Pharmacodynamics and pharmacokinetics
Pharmacodynamics
Antiarrhythmic drug. It has a membrane-stabilizing effect, sodium channel blocker properties and slight b-adrenergic blocking activity.
It inhibits the increase in action potential, which reduces the speed of impulse transmission. The refractory period in the AV node, atrium, and ventricles increases. It also lengthens the refractory period in additional conduction pathways in individuals with Wolff-Parkinson-White syndrome.
Pharmacokinetics
The drug is a mixture of S-propafenone and R-propafenone.
The highest concentration in the blood is created 2-3 hours after administration. The active substance undergoes significant biotransformation under the influence of the CYP2D6 isoenzyme . Bioavailability depends on the dose and form of release. Quickly distributed in tissues. In almost 90% of patients, the drug undergoes rapid and significant transformation, with a half-life of 3-9 hours. There are 2 main derivatives - 5-hydroxypropafenone and N-depropylpropafenone .
In another 10% of patients, the drug is metabolized more slowly. With this type of metabolism , the half-life averages 12-30 hours.
Rytmonorm®
Propafenone is a racemic mixture consisting of R-propafenone and S-propafenone.
Suction
The maximum concentration (Cmax) of the drug in the blood plasma is created in the interval from 2 to 3 hours after oral administration. Propafenone undergoes significant and saturable presystemic biotransformation using the CYP2D6 isoenzyme (first pass effect through the liver), and therefore the absolute bioavailability of the drug depends on the dose and dosage form. Although food intake caused an increase in bioavailability and plasma Cmax in a single dose study, chronic administration of propafenone with food in healthy volunteers did not result in a significant change in bioavailability.
Distribution
Propafenone is rapidly distributed in the body. The volume of distribution at steady state ranges from 1.9 to 3.0 l/kg. The degree of binding of propafenone to plasma proteins depends on the concentration and decreases from 97.3% when a dose of 0.25 ng/ml is administered to 91.3% when a dose of 100 ng/ml is administered.
Metabolism and excretion
There are two genetically determined pathways for the metabolism of propafenone. In more than 90% of patients, the drug is quickly and significantly metabolized, the half-life (T1/2) ranges from 2 to 10 hours (so-called “rapid metabolizers”). In such patients, propafenone is metabolized to form 2 active metabolites - 5-hydroxypropafenone via the CYP2D6 isoenzyme and N-depropylpropafenone (norpropafenone) via the CYP3A4 and CYP1A2 isoenzymes. In less than 10% of patients, propafenone is metabolized more slowly because 5-hydroxypropafenone is not formed or is formed in small quantities (so-called “poor metabolizers”). With this type of metabolism, T1/2 ranges from 10 to 32 hours. The clearance of propafenone ranges from 0.67 to 0.81 l/h/kg.
Since the equilibrium state of pharmacokinetic parameters or indicators is achieved 3-4 days after taking the drug in all patients, the dosage regimens of propafenone are the same for all patients, regardless of metabolic rate (“fast” or “slow” metabolizers).
With significant metabolism with a cycle of saturable hydroxylation using the CYP2D6 isoenzyme, the pharmacokinetics of propafenone are non-linear, and with slow metabolism - linear.
The pharmacokinetics of propafenone has significant individual variability, which is mainly due to the effect of “first pass” through the liver, as well as the nonlinearity of pharmacokinetics with significant metabolism. The variability of propafenone blood concentrations requires careful titration of the dose and monitoring of clinical and electrocardiographic signs of drug action.
Elderly patients
In elderly patients with normal renal function, the content of propafenone varied greatly and did not differ significantly from that in healthy young patients. The content of 5-hydroxypropafenone was approximately similar, but the content of propafenone glucuronides was twice as high.
Renal dysfunction
In patients with impaired renal function, the content of propafenone and 5-hydroxypropafenone was similar compared to healthy volunteers, but accumulation of glucuronide metabolites was observed. If renal function is impaired, propafenone should be used with caution.
Liver dysfunction
Bioavailability and T1/2 when taken orally are increased in patients with impaired liver function. It is necessary to adjust the dose of propafenone in case of liver dysfunction.
Contraindications
- Brugada syndrome.
- Myocardial infarction (within 3 months).
- Severe changes in the myocardium (severe bradycardia, chronic refractory heart failure with LVEF up to 35%, sinus node weakness, cardiogenic shock, AV block, intraatrial conduction disorders, distal block, arterial hypotension.
- Severe changes in water and electrolyte balance.
- Decompensated obstructive chronic pulmonary disease.
- Concomitant use of Ritonavir .
- Myasthenia gravis.
- Age less than 18 years.
- Hypersensitivity to the components of the drug.
It is recommended to use Ritmonrm with caution in cases of atrial fibrillation , organic myocardial changes, obstructive lesions of the respiratory tract, liver or kidney dysfunction, in persons with a pacemaker, elderly patients, during pregnancy or lactation .
