Telsartan® H
Telmisartan
Other antihypertensive drugs
The antihypertensive effect may be enhanced. In addition, orthostatic hypotension may be exacerbated by the use of alcohol, barbiturates, narcotics, or antidepressants.
Baclofen, amifostine
Based on the pharmacological properties of baclofen and amifostine, it can be assumed that they will enhance the therapeutic effect of all antihypertensive drugs, including telmisartan.
Ramipril
In one study, with the combined use of telmisartan and ramipril, an increase in AUC0-24 and Cmax of ramipril and ramiprilat was observed by 2.5 times. The clinical significance of this interaction has not been established.
In the analysis of adverse events leading to discontinuation of treatment and the analysis of serious adverse events obtained during the clinical trial, it was found that cough and angioedema were observed more often during therapy with ramipril, while arterial hypotension occurred more often during therapy with telmisartan. Cases of hyperkalemia, renal failure, arterial hypotension and syncope were observed significantly more often with the combined use of telmisartan and ramipril.
Lithium preparations
There was a reversible increase in the concentration of lithium in the blood, accompanied by toxic effects when taking ACE inhibitors. In rare cases, such changes have been reported with the administration of angiotensin II receptor antagonists, in particular telmisartan. When prescribing lithium drugs and angiotensin II receptor antagonists simultaneously, it is recommended to determine the lithium content in the blood.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
NSAIDs, including acetylsalicylic acid in doses used as an anti-inflammatory agent, cyclooxygenase-2 (COX-2) inhibitors and non-selective NSAIDs, can cause the development of acute renal failure in patients with reduced blood volume. Drugs that affect the RAAS may have a synergistic effect. In patients receiving NSAIDs and telmisartan, blood volume should be compensated and renal function monitored at the beginning of treatment.
A decrease in the effect of antihypertensive agents, such as telmisartan, through inhibition of the vasodilatory effect of prostaglandins has been observed when used together with NSAIDs. When telmisartan was taken simultaneously with ibuprofen or paracetamol, no clinically significant effect was detected.
Drugs that can cause hyperkalemia
Like other drugs acting on the RAAS, telmisartan may pose a risk of developing hyperkalemia. The risk may be increased when used concomitantly with other medicinal products that may cause hyperkalemia - salt substitutes containing potassium; potassium-sparing diuretics (spironolactone, eplerenone, triamterene or amiloride); ACE inhibitors; APA II; NSAIDs, including selective COX-2 inhibitors), heparin, immunosuppressants (cyclosporine or tacrolimus) and trimethoprim. Caution should be exercised and plasma potassium levels periodically monitored during coadministration.
Warfarin, glibenclamide, simvastatin and amlodipine
No clinically significant interaction was identified.
Digoxin
There was an increase in the average concentration of digoxin in the blood plasma by an average of 20% (in one case by 49%). When telmisartan and digoxin are prescribed simultaneously, it is advisable to periodically determine the concentration of digoxin in the blood.
Diuretics (thiazide or loop)
Previous treatment with high doses of diuretics such as furosemide (loop diuretic), hydrochlorothiazide (thiazide diuretic) may lead to hypovolemia and the risk of developing arterial hypotension at the beginning of treatment with telmisartan.
Aliskiren, aliskiren-containing drugs
Clinical data have shown that dual blockade of the RAAS through concomitant use with ACE inhibitors, angiotensin II receptor antagonists or aliskiren is associated with a high incidence of side effects such as arterial hypotension, hyperkalemia, decreased renal function (including acute renal failure) compared with using one active RAAS blocker.
Concomitant use of telmisartan with aliskiren is contraindicated in patients with diabetes mellitus or renal failure (GFR less than 60 ml/min/1.73 m2 body surface area) and is not recommended in other patients.
The simultaneous use of telmisartan and ACE inhibitors is contraindicated in patients with diabetic nephropathy.
Glucocorticosteroids (for systemic use)
Glucocorticosteroids weaken the antihypertensive effect of telmisartan.
