3.1: 1.0). In the comparison group, the average age of patients was 59.90 ± 1.59 years. The control group included 25 practically healthy individuals.
Exclusion criteria from the study:
- conducting CCE in less than a year;
- “organic” causes of postcholecystectomy disorders (choledochal stricture, elongated cystic duct stump, relapse of choledocholithiasis, etc.);
- age over 70 years;
- acute surgical pathology (acute cholangitis, obstructive jaundice, peritonitis);
- decompensation of chronic somatic diseases;
- tumors of various localizations;
- refusal to participate in the study.
Clinical and instrumental examination was carried out with the voluntary informed consent of the patients. In addition to the standard clinical and laboratory examination, all patients underwent esophagogastroduodenoscopy (EGD) with a targeted biopsy of the mucosa of the lower third of the esophagus, the antrum and body of the stomach, and the duodenal bulb, both in the presence of visible changes in mucus and visually unchanged mucus. For histological examination of biopsy specimens, the generally accepted technique with hematoxylineosin staining was used. Helicobacter pylori was detected using the histobacterioscopic method and rapid urease test (Helpil test system; Association of Medicine and Analytics, St. Petersburg).
Daily pH-metry was performed in 75 patients using the Gastroscan-ECG device (Istok-Sistema, Fryazino). Probes for pH-metry were installed in the lower third of the esophagus, body and antrum of the stomach, the results were processed using a computer. During daily pH-metry, patients were in their usual conditions: they did not limit physical activity, continued to eat as usual; kept a diary where they noted various complaints (heartburn, abdominal pain, etc.). pH 6.0–7.0 was taken as normal acidity values in the esophagus, 1.3–7.4 in the antrum, and 1.5–2.0 in the body of the stomach. Gastroesophageal reflux (GER) was considered to be episodes in which the pH in the esophagus dropped below 4, bile reflux (duodenogastroesophageal reflux - DGER) - episodes of pH rise above 7. DGER was defined as episodes of pH increase in the antrum of the stomach over 7.4. The level of basal secretion of the body of the stomach within the pH range of 1.5–2.0 was regarded as normacidity, pH less than 1.5 – hyperacidity, pH from 2.1 to 6.0 – hypoacidity, over 6.0 – anacidity. The study results were processed statistically using Student's and Mann-Whitney reliability tests.
Results and discussion
At the first stage of the examination, out of 625 patients with a history of CCE, 335 (53.6%) patients who were on outpatient or inpatient treatment, during the questionnaire, noted abdominal pain in the epigastrium of varying severity and symptoms of gastric dyspepsia, characteristic of diseases of the digestive tract, including h. for EGD pathology. Among 290 (46.4%) patients who were not observed by a gastroenterologist, dyspeptic symptoms during targeted questioning were identified in 65 (10.4%) and were absent in 225 (36%). The total number of patients with clinical signs of EGD pathology was 400 (64%).
Analysis of the clinical picture showed that not only the absence of GB is significant, but also the time elapsed after the operation. According to the results of the questionnaire, in people without gallstones in the period 1–3 years after surgery, compared with patients suffering from gallstones, persistent abdominal pain was significantly more common (48.8 and 33.9%, respectively) in the epigastrium (25.6 and 22 .6%) or encircling in the upper abdomen (44.1 and 30.6%). Of the dyspeptic disorders in the early stages after CCE, bitterness in the mouth (65.1%), heartburn (58.1%), lack of appetite (11.6%) were noted more often than with cholelithiasis (54.8; 27.4 and 8 .1% respectively). 3 years or more after CCE, persistent pain (60.8%) in the epigastrium (31.4%) and girdle pain (49%) were detected with greater frequency; nausea (43.1%), bitterness in the mouth (66.7%), belching (39.2%), lack of appetite (17.7%). The results obtained indicate that CCE, while relieving patients from attacks of biliary colic and from the gallbladder itself, does not lead to complete recovery and does not always improve the condition of the EGD organs. Some dyspeptic symptoms and persistent epigastric pain occur in people without gallbladder more often than before surgery, especially more than 3 years after CCE.
At the second stage, patients with and without gastroenterological complaints were included in the study. During endoscopic examination, EGD lesions were detected in 95.3% of patients without GB with pain and dyspeptic syndromes and in 81.4% of patients in the absence of clinical manifestations of the disease. Obviously, the absence of clinical symptoms does not always mean the absence of morphofunctional changes in the EGDZ. The asymptomatic course of gastroduodenal pathology in some patients creates the illusion of well-being and complicates timely diagnosis and treatment.
