The protein component does not have its own color and dissolves in blood serum. Fibrinogen is the basis of blood clots; it is formed in the liver; its renewal is recorded every 3 days. The amount of the element is regularly checked by laboratory diagnostics. A critical minimum or maximum amount of a component can cause serious disruptions in the functioning of the body, provoke long-term bleeding or the formation of blood clots on the inner walls of blood vessels.
The role of fibrinogen in the body
Fibrinogen activation occurs when blood vessels are damaged. This begins the process of formation of a blood clot, in which platelets take an active part. These cells stick together, forming a so-called red blood clot. Thrombin-activated fibrinogen is then transformed into fibrin strands, which strengthen the primary blood clot, thereby forming a white thrombus.
In addition to stopping bleeding, fibrinogen takes part in the following processes in the human body:
- restoration of damaged soft tissues: skin, mucous membranes, muscles, etc.;
- dissolution of the blood clot during tissue regeneration - fibrinolysis;
- formation and development of new blood vessels - angiogenesis;
- strengthening the walls of blood vessels, counteracting inflammatory changes in them.
D-dimer as a marker of thrombus formation after Covid
“Often in patients both in the acute period and after suffering a new coronavirus infection, an increase in D-dimer may be observed in blood tests. D-dimer is the breakdown product of fibrin, a small protein fragment present in the blood after the blood clot has broken down. If the D-dimer is normal, this practically excludes thrombosis, and if it is elevated, thrombosis or other causes are possible. Therefore, the decision to prescribe or continue anticoagulants after treatment for coronavirus should not be made solely on the basis of this indicator. We need to assess the patient's complaints and his general status: if, along with an increase in D-dimer, there are also symptoms indicating thrombosis, additional studies are necessary (for example, CT angiography of the pulmonary artery to exclude pulmonary embolism, duplex scanning of the veins of the lower extremities to exclude thrombosis of the veins of the lower extremities).
Kogrusheva Yulia Petrovna
expert
clinic "Ogni Olympa" therapist, gastroenetrologist
Materials and methods
The retrospective study included an analysis of medical records of 350 patients with SARS-CoV-2 infection confirmed by PCR data who were treated at City Clinical Hospital No. 52, Moscow.
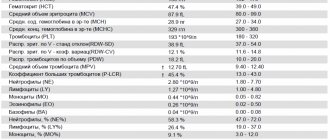
The average age of patients was 63 years (from 20 to 95 years). Women were present in equal proportions to men (176/174 people). At the time of admission, 53 patients (15.1%) had a severe condition, and 297 (84.9%) had a moderate condition. The average score on the NEWS scale was 3 points (from 1 to 12). 49 patients died (14%), 301 patients were discharged from the hospital. During treatment, all patients underwent laboratory monitoring of a series of parameters at intervals of 1–2 days, including, among other things, assessment of fibrinogen according to Claus, D-dimer, prothrombin time (ACL-TOP 500 automatic hemostasis analyzer); liver transaminases and C-reactive protein (automated biochemical analyzer Beckman Coulter Au-680), as well as platelet count (automatic hematology analyzer Beckman Coulter DXH-800). When hypofibrinogenemia was detected less than 2.0 g/l, patients underwent thromboelastography (TEG) using a TEG 5000 thromboelastograph and thromboelastometry (TEM) using a ROTEM delta thromboelastometer.
All patients received initial therapy with hydroxyquinine and azithromycin. Interleukin-6 receptor antagonists were included in the treatment complex for 132 patients (37.7%). From the moment of admission, all patients received prophylaxis of venous thromboembolic complications with low molecular weight heparins (enoxaparin, nadroparin and dalteparin), according to current recommendations [3].
As part of the analysis, it was necessary to evaluate:
1) dynamics of plasma fibrinogen in patients with COVID-19;
2) the risk of developing thrombosis with hyperfibrinogenemia (over 5.0 g/l) and hemorrhagic manifestations with hypofibrinogenemia (less than 2.0 g/l);
3) different values of plasma fibrinogen as a predictor of unfavorable outcome of the disease.
To solve the problems, a statistical analysis was performed using BioStat Pro 5.9.8 software and the Excel statistical package. Analysis of variance, assessment of linear correlation and odds were carried out. Data are presented as mean ± standard deviation, median (minimum, maximum).