Hydrochlorothiazide
Not recommended drug combinations
Lithium preparations
With the simultaneous use of hydrochlorothiazide and lithium preparations, the renal clearance of lithium is reduced, which can lead to an increase in the concentration of lithium in the blood plasma and an increase in its toxicity. If concomitant use of hydrochlorothiazide is necessary, the dose of lithium preparations should be carefully selected, the concentration of lithium in the blood plasma should be regularly monitored and the dose of the drug should be adjusted accordingly.
Combinations of drugs requiring special attention
Drugs that can cause polymorphic ventricular tachycardia of the “pirouette” type
Hydrochlorothiazide should be used with extreme caution concomitantly with drugs such as:
- class IA antiarrhythmic drugs (quinidine, hydroquinidine, disopyramide, procainamide);
- class III antiarrhythmic drugs (dofetilide, ibutilide, bretylium tosylate), sotalol, dronedarone, amiodarone;
- other (non-antiarrhythmic) medicines, such as:
- neuroleptics: phenothiazines (chlorpromazine, cyamemazine, levomepromazine, thioridazine, trifluoperazine, fluphenazine), benzamides (amisulpride, sultopride, sulpride, tiapride), butyrophenones (droperidol, haloperidol), pimozide, sertindole;
- antidepressants: tricyclic antidepressants, selective serotonin reuptake inhibitors (citalopram, escitalopram):
- antibacterial agents: fluoroquinolones (levofloxacin, moxifloxacin, sparfloxacin, ciprofloxacin); macrolides (erythromycin for intravenous administration, azithromycin, clarithromycin, roxithromycin, spiramycin), co-trimoxazole;
- antifungals: azoles (voriconazole, itraconazole, ketoconazole, fluconazole);
- antimalarials (quinine, chloroquine, mefloquine, halofantrine, lumefantrine);
- antiprotozoal drugs (pentamidine for parenteral administration);
- antianginal agents (ranolazine, bepridil);
- antitumor agents (vandetanib, arsenic trioxide, oxaliplatin, tacrolimus);
- antiemetics (domperidone, ondansetron);
- drugs affecting gastrointestinal motility (cisapride);
- antihistamines (astemizole, terfenadine, mizolastine);
- other medicines (anagrelide, vasopressin, difemanil methyl sulfate, ketanserin, probucol, propofol, sevoflurane, terlipressin, terodiline, flecainide, cilostazol)
due to an increased risk of ventricular arrhythmias, especially polymorphic ventricular tachycardia of the “pirouette” type (risk factor - hypokalemia). It is necessary to determine the potassium content in the blood plasma and. if necessary, adjust it before starting combination therapy with hydrochlorothiazide with the above drugs. It is necessary to monitor the patient’s clinical condition, blood plasma electrolyte levels and ECG parameters. In patients with hypokalemia, it is necessary to use drugs that do not cause polymorphic ventricular tachycardia of the “pirouette” type.
Medicines that can prolong the QT interval
The simultaneous use of hydrochlorothiazide with drugs that can prolong the QT interval should be based on a careful assessment for each patient of the relationship between the expected benefit and the potential risk (possible increased risk of developing torsade de pointes (TdP).
When using such combinations, it is necessary to regularly record an ECG (to detect prolongation of the QT interval), as well as monitor the potassium level in the blood.
Drugs that can cause hypokalemia: Amphotericin B (with intravenous administration), gluco- and mineralocorticosteroids (with systemic use), tetracosactide (ACTH), glycyrrhizic acid (carbenoxolone, drugs containing licorice root), laxatives that stimulate intestinal motility
Increased risk of hypokalemia when used simultaneously with hydrochlorothiazide (additive effect). Regular monitoring of potassium levels in the blood plasma is necessary and, if necessary, its correction. During therapy with hydrochlorothiazide, it is recommended to use laxatives that do not stimulate intestinal motility. With the simultaneous use of hydrochlorothiazide and cardiac glycosides, the concentration of potassium in the blood plasma, ECG readings should be regularly monitored and, if necessary, therapy should be adjusted.