Side effects
- Hematopoietic disorders: leukopenia, thrombocytopenia, agranulocytosis, granulocytopenia.
- Immune disorders : blood dyscrasia, cholestasis , skin rash.
- Metabolic disorders: decreased appetite .
- Mental disorders: nightmares, anxiety, confusion, sleep disturbances.
- Nervous disorders: headache , dizziness , taste disturbance, fainting, paresthesia , lack of coordination, extrapyramidal symptoms , convulsions, anxiety.
- Visual disturbances: blurred vision.
- Hearing disorders: vertigo.
- Circulatory disorders: cardiac conduction disorders, tachycardia , palpitations, bradycardia, atrial flutter, arrhythmia, ventricular tachycardia, marked decrease in pressure, heart failure, ventricular fibrillation, decreased number of heartbeats, orthostatic hypotension.
- Respiratory disorders: shortness .
- Digestive disorders: vomiting, abdominal pain, nausea, constipation , diarrhea , dry mouth, flatulence , bloating, retching, diseases of the digestive system, liver dysfunction, cholestasis, hepatocellular disorders, jaundice, hepatitis.
- Skin disorders: skin itching , urticaria, erythema , skin rash.
- Musculoskeletal disorders: lupus-like syndrome.
- Reproductive disorders: decreased sperm count, erectile dysfunction.
- General disorders: weakness, chest pain, fever , increased fatigue.
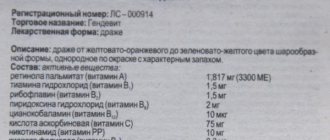
Indications for use
- arrhythmias due to a decrease in potassium and magnesium in the blood plasma;
- arrhythmias that occurred when taking cardiac glycosides;
- extrasystolic arrhythmia;
- cardiac ischemia;
- cardiopsychoneurosis;
- myocarditis and myocardiopathy ;
- liver diseases;
- chronic fatigue syndrome (as part of complex therapy).
Instructions for use Ritmonorm (Method and dosage)
The instructions for Ritmonorm prescribe taking the tablets orally, swallowing them whole (due to the bitter taste), washing them down with liquid and without chewing.
The dosage of the drug must be selected individually, based on the patient’s response and the effect obtained. It is recommended to begin therapy in a hospital, having first stopped taking all antiarrhythmic drugs (monitoring blood pressure and ECG ).
In individuals with significantly increased QRS intervals and AV block, it is recommended to reduce the dose.
For adults weighing over 70 kg, the initial dosage is 150 mg three times a day. The dosage can be increased after 3-4 days to 300 mg twice a day, and if necessary - to a maximum dosage of 300 mg three times a day.
If the patient weighs up to 70 kg, therapy should begin with low dosages of the drug. The dosage should not be increased if the duration of use of the drug does not exceed 3-4 days.
Information for physicians on the use of propafenone in the treatment of cardiac arrhythmias
doctor to work with the patient
Information for patients
Among the many modern antiarrhythmic drugs, propafenone deserves special attention. Propafenone (Propanorm) is one of the most effective and safe drugs used to treat supraventricular and ventricular heart rhythm disorders.
Propafenone in the treatment of atrial fibrillation.
Propafenone is the drug of choice for the relief of AF paroxysms in patients with preserved left ventricular systolic function (Class of recommendations I, level of evidence A). The pharmacodynamics of propafenone allows the drug to be prescribed in tablet form as a loading dose of 450-600 mg and used on an outpatient basis independently by the patient. The first loading dose of propafenone should be taken under the supervision of the attending physician, after which the use of propafenone on an outpatient basis can be recommended to relieve paroxysms of AF.
Diagnostic examination of patients with persistent AF before starting propafenone therapy should include a thorough collection of complaints and medical history, an objective examination of the patient and an electrocardiographic study (ECG) or 24-hour Holter ECG monitoring. It is mandatory to perform a control ECG to assess the dynamics of the duration of the PQ and QT intervals after the first dose of the drug.
With long-term use of propafenone, the following treatment regimens are used to prevent relapses of AF:
- The drug should be started with a minimum daily dose of 150 mg of propafenone 3 times a day,
- if relapses of arrhythmia occur, the dose may be increased to 300 mg of propafenone 2 times a day,
- in patients with excess body weight or with frequent long-term paroxysms of AF, the maximum daily dose can reach 900 mg, in which case it is advisable to prescribe 300 mg of propafenone 3 times a day.
The safety of antiarrhythmic therapy is one of the most important indicators of successful treatment of recurrent AF. These studies on the effectiveness of an oral loading dose of propafenone did not find dangerous side effects. When compared with other IC class antiarrhythmic drugs, propafenone has a larger evidence base and has a better safety profile.