Congenital disorders of fibrinogen synthesis
Rare congenital diseases affecting the synthesis process and functionality of fibrinogen are:
- Dysfibrinogenemia. It is manifested by reduced production of this protein by liver cells due to a genetic mutation of the F1 gene located on the q28 region of chromosome 4. With this pathology, the liver produces abnormal dysfunctional fibrinogen, which is difficult to degrade when converted into fibrin or cannot function normally in the coagulation cascade. Dysfibrinogenemia increases the risk of blood clots or, in rare cases, causes bleeding and poor wound healing².
- Congenital hypofibrinogenemia. Leads to a decrease in fibrinogen production in the liver. People with this condition may experience spontaneous bleeding (such as from the nose or gums)³.
- Congenital afibrinogenemia. Pathology accompanied by acute lack of fibrinogen. Episodes of heavy bleeding occur, especially in infancy or early childhood: from the umbilical cord, nose, after surgical procedures. Large hematomas (bruises) appear even with minor bruises.
Figure 1. Blood coagulation diagram. Image: rob3000/Depositphotos
Solution
Deviation from the norm of fibrinogen does not allow us to draw conclusions about a hidden disease. The indicators make it possible to identify increased or decreased results, but not to detect the original source of the disease. To make a correct diagnosis, the patient must undergo additional laboratory diagnostic examination. Correct identification of existing pathologies will solve the problem.
Doctors warn that ignoring the altered level of fibrinogen and refusing to undergo therapeutic procedures provokes external and internal bleeding (with reduced results) or accelerated formation of blood clots (with an increased amount).
The attending physician makes the final diagnosis and selects a treatment regimen. By seeking professional help in a timely manner, the chances of complications and consequences are significantly reduced.
Blood test for fibrinogen
Measuring the level of fibrinogen in blood plasma is most often performed as part of a coagulogram, a blood test that evaluates blood clotting functions. Venous blood is used for the study. In the analysis form, fibrinogen is often indicated by its full name in Latin or Cyrillic. The amount of this protein varies in grams per liter of blood plasma (g/l).
In the vast majority of cases, fibrinogen levels are measured as part of a coagulogram, a comprehensive study that evaluates the various stages of blood clotting. In addition to this analysis, the coagulogram also includes: free protein S, factor VIII, protein C, plasminogen, lupus anticoagulant, antithrombin III, D-dimer, prothrombin, thrombin time, APTT (activated partial thromboplastin time), INR (international normalized ratio).
In general, there are two options for laboratory blood tests for fibrinogen³:
- Fibrinogen activity test. Evaluates the part of the coagulation process in which soluble fibrinogen is converted into fibrin filaments. It measures the time it takes for a fibrin clot to form after adding a standard amount of thrombin to a blood sample (plasma). The time it takes for a clot to form directly correlates with the amount of active fibrinogen. An increase in the interval for clot formation may be due to decreased levels of normal fibrinogen or because it is not functioning properly.
- Fibrinogen antigen test. Measures the level of functional and dysfunctional fibrinogen in the blood. In most cases, it is used as a follow-up test to determine whether the decrease in fibrinogen activity is due to insufficient fibrinogen or a malfunction of fibrinogen.
What is the difference between fibrinogen, D-dimer, and fibrin breakdown products (FDP) tests?
Determination of fibrinogen activity allows one to evaluate the conversion of fibrinogen to fibrin. Fibrinogen antigen testing measures the amount of factor I dissolved in the blood before it is converted to insoluble fibrin and forms a fibrin network. D-dimer and FDP tests help assess the state of the fibrinolytic system, the body's ability to break down blood clots when they are no longer needed. FDP is a measurement of all fragments of a dissolving clot, while D-dimer is a more specific measurement for one of the final fragments of decomposition.
Coagulogram
Factors of the coagulation, anticoagulant (anticoagulant) and fibrinolytic blood systems take part in the hemostasis system. A change in the functional state of one of the systems is accompanied by compensatory changes in the activity of the other. Violation of functional relationships can lead to severe pathological conditions of the body, consisting of either increased bleeding or intravascular thrombus formation. The study of the hemostatic system has the following goals:
- diagnosis of disorders in the hemostasis system;
- clarification of the admissibility of surgical intervention in case of identified disorders in the hemostasis system;
- monitoring treatment with direct and indirect anticoagulants, as well as thrombolytic therapy.