It is recommended to stop taking hydrochlorothiazide 2-3 days before starting therapy with angiogensin-converting enzyme (ACE) inhibitors to prevent the development of symptomatic hypotension.
If this is not possible, then the initial dose of ACE inhibitors should be reduced.
Ethanol, barbiturates, antipsychotics (neuroleptics), antidepressants, anxiolytics, narcotic analgesics and general anesthesia
It is possible to enhance the antihypertensive effect of hydrochlorothiazide and potentiate orthostatic hypotension (additive effect).
Theophylline
Theophylline enhances the effect of diuretics.
Non-depolarizing muscle relaxants (eg, tubocurarine)
The effect of non-depolarizing muscle relaxants may be enhanced.
Adrenergic agonists (pressor amines)
Hydrochlorothiazide may reduce the effect of adrenergic agonists such as epinephrine (adrenaline) and norepinephrine (norepinephrine).
Nonsteroidal anti-inflammatory drugs (NSAIDs), including selective cyclooxygenase-2 (COX-2) inhibitors and high doses of acetylsalicylic acid (≥3 g/day)
NSAIDs may reduce the diuretic and antihypertensive effects of hydrochlorothiazide. With simultaneous use, there is a risk of developing acute renal failure due to a decrease in glomerular filtration rate. Hydrochlorothiazide may enhance the toxic effects of high doses of salicylates on the central nervous system.
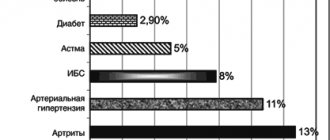
Oral hypoglycemic agents and insulin
Thiazide diuretics affect glucose tolerance (hyperglycemia may develop) and reduce the effectiveness of hypoglycemic agents (dose adjustment of hypoglycemic agents may be required). Hydrochlorothiazide and metformin should be used together with caution due to the risk of lactic acidosis due to renal impairment caused by hydrochlorothiazide.
Beta blockers, diazoxide
Concomitant use of thiazide diuretics (including hydrochlorothiazide), beta-blockers or diazoxide may increase the risk of hyperglycemia.
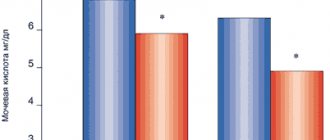
Medicines used to treat gout (probenecid, sulfinpyrazone, allopurinol)
Dose adjustment of uricosuric drugs may be required as hydrochlorothiazide increases serum uric acid concentrations. Thiazide diuretics may increase the incidence of hypersensitivity reactions to allopurinol.
Amantadine
Thiazide diuretics (including hydrochlorothiazide) may reduce the clearance of amantadine, lead to increased plasma concentrations of amantadine and increase the risk of adverse effects.
Fluconazole
With repeated simultaneous use with hydrochlorothiazide, the maximum concentration of fluconazole in blood plasma increases by 40%. No dose adjustment of fluconazole is required, but this interaction should be taken into account.
Anticholinergic drugs (cholinergic blockers)
Anticholinergic drugs (eg, atropine, biperiden) increase the bioavailability of thiazide diuretics by reducing gastrointestinal motility and the rate of gastric emptying.
Cytotoxic (antitumor) drugs
Thiazide diuretics reduce the renal excretion of cytotoxic drugs (for example, cyclophosphamide and methotrexate) and potentiate their myelosuppressive effects.
Methyldopa
Cases of hemolytic anemia have been described with the simultaneous use of hydrochlorothiazide and methyldopa.
Carbamazepine
Risk of developing symptomatic hyponatremia. When using hydrochlorothiazide and carbamazepine simultaneously, it is necessary to monitor the patient's condition and monitor the sodium content in the blood plasma.
Cyclosporine
With simultaneous use of thiazide diuretics and cyclosporine, the risk of developing hyperuricemia and exacerbation of gout increases.
Oral anticoagulants
Thiazide diuretics may reduce the effect of oral anticoagulants.