According to the results of the study, catarrhal esophagitis in persons without gallstones was more common (8.1%) than in those with gallstones; the frequency of its detection was similar at different times after cholecystectomy (9.3 and 9.8%). Erosion of the esophagus was not detected in any of the examined patients.
The greatest frequency and diversity were changes in the coolant, mainly in the antrum, diagnosed in 90.7% in the early and 96% in the long term after cholecystectomy. Structural features of the gastric mucosa in patients without gallbladder at various times after cholecystectomy are presented in Fig. 1 and 2. In the period from 1 to 3 years after CCE, superficial gastritis (20.9%), refluxgastritis (13.9%), acute erosions of the coolant (6.9%), and DGR ( 34%), chronic duodenitis and papillitis (18.6 and 11.6%). 3 years or more after cholecystectomy, the incidence of reflux gastritis (21.6%), focal and multifocal atrophic gastritis (13.7 and 5.9%), DGR (35.3%), chronic duodenitis and papillitis increased (21 .6 and 17.6% respectively). The incidence of erosive and ulcerative defects and cicatricial deformation of the pylorus and duodenal bulb was similar in the main groups and the comparison group.
In a morphological study of biopsy specimens of the esophagus, the incidence of moderately severe leukocyte infiltration at different times after CCE was similar and amounted to 9.3 and 9.8%. However, more than 3 years after CCE, signs of dystrophy (5.9%), atrophy (3.9%) of the epithelium and columnar metaplasia (3.9%) were revealed. Such changes are characteristic of a long course of esophagitis and may be associated with the aggressive effect of bile acids and pepsin as a result of DGER. Morphological changes in the coolant in patients at various times after CCE are presented in Fig. 3. In patients who underwent CCE from 1 to 3 years ago, compared with patients suffering from cholelithiasis, the following were more often detected: gastritis with damage to the glands without atrophy (30.5%), regenerative hyperplasia of the integumentary epithelium (47.3%), dysplasia I–II degrees (4.65%) and intestinal metaplasia of the gastric mucosa (11.6%). As the time elapsed after CCE increased to 3 years or more, glandular atrophy (9.8%), intestinal metaplasia (17.6%) and grades I–II dysplasia of the gastric epithelium (7.8%) were significantly more common.
Histological changes in the duodenal mucosa 1–3 years after surgery corresponded to moderate atrophy in 25.3% of cases, lymphocytic infiltration in 9.1%. 3 or more years after surgery, subatrophic duodenitis was found in 25.5%, lymphocytic infiltration was more common (15.7%), signs of gastric metaplasia were detected (3.9%).
The contamination of the coolant with N. pylori in patients without gallstones was significantly lower compared to patients with gallstones: 1–3 years after CCE - 20.2%, over 3 years - 18.9%, with gallstones - 35.3%. The data obtained correspond to published information indicating the inhibitory effect of bile acids of duodenal reflux on H. pylori [6]. In addition, due to partial or complete atrophy of the glands, mucus production decreases, which can limit the “habitat” of the microorganism [6, 12].
According to the results of 24-hour pH-metry, “acid” and “alkaline” reflux in the esophagus were 2.5 times more common than endoscopic and morphological signs of esophagitis (Table 1). It was found that with an increase in the period elapsed after CCE, the incidence of DGR, DGER increased, and the frequency of GER decreased. In the long-term period after CCE, hyperacidity was recorded significantly less often, and hypo- and anacidity were recorded more often. At the same time, the appearance of acute and chronic erosions of the gastric mucosa in persons without gallbladder in 65% of cases occurred with normal or reduced production of hydrochloric acid, and exacerbation of duodenal ulcer in 71.4% occurred against the background of normal acid production. It is obvious that in persons without gallbladder, hydrochloric acid as a factor of aggression does not have a dominant role in the development of destructive changes in the mucous membrane of the EGD.
. Results of daily pH-metry at different times after CCE.
Statistical processing of the data revealed a correlation between a decrease in acid production and superficial gastritis 1–3 years after surgery (r = 0.321), at a later date - with the severity of atrophic changes in the coolant (r = 0.727), and the presence of intestinal metaplasia (r = 0.713) .
Thus, in the absence of GB, with increasing time after surgery, progression of motor and secretory dysfunction is noted, and atrophic and dysregenerative changes in the mucous membrane of the EGD are aggravated.
Helicobacteriosis and a violation of the relationship between the factors of aggression and defense are traditionally considered to be leading in the etiopathogenesis of gastroduodenal pathology. There is no doubt about the dominant role of hydrochloric acid in damage to the EGDZ CO. In this regard, the main drugs in the treatment of EGD diseases are proton pump inhibitors and antibiotics.