Currently, the usual practice for recognizing hemostasis disorders is heterogeneous and often varies in different clinics from performing one or two uninformative tests (prothrombin index, fibrinogen) to using an overloaded list of methods, some of which duplicate each other.
Many routine tests are outdated, of little value and inaccurate. To date, assessment of the results of prothrombin time using the prothrombin index is incomparable with global methodological approaches. Conditions for taking a coagulogram
Eating food, including juice, tea, coffee, and alcohol, is not allowed for 8 hours (preferably 12) before the test. You can drink plain water. If your doctor has prescribed a test while you are taking medications that affect blood clotting, please note this when taking the test.
List of coagulogram tests:
- Lupus anticoagulant;
- D-dimer;
- Antithrombin II;
- Thrombin time;
- APTT;
- INR (PTV, PTI);
- Fibrinogen;
- Screening for antiphospholipid syndrome.
Lupus Anticoagulant
Lupus Anticoagulant is an inhibitor of the blood anticoagulant system. Being present in the blood, it increases the coagulation activity of the hemostasis system, which adversely affects the process of implantation of the embryo, the course of the entire pregnancy, and the development of the fetus.
D-dimer (fibrin degradation product, D-dimer, Fibrin degradation fragment)
Determination of D-dimer level is a highly specific and sensitive marker of thrombus formation. However, its level also increases in pathological conditions accompanied by increased fibrinolysis: hemorrhagic complications, infections, wound healing, in the presence of rheumatoid factor in the blood, etc. However, the determination of D-dimer has important diagnostic value in the diagnosis of thrombosis. Its normal level allows, with 98% accuracy, to exclude conditions accompanied by increased thrombus formation.
Antithrombin III
AT III is determined by thrombin inhibition. AT III deficiency can be hereditary or acquired. The most common clinical manifestation of hereditary AT III deficiency is the development of deep vein thrombosis and, as a consequence, pulmonary embolism. The likelihood of developing thrombotic complications in patients with AT III deficiency increases with age.
Acquired AT III deficiency may be due to decreased synthesis, increased protein intake, or loss of protein. In all these cases, there is a parallel decrease in the concentration and activity of AT III. AT III is synthesized in the liver, so some liver diseases lead to decreased AT III levels. If, in parallel with the decrease in AT III, there is an increase in the thrombogenic properties of the vascular wall and activation of coagulation, then a further decrease in AT III is observed due to its consumption, which occurs in DIC caused by various pathologies: massive injuries, sepsis, inflammation of wounds, snake bites, complicated pregnancy, cancer, etc.
In addition, a decrease in AT III synthesis is observed during therapy with estrogens and synthetic drugs with estrogenic effects, nephrotic syndrome and gastrointestinal diseases, when the loss of protein exceeds the rate of its synthesis. In these cases, a parallel decrease in AT III and albumin is observed.
Thrombin time (TV)
Gives a general assessment of the final stage of blood coagulation. This is an indicator of the transition of fibrinogen to fibrin, the state of the anticoagulant system. Does not depend on the internal and external activation system, but depends on the concentration of fibrinogen, the presence of abnormal fibrinogen, the activity of antithrombins, the processes of polymerization and stabilization of fibrin.
In the clinic, TV determination is used to monitor heparin therapy (especially high molecular weight heparin) and fibrinolytic therapy; for the diagnosis of activation of fibrinolysis, indirect diagnosis of hypo- and dysfibrinogenemia.
Clinical and diagnostic value
TV shortening:
- hyperfibrinogenemia (more than 6 g/l);
TV extension:
- severe hypofibrinogenemia (less than 1.0 g/l), dysfibrinogenemia;
- heparin therapy with regular heparin (the test detects relatively low concentrations of the anticoagulant - from 0.05 IU/ml of blood);
- the presence of fibrin polymerization inhibitors (PDF, paraproteins, etc.);
- increase in immunoglobulins;
- use of asparaginase, streptokinase, urokinase;
- a decrease in fibrinase activity (factor XIII) does not affect thrombin time.