Iodinated contrast agents
Dehydration while taking thiazide diuretics increases the risk of developing acute renal failure, especially when using high doses of iodinated contrast agents. Before using iodinated contrast agents, it is necessary to compensate for fluid loss.
Calcium preparations
With simultaneous use, it is possible to increase the calcium level in the blood and develop hypercalcemia due to a decrease in the excretion of calcium ions by the kidneys. If simultaneous administration of calcium-containing drugs is necessary, the calcium level in the blood plasma should be monitored and the dose of calcium supplements should be adjusted.
Anion exchange resins (cholestyramine and colestipol)
Anion exchange resins reduce the absorption of hydrochlorothiazide. Single doses of cholestyramine and colestipol reduce the absorption of hydrochlorothiazide in the gastrointestinal tract by 85% and 43%, respectively.
Periodic monitoring of the potassium level in the blood plasma is recommended in cases where a drug containing hydrochlorothiazide and telmisartan is prescribed together with drugs that can cause hypokalemia, as well as with drugs that can increase the potassium level in the blood serum.
Telsartan N, 28 pcs., 12.5 mg+80 mg, tablets
Side effects reported with the combination of telmisartan and hydrochlorothiazide
The overall incidence of adverse events reported with the combination of telmisartan and hydrochlorothiazide was comparable to the incidence of adverse effects observed with telmisartan monotherapy in controlled trials involving 1471 patients randomized to telmisartan + hydrochlorothiazide (835 patients) or patients treated with telmisartan plus hydrochlorothiazide. who received only telmisartan (636). The dependence of side effects on the dose, gender, age or race of patients has not been established.
All side effects that occur when using the combination of telmisartan and hydrochlorothiazide with a frequency exceeding the frequency of placebo (p≤0.05) are presented below according to system-organ classes.
Frequency of occurrence: very common (≥1/10); often (≥1/100 - <1/10); uncommon (≥1/1000 - <1/100); rare (≥1/10000 - <1/1000); very rare (<1/10000); frequency unknown (cannot be determined from available data). Adverse reactions are presented in descending order of severity.
Infectious and parasitic diseases:
rarely - bronchitis, pharyngitis, sinusitis.
From the immune system:
rarely - exacerbation or intensification of symptoms of systemic lupus erythematosus (based on post-marketing experience).
Metabolism and nutrition:
uncommon - hypokalemia; rarely - hyperuricemia, hyponatremia.
Mental disorders:
infrequently - anxiety; rarely - depression.
From the nervous system:
often - dizziness; uncommon - syncope/fainting, paresthesia; rarely - insomnia, sleep disturbances.
From the side of the organ of vision:
rarely - visual impairment, transient blurred vision.
Hearing and labyrinth disorders:
infrequently - vertigo.
From the heart:
infrequently - tachycardia, arrhythmia.
From the side of blood vessels:
infrequently - hypotension, orthostatic hypotension.
From the respiratory system, chest and mediastinal organs:
infrequently - shortness of breath; rarely - respiratory distress syndrome (including pneumonia and non-cardiogenic pulmonary edema).
From the gastrointestinal tract:
infrequently - diarrhea, dry mouth, flatulence; rarely - abdominal pain, constipation, dyspepsia, vomiting, gastritis.
From the liver and biliary tract:
rarely - liver dysfunction (see
Description of selected adverse reactions
).
For the skin and subcutaneous tissues:
rarely - angioedema (including cases with fatal outcome), erythema, itching, rash, increased sweating, urticaria.
From the musculoskeletal system and connective tissue:
uncommon - back pain, muscle spasms, myalgia; rarely - arthralgia, muscle cramps, pain in the calf muscles.
From the genital organs and breast:
infrequently - erectile dysfunction.
General disorders and disorders at the injection site:
uncommon - chest pain; rarely - flu-like syndrome, pain.
Laboratory and instrumental data:
infrequently - increased concentration of uric acid in the blood plasma; rarely - increased concentration of creatinine in the blood plasma, increased activity of CPK in the blood plasma, increased activity of liver enzymes.