However, judging by the results of our own research, in people without GB, other mechanisms predominate in the development of gastroduodenal pathology. Due to the loss of the concentration function of the gallbladder, the development of DGR and DGER becomes more frequent, and prematurely deconjugated bile acids become the main factor damaging the mucosa of the esophagus and stomach. In addition, the prevalence of H. pylori decreases, atrophic changes in the coolant progress with a decrease in acid production.
Taking this into account, it is advisable to include VTD drugs that have cytoprotective properties and do not reduce the production of hydrochloric acid in the treatment regimen for gastroduodenal pathology [5, 7]. Bismuth preparations suppress the processes of lipid peroxidation while simultaneously protecting DNA from damage. Studies have appeared indicating the ability of bismuth ions to stimulate the reverse development of gastric epithelial atrophy due to a proliferative effect [14, 15].
In our study, when determining indications for differentiated prescription of drugs, we used an approach based on the results of 24-hour pH measurements, endoscopic and morphological studies. When acid production decreased (14 patients), patients were prescribed VTD at a dose of 480 mg/day. The comparison group consisted of 14 patients receiving omeprazole at a dose of 40 mg/day. The course of taking the drugs was 8 weeks.
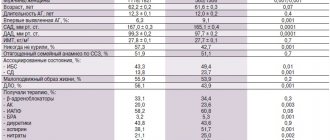
The results of dynamic observation proved the clinical effectiveness of VTD in this cohort of patients. The criterion for the effectiveness of therapy was the positive dynamics of the following parameters (Table 2).
. Clinical signs of gastroduodenal pathology in patients without gallstones during VTD therapy.
After 10–14 days of treatment, patients taking VTD were less likely to report constant epigastric pain, belching, heartburn, and their appetite improved. It is known that this drug has cytoprotective and anti-Helicobacter effects [7], which may explain such a regression of clinical symptoms.
8 weeks after treatment, patients underwent fibrogastroduodenoscopy with targeted biopsy of the esophagus, stomach and duodenum. The dynamics of the endoscopic and morphological picture of the EGD pathology are presented in Table. 3 and 4.
When taking VTD, the incidence of erosive and ulcerative defects of the gastric mucosa, superficial gastritis, H. pylori contamination and the degree of leukocyte infiltration of the gastric mucosa significantly decreased. It is known that bismuth salts are able to form a protective coating at the site of an ulcer, increase the formation of mucus and the secretion of bicarbonates, reduce the activity of pepsin, impair the adhesion of H. pylori, destroy the bacterial wall and inhibit H. pylori enzymes [5, 7]. Atrophic changes, the phenomena of metaplasia and dysplasia did not undergo reverse development, but did not progress.
Thus, the pathogenetic direction of action and the proven effectiveness of VTD justify the need for its use in the pathology of EGD in the absence of GB.
conclusions
With an increase in the time elapsed after removal of the gallbladder, the incidence of GDR and DGER in patients significantly increases, the secretory activity of the gastric mucosa decreases, atrophy of the gastroduodenal zone, intestinal metaplasia and dysplasia of the gastric epithelium of degrees I–II increases.
In some patients without GB, the pathology of EGD is asymptomatic, which creates the illusion of well-being. However, when conducting a comprehensive instrumental examination of patients in this group, structural and functional changes in the esophagus, stomach and duodenum are revealed, requiring drug correction.
Patients who have undergone CCE should be in a group of dispensary observation and targeted therapeutic intervention. The examination plan for patients without gallbladder should include endoscopy with targeted biopsy, as well as daily pH measurements. The use of 24-hour pH-metry in patients of this group makes it possible to effectively diagnose reflux pathology of endoscopy and gastric secretory activity, as well as to carry out individual selection of medications.
If a decrease in acid production is detected, in the presence of erosive and ulcerative defects and/or H. pylori is detected, VTD may be the drug of choice. Therapy carried out by VTD helps to reduce abdominal pain, dyspeptic syndrome, and reduce the activity of the inflammatory process.
Information about the authors: Elena Vyacheslavovna Graushkina – candidate of medical sciences, assistant at the department of therapy of pediatric and dental faculties of Saratov State Medical University named after. IN AND. Razumovsky; Kozlova Irina Vadimovna – Doctor of Medical Sciences, Professor, Head of the Department of Therapy of Pediatric and Dental Faculties of Saratov State Medical University named after. IN AND. Razumovsky. Email: [email protected] ; Volkov Stanislav Vladimirovich – Candidate of Medical Sciences, Assistant of the Department of Therapy, Pediatric and Dental Faculties, Saratov State Medical University named after. IN AND. Razumovsky, Head of the Gastroenterology Department of City Clinical Hospital No. 5 of Saratov
Proton pump inhibitors (PPIs)
PPI therapy has proven effective in various clinical studies. Although PPIs have a direct antibacterial effect on H. pylori in vitro, they do not play an important role in eradicating the infection.