Activated partial thromboplastin time (APTT)
APTT evaluates the intrinsic pathway of activation of the coagulation process. The test is also called kaolin-kephalin time. It is a simple and comprehensive test, sensitive to deficiencies of all coagulation factors. But it is mainly used to evaluate factors VIII, IX, XI, XII and prekallikrein. Sensitive to excess plasma anticoagulants. Does not depend on platelet count.
This test is one of the main tests for monitoring heparin treatment. In patients receiving heparin therapy, the aPTT lengthens by 1.5–2 times, which indicates the effectiveness of treatment.
Determining the APTT allows you to finally resolve the issue of tolerance to heparin: for this purpose, the APTT is determined 1 hour before the next administration of heparin. If the APTT is prolonged by more than 2.5 times compared to the norm, an increased sensitivity to heparin is noted, its dose is reduced or the interval between injections is increased.
Clinical and diagnostic value
of test extension:
- hypocoagulation and bleeding tendency;
- hemophilia (A, B, C);
- significant deficiency of factors II, V, X, XII, fibrinogen;
- von Willebrand disease;
- heparin therapy with unfractionated heparin (the test detects low concentrations of the anticoagulant - from 0.05 IU/ml of blood);
- treatment with indirect anticoagulants;
- the presence of blood clotting inhibitors (PDF, lupus anticoagulant).
A shortened test indicates hypercoagulability and a tendency to thrombus formation;
and is also observed during normal pregnancy and taking oral contraceptives. Prothrombin (thromboplastin) time (PT)
By means of PT with calculation of the international normalized ratio (INR) and prothrombin index (PI), the external mechanism is assessed in total. Prothrombin time depends on the content of prothrombin itself - factor II, as well as factors V, VII, X and fibrinogen. Used to diagnose thromboembolic and hemorrhagic conditions, to monitor treatment with indirect anticoagulants.
Clinical and diagnostic value
Prolongation of prothrombin time (PI decreases, INR increases) - a tendency to hypocoagulation. Main reasons:
- violation of protein-synthetic function of the liver;
- vitamin K deficiency (usually due to impaired breakdown and absorption of fats in the intestines);
- treatment with indirect anticoagulants;
- deficiency of factors II, V, VII, X;
- heparin therapy with regular heparin (the test responds to relatively high concentrations of the anticoagulant - from 0.5 IU/ml of blood);
- hypo-, dysfibrinogenemia, impaired fibrin polymerization;
- the presence of clotting factor inhibitors (PDF, lupus anticoagulant);
- medications: anabolic steroids, antibiotics, acetylsalicylic acid in large doses, laxatives, methotrexate, nicotinic acid, thiazide diuretics, etc.
Shortening of prothrombin time is rare and has no independent diagnostic value. Together with a shortening of APTT, it indicates a tendency towards hypercoagulation:
- thrombosis;
- increased activity of factor VII (trauma, necrosis);
- pregnancy, childbirth;
- medications: acetylsalicylic acid in small doses, oral contraceptives, corticosteroids, vitamin K, barbiturates, antihistamines, caffeine.
Currently, recording the results of prothrombin time using the prothrombin index does not meet modern requirements.
To unambiguously interpret the results of prothrombin time measurements, regardless of the laboratory, INR is used: this method allows you to mathematically correct the difference given by thromboplastins with different sensitivities. Calculated using thromboplastin standardized to the international sensitivity index. Determination of fibrinogen content
Its concentration is determined by the time of clot formation in diluted platelet-free plasma with the addition of excess highly active thrombin (according to Clauss). Fibrinogen is synthesized in the liver, from where it enters the blood. Changes in fibrinogen concentration are observed in various diseases - primarily in disorders of the hemostasis system and acute inflammation.
An increase in the amount of fibrinogen, even within normal values, is considered a risk factor for cardiovascular diseases.
Clinical and diagnostic value
Increased concentration (tendency to hypercoagulation):
- physiological (pregnancy, menstruation);
- mild forms of hepatitis;
- kidney disease;
- acute phase reactions, myocardial infarction;
- collagenoses;
- radiation sickness;
- malignant tumors (especially lung cancer);
- estrogens, oral contraceptives.