Additional information on experience with individual active ingredients
Adverse reactions previously observed with each component of the drug may potentially be observed with the combination of telmisartan and hydrochlorothiazide, even if they were not observed when studying this combination.
Hydrochlorothiazide
The use of hydrochlorothiazide may lead to or worsen hypovolemia, which can cause electrolyte imbalance. The following are the adverse reactions noted when using hydrochlorothiazide in monotherapy. The frequency of occurrence of such reactions cannot be determined.
Infectious and parasitic diseases:
sialadenitis.
From the blood and lymphatic system:
aplastic anemia, hemolytic anemia, bone marrow dysfunction, leukopenia, neutropenia, agranulocytosis, thrombocytopenia.
From the immune system:
anaphylactic reactions, hypersensitivity.
From the endocrine system:
uncontrolled diabetes mellitus.
Metabolism and nutrition:
anorexia, loss of appetite, electrolyte imbalance, hypercholesterolemia, hyperglycemia, hypovolemia.
Mental disorders:
restlessness.
From the nervous system:
slight dizziness.
From the side of the organ of vision:
xanthopsia, acute myopia, acute angle-closure glaucoma.
From the side of blood vessels:
necrotizing vasculitis.
From the gastrointestinal tract:
pancreatitis, feeling of discomfort in the stomach.
From the liver and biliary tract:
hepatic jaundice, cholestatic jaundice.
For the skin and subcutaneous tissues:
lupus-like syndrome, photosensitivity reactions, cutaneous vasculitis, toxic epidermal necrolysis.
From the musculoskeletal system and connective tissue:
weakness.
From the kidneys and urinary tract:
interstitial nephritis, renal dysfunction, glucosuria.
General disorders and disorders at the injection site:
pyrexia.
Laboratory and instrumental data:
increased triglyceride levels.
Telmisartan
The incidence of side effects with telmisartan is similar to that with placebo.
In placebo-controlled studies, the overall incidence of side effects observed with telmisartan (41.4%) was generally comparable to the incidence of side effects observed with placebo (43.9%). The side effects listed below are based on the results of all clinical studies involving patients treated with telmisartan for hypertension, or the results of the use of telmisartan in patients 50 years of age and older with a high risk of developing cardiovascular events.
Infectious and parasitic diseases:
uncommon - upper respiratory tract infections, urinary tract infections, incl. cystitis; rarely - sepsis, including fatal cases.
From the blood and lymphatic system:
infrequently - anemia; rarely - eosinophilia, thrombocytopenia.
From the immune system:
rarely - hypersensitivity reactions, anaphylactic reactions.
Metabolism and nutrition:
uncommon - hyperkalemia; rarely - hyperglycemia (in patients with diabetes mellitus).
From the heart:
infrequently - bradycardia.
From the nervous system:
rarely - drowsiness.
From the respiratory system, chest and mediastinal organs:
infrequently - cough;
very often - interstitial lung disease (see Description of selected adverse reactions
).
From the gastrointestinal tract:
rarely - a feeling of discomfort in the stomach.
For the skin and subcutaneous tissues:
rarely - eczema, drug and toxic rash.
From the musculoskeletal system and connective tissue:
rarely - arthrosis, tendon pain.
From the kidneys and urinary tract:
uncommon - renal dysfunction (including acute renal failure).
General disorders and disorders at the injection site:
infrequently - asthenia.
Laboratory and instrumental data:
rarely - decrease in Hb level.
Description of selected adverse reactions
Liver dysfunction.
Most cases of liver dysfunction with post-registration use of telmisartan have been described in patients in Japan. Apparently, these undesirable effects are more typical for this group of patients.
Sepsis.
In the
PRoFESS
, an increased incidence of sepsis was observed with telmisartan compared with placebo. The data obtained can be considered a random find, because the mechanism of the relationship is unknown.
Interstitial lung disease.
Cases of interstitial lung disease were recorded during post-registration use of telmisartan and coincided with the period of its prescription. However, a cause-and-effect relationship between these events has not been established.