The mechanism by which PPIs synergize when combined with antimicrobials to enhance the clinical efficacy of eradication therapy has not been fully established. It is assumed that antisecretory drugs of the PPI group may help increase the concentration of antimicrobial agents, in particular metronidazole and clarithromycin, in the gastric lumen. PPIs reduce the volume of gastric juice, as a result of which the leaching of antibiotics from the surface of the mucosa decreases, and the concentration, accordingly, increases. In addition, reducing the volume of hydrochloric acid maintains the stability of antimicrobials.
Eradication therapy
Despite the use of combination treatment regimens, 10–20% of patients infected with H. pylori fail to achieve elimination of the pathogen. The best strategy is to select the most effective treatment regimen, but the possibility of using two or even more sequential regimens should not be ruled out if the treatment of choice is insufficiently effective.
If the first attempt at eradication of H. pylori fails, it is recommended to immediately proceed to second-line therapy. Antibiotic sensitivity testing and switching to salvage therapy regimens are indicated only for those patients in whom second-line therapy will also not lead to eradication of the pathogen.
One of the most effective “rescue regimens” is a combination of PPI, rifabutin and amoxicillin (or levofloxacin 500 mg) for 7 days. An Italian study led by Fabrizio Perri and published in Alimentary Pharmacology & Therapeutics in 2000 confirmed that the rifabutin regimen was effective against strains of H. pylori resistant to clarithromycin or metronidazole. However, the high price of rifabutin limits its widespread use.
NB! To avoid the development of resistance to both metronidazole and clarithromycin, these drugs are never combined in the same regimen. The effectiveness of such a combination is very high, but patients who do not respond to therapy usually develop resistance to both drugs at once (a study by German scientists led by Ulrich Peitz, published in Alimentary Pharmacology & Therapeutics in 2002). And further selection of therapy causes serious difficulties.
Research data confirm that a 10-day salvage therapy regimen, including rabeprazole, amoxicillin and levofloxacin, is much more effective than standard second-line eradication therapy (a study by Italian scientists led by Enrico C Nista, published in Alimentary Pharmacology & Therapeutics in 2003 year).
Indications for eradication therapy
According to the Maastricht 2-2000 Consensus Report, H. pylori eradication is strongly recommended:
- all patients with peptic ulcer disease;
- patients with poorly differentiated MALT lymphoma;
- persons with atrophic gastritis;
- after resection for gastric cancer;
- first-degree relatives of patients with stomach cancer.
The need for eradication therapy in patients with functional dyspepsia, GERD, as well as in persons taking non-steroidal anti-inflammatory drugs for a long time remains a subject of debate. There is no evidence that eradication of H. pylori in such patients affects the course of the disease. However, it is well known that individuals with H. pylori who have nonulcer dyspepsia and corpus-predominant gastritis are at increased risk of developing gastric adenocarcinoma. Thus, H. pylori eradication should also be recommended for patients with nonulcer dyspepsia, especially if histology reveals corpus-predominant gastritis.
The argument against anti-Helicobacter therapy in patients taking NSAIDs is that the body protects the gastric mucosa from the damaging effects of drugs by increasing cyclooxygenase activity and prostaglandin synthesis, while PPIs reduce natural defenses. However, eradication of H. pylori before prescribing NSAIDs significantly reduces the risk of peptic ulcer disease during subsequent treatment (a study by American scientists led by Francis K. Chan, published in The Lancet in 1997).
Metronidazole
H. pylori is generally very sensitive to metronidazole, the effectiveness of which is independent of pH. After oral or infusion use, high concentrations of the drug are achieved in the gastric juice, which makes it possible to achieve the maximum therapeutic effect. Metronidazole is a prodrug that undergoes activation by bacterial nitroreductase during metabolism. Metronidazole causes H. pylori to lose its helical DNA structure, causing DNA damage and killing the bacterium.
NB!
The result of treatment is considered positive if the results of the test for H. pylori, carried out no earlier than 4 weeks after the course of treatment, are negative. Performing the test before 4 weeks after eradication therapy significantly increases the risk of false negative results. It is preferable to stop taking PPIs two weeks before diagnosis. Helicobacter pylori eradication therapy: scheme