Decreased concentration (a decrease below 0.5–1 g/l causes bleeding):
- congenital afibrinogenemia, hypo- and dysfibrinogenemia;
- severe liver damage;
- condition after bleeding, injury, burn;
- bone marrow lesions (leukemia, tumor metastases);
- activation of fibrinolysis (including drugs);
- phenobarbital, anabolic steroids, unfractionated heparin in high doses.
In DIC syndrome, changes in coagulogram tests depend on the form and stage of the process.
Antiphospholipid syndrome (APL)
This is a group of diseases caused by the presence of antibodies to phospholipids. Antiphospholipid antibodies (APL) are autoantibodies of the IgG and IgM class, capable of binding to the antigenic determinants of phospholipids (cardiolipin, phosphatidylserine, phosphatidylinositol, phosphatidylic acid, phosphatidylcholine) and phospholipid binding proteins. Binding with cardiolipin occurs with the obligatory participation of a cofactor, rg-glycoprotein I.
The reasons for the production of APL have not been established. Presumably, long-term persistence of viruses that are tropic to the vascular endothelium causes: morphological and functional changes in endothelial membrane cells with the development of hypercoagulation syndrome, stimulation of B-lymphocytes, which under certain conditions produce aPL.
APL bind to phospholipids of cell membranes, changing the conformational and metabolic structure of the cell, which leads to disruption of cell function with the development of stasis and thrombosis. Due to the fact that vessels of different sizes and different locations are affected, the range of clinical manifestations of APS is diverse - thrombosis, strokes, obstetric pathology, thrombocytopenia. The incidence of aPL in various pathological conditions is presented below.
Pathological condition/APL detection frequency, %:
- Recurrent venous thrombosis: 28–71
- Recurrent miscarriage: 25–64
- Transverse myelitis: 50
- Thrombocytopenia: 27–33
- Hemolytic anemia: 38
- Arterial thrombosis: 25–31
- Pulmonary hypertension: 20–40
The most significant manifestation of APS is obstetric pathology associated with placental decidual vasculopathy - recurrent miscarriage, antenatal fetal death (usually in the 1st and 2nd trimester), severe forms of gestosis, intrauterine growth retardation.
In the population, aPL is found in 2–4% of the population. The incidence of aPL increases in patients with autoimmune, inflammatory, infectious diseases, malignant tumors, while taking oral contraceptives, psychotropic drugs. APS can be primary (there are no signs of other autoimmune diseases) or secondary (against the background of other autoimmune diseases, most often systemic lupus erythematosus). There is also a seronegative variant of APS, characterized by the absence of aPL and lupus anticoagulant in the presence of clinical manifestations of APS. In this form, only antibodies to glycoprotein I are detected.
The main criterion for the laboratory diagnosis of APS is the presence of aPL (or antibodies to cardiolipin) and lupus anticoagulant in 2 or more studies at least 6 weeks apart.
Indications for prescribing analysis for aPL:
- Obstetric pathology (recurrent miscarriage).
- Recurrent thrombosis of various locations.
- Systemic connective tissue diseases (systemic lupus erythematosus, Sjogren's syndrome).
- Thrombocytopenia.
- False-positive reaction to syphilis using cardiolipin antigen (RW, RPR).
Indications of basic coagulation tests
Test Deficiency and/or inhibition of factors/Effects of anticoagulants
XII, XI, IX, VIII, von Willebrandt, Fletcher, Fitzgerald factors V, X VII II (prothrombin) I (fibrinogen) direct/indirect.
- Thrombin time
- normal/normal/normal/extended/extended/extended/normal. - APTT
- prolonged/prolonged/normal/normal/prolonged/normal/prolonged/prolonged/prolonged. - Prothrombin time (INR)
- normal/extended/extended/extended/normal/extended/extended/extended. - Fibrinogen
- normal/normal/normal/reduced or undetectable/reduced or undetectable/normal/reduced/normal.
Note.
Prothrombin time (INR) results are inversely proportional to prothrombin index results. Outdated methods for studying hemostasis disorders and options for their replacement
Method/Disadvantages/Modern methods.
- Clotting time/Low standardization/APTT.
- Recalcification time/Low standardization/APTT.
- Plasma tolerance to heparin/Low standardization/Plasma thrombin-heparin time, determination of anti-Xa activity.
- Autocoagulation test (ACT)/Low standardization/APTT, antithrombin III activity.