Favorable factors for long-term use of propafenone can be considered its low organotoxicity compared to other antiarrhythmic drugs. The half-life of propafenone is on average 10 hours, the drug does not accumulate in tissues and is well tolerated by patients. The duration of use of propafenone has no restrictions; prospective observation of patients receiving propafenone therapy did not reveal the occurrence of severe side effects. Given the short half-life and lack of cumulative properties, the drug can be prescribed for a long time, without interruption.
Propafenone in the treatment of paroxysmal supraventricular tachycardia.
The use of a loading dose of propafenone 450 mg can be successfully used to relieve paroxysms of supraventricular tachycardia. Prophylactic administration of propafenone at a dose of 150 mg 3 times a day can be prescribed to patients with frequent symptomatic or rare but hemodynamically significant episodes of paroxysmal supraventricular tachycardia.
Propafenone in the treatment of ventricular extrasystole.
Propafenone is an effective drug for the treatment of PVCs in patients without significant organic heart pathology. The daily dose of propafenone for the treatment of PVCs is 450 mg; the drug can be taken in short courses lasting 4-8 weeks with breaks.
Absolute contraindications for the prescription of propafenone are dysfunction of the sinoatrial or atrioventricular node, bundle branch block, prolongation of the QT interval, Brugada syndrome, gross organic pathology of the heart, decompensated CHF. Considering the presence of a beta-blocking effect of the drug, chronic obstructive pulmonary diseases may be relative contraindications for its use.
Draw your attention to! This article is not a call for self-medication. It is written and published to improve the reader's knowledge about his own health and understanding of the treatment regimen prescribed by the doctor. If you experience similar symptoms, be sure to seek help from a doctor. Remember: self-medication can harm you.
Overdose
Signs of overdose: deterioration of sinus node automaticity, increased PQ interval, increased QRS complex, ventricular fibrillation, ventricular tachycardia, AV block, ventricular flutter, headache, blurred vision, dizziness, tremor, paresthesia, nausea, constipation, dry mouth mucous membranes, arrest breathing, coma .
Treatment of overdose
Hemodialysis is ineffective. In addition to carrying out standard emergency measures, it is necessary to monitor and adjust the main indicators in the intensive care unit. of Isoproterenol and Dopamine are effective . Seizures are usually treated with intravenous diazepam . You may also need to be connected to a ventilator and perform chest compressions.
Interaction
When used simultaneously with local anesthetics or other drugs that slow down the pulse or reduce myocardial contractility, increased side effects are possible.
Concomitant use with drugs metabolized by CYP2D6 may cause an increase in the concentration of these drugs in the blood .
An increase in the content of Metoprolol, Propranolol, Desipramine, Theophylline, Cyclosporine, Digoxin in the blood can be observed when taken together with Propafenone.
Drugs that inhibit the isoenzymes CYP1A2, CYP2D6, CYP3A4 may cause an increase in the concentration of Propafenone in the blood. When using Propafenone with blockers of these isoenzymes, patients should be monitored, and if necessary, the dose of the drug should be adjusted.
Combined treatment with Amiodarone and Propafenone can cause repolarization and conduction disturbances and be accompanied by a proarrhythmogenic effect. In this case, it may be necessary to adjust the dosages of both drugs.
The simultaneous use of Propafenone and Rifampicin reduces the concentration of the former in the blood and weakens its antiarrhythmic activity.
It is necessary to monitor the parameters of the coagulation system in patients simultaneously receiving indirect anticoagulants , since Propafenone stimulates the pharmacological action of this group of drugs and increases the prothrombin time.
With the simultaneous use of Propafenone and selective serotonin reuptake blockers, an increase in the concentration of the former in the blood is possible.
Rhythmonorm
Antiarrhythmic drug.
Propafenone has membrane-stabilizing properties, sodium channel blocker properties (class IC) and weak beta-blocking activity (class II).
It slows down the rise of the action potential, as a result of which the speed of impulse conduction decreases (negative dromotropic effect). The refractory period in the atrium, AV node and ventricles lengthens. Propafenone also prolongs the refractory period in accessory pathways in patients with Wolff-Parkinson-White (WPW) syndrome.
Pharmacokinetics
Propafenone is a racemic mixture consisting of R-propafenone and S-propafenone.
Suction
Cmax of the drug in blood plasma is created in the interval from 2 to 3 hours after oral administration. Propafenone undergoes significant and saturable presystemic biotransformation using the CYP2D6 isoenzyme (first pass effect through the liver), and therefore the absolute bioavailability of the drug depends on the dose and dosage form. Although food intake caused an increase in bioavailability and plasma Cmax in a single dose study, chronic administration of propafenone with food in healthy volunteers did not result in a significant change in bioavailability.
Distribution
Propafenone is rapidly distributed in the body. Vd at equilibrium ranges from 1.9 to 3.0 l/kg. The degree of binding of propafenone to plasma proteins depends on the concentration and decreases from 97.3% when administered at a dose of 0.25 ng/ml to 91.3% when administered at a dose of 100 ng/ml.
Metabolism and excretion
There are two genetically determined pathways for the metabolism of propafenone. In more than 90% of patients, the drug is quickly and significantly metabolized, T1/2 ranges from 2 to 10 hours (so-called “fast metabolizers”). In such patients, propafenone is metabolized to form 2 active metabolites - 5-hydroxypropafenone via the CYP2D6 isoenzyme and N-depropylpropafenone (norpropafenone) via the CYP3A4 and CYP1A2 isoenzymes.
In less than 10% of patients, propafenone is metabolized more slowly because 5-hydroxypropafenone is not formed or is formed in small quantities (so-called “poor metabolizers”). With this type of metabolism, T1/2 ranges from 10 to 32 hours. Propafenone clearance ranges from 0.67 to 0.81 l/h/kg.
Since the equilibrium state of pharmacokinetic parameters or indicators is achieved 3-4 days after taking the drug in all patients, the dosage regimens of propafenone are the same for all patients, regardless of metabolic rate (“fast” or “slow” metabolizers).
With significant metabolism with a cycle of saturable hydroxylation using the CYP2D6 isoenzyme, the pharmacokinetics of propafenone are non-linear, and with slow metabolism - linear.
Pharmacokinetics in special clinical situations
The pharmacokinetics of propafenone has significant individual variability, which is mainly due to the effect of “first pass” through the liver, as well as the nonlinearity of pharmacokinetics with significant metabolism. Variability in blood concentrations of propafenone requires careful titration of the dose and monitoring of clinical and electrocardiographic signs of drug action.
In elderly patients with normal renal function, the content of propafenone varied greatly and did not differ significantly from that in healthy young patients. The content of 5-hydroxypropafenone was approximately similar, but the content of propafenone glucuronides was 2 times higher.
In patients with impaired renal function, the content of propafenone and 5-hydroxypropafenone was similar compared to healthy volunteers, but accumulation of glucuronide metabolites was observed. If renal function is impaired, propafenone should be used with caution.
Bioavailability and T1/2 when taken orally are increased in patients with impaired liver function. It is necessary to adjust the dose of propafenone in case of liver dysfunction.
special instructions
Therapy should be started in a hospital setting, since there is a possibility of arrhythmogenic effects caused by the use of Ritmonorm. It is necessary that previous antiarrhythmic treatment be completed before starting new therapy within a period equal to approximately 2-4 half-lives of the drugs used. Each patient must undergo an ECG and a general clinical examination before starting therapy.
Taking propafenone can reveal the hidden course of Brugada syndrome and provoke Brugada-like changes during an ECG . After starting treatment with Ritmonorm, it is recommended to perform an ECG to exclude Brugada syndrome.
In patients with pronounced changes in the myocardium when using the drug Ritmonorm, the occurrence of serious side effects cannot be ruled out.
Dizziness, blurred vision, increased fatigue and arterial hypotension disrupt the patient’s reaction speed and impair his ability to drive. During treatment with Rytmonorm you should refrain from such activities.
Reviews about Rhythmocore
A decrease in the level of potassium in the blood causes the development of extrasystole and tachycardia . Therefore, maintaining potassium at normal levels is important for normal cardiac function. Hypokalemia increases the toxicity of cardiac glycosides and causes an imbalance in protein balance in the body.
A decrease in magnesium levels is observed in half of patients who take diuretics and, especially often, in the elderly. Hypomagnesemia also manifests itself as heart rhythm disturbances. Correction of disorders is carried out by prescribing potassium and magnesium drugs, among which are Panangin , Rhythmocor and Asparkam . They are usually well tolerated, especially since the dosage form in capsule form significantly reduces the incidence of adverse reactions from the gastrointestinal tract . Patients note effectiveness, reasonable price, and only in some cases the development of undesirable effects.
- “... An attack of arrhythmia begins suddenly and can last more than a week. After 2 days of taking Rhythmocor everything goes away.”
- “... There was a rhythm disturbance and pain like angina pectoris. I drank it for 10 days - everything returned to normal, including the cardiogram.”
- “... Helps with extrasystole.”
- “... Itching and rash appeared on the fifth day of use.”
- “... After it I felt heaviness in the liver and stomach.”
Price, where to buy
The price of Ritmonorm in standard packaging in Russia is 700-1350 rubles; in Ukraine, purchasing such a drug will cost an average of 511 hryvnia.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
ZdravCity
- Ritmonorm tablets p.p.o.
150 mg 50 pcs. Famar Lyon 482 rub. order
Pharmacy Dialogue
- Ritmonorm (tab. p.pl/vol. 150 mg No. 50) EbbVi
510 rub. order
show more