- Beta-naphthol (fibrinogen B), ethanol or protamine sulfate tests / Low-informative, low-quality expression of results, often false positive / Tests for thrombinemia: quantitative determination of SFMC (soluble fibrin-monomer complexes).
Optimal complex of hemostasiological laboratory tests
Test/Hemostasis link/Diagnostic significance.
- Platelet count/Vascular platelet/Main component of platelet hemostasis.
- Von Willebrand factor (VWF)/Vascular platelet/Plasma platelet adhesion cofactor and marker of vascular wall endothelial damage.
- Prothrombin time (PT)/Procoagulant (extrinsic coagulation mechanism)/Screening test to determine the factors (fibrinogen, prothrombin, factors v, VII and X) involved in blood clotting initiated by high concentrations of tissue factor.
- APTT (aPTT)/Procoagulant (intrinsic coagulation mechanism)/Screening test to determine factors (fibrinogen, prothrombin, factors V, VIII, IX, X, XI, XII, prekallikrein and high molecular weight kininogen) involved in blood coagulation upon contact activation. A phospholipid-dependent screening test that provides insight into disorders associated with the effect of the lupus anticoagulant - VA.
- Thrombin time (TT)/Procoagulant (fibrin formation)/Screening test of the last stage of blood coagulation - reaction between thrombin and fibrinogen - anticoagulant activity of antithrombin III.
- Fibrinogen/Procoagulant (substrate)/The main substrate from which fibrin is formed under the action of thrombin.
- D-dimer/Procoagulant and fibrinolytic (activation of coagulation in vivo)/Fibrin degradation product, one of the most specific tests for the diagnosis of DIC syndrome, thrombophilia and thrombosis, a marker of thrombin formation, fibrin formation and activation of secondary fibrinolysis.
- Antithrombin III/Anticoagulant/Basic physiological anticoagulant, for which heparin is a cofactor, inactivates thrombin and active factors IX, X, XI, XII.
- Protein C / Anticoagulant / Physiological anticoagulant, in the activated state, inactivates active factors V, VII, inhibits plasminogen activator (activity manifests itself mainly in the microcirculatory bed).
- Lupus Anticoagulant (LA) Confirmatory Test/Done as part of an extended screening test to confirm the presence of LA.
It is possible that this range of studies is insufficient for patients with severe pathology of the hemostatic system, but in the case of preliminary screening and monitoring of therapy, it seems necessary and sufficient.
Indications for analysis
Determination of the level of fibrinogen in the blood is most often carried out as part of an assessment of the blood coagulation system, as well as if hereditary disorders of the synthesis of this protein, liver pathologies and most inflammatory diseases are suspected.
Prolonged bleeding is an indication for fibrinogen testing. Photo: Crystal (Crystl) from Bloomington, USA / Wikipedia (CC BY 2.0)
The main indications for taking an analysis are:
- Prolonged bleeding even with minor injuries.
- Bleeding disorders and associated genetic diseases in close blood relatives.
- Cases of intravascular coagulation (thrombosis).
- Suspicion of congenital or acquired fibrinogen deficiency.
- Diseases of the cardiovascular and hematopoietic system.
- Recent extensive burns or severe injuries.
- Control of blood clotting during treatment with drugs that affect hemostasis (anticoagulants, coagulants, thrombolytics).
- Progressive liver diseases.
- Planned preparation for surgery.
- Screening diagnostics during pregnancy.
Complexes with this research
Pregnancy planning.
Clinical indicators 6,800 ₽ Composition Coagulogram Study of the functional state of hemostasis 2,080 ₽ Composition
Male check-up No. 1 39 studies for annual preventive examination 18,920 ₽ Composition
IN OTHER COMPLEXES
- Women's check-up No. 1 RUB 19,720
- For those at risk of COVID-19 RUB 4,620
- Female infertility RUB 16,470
- Joining IVF RUB 23,500
- Examination during pregnancy. 1st trimester 17,040 RUR
Preparing for analysis
No specific preparation is required before the test; following routine rules before collecting blood for most laboratory tests is sufficient. These include:
- fasting for 12 hours before donating blood;
- exclusion of physical and psycho-emotional stress several hours before the analysis;
- Stop smoking 30 minutes before donating blood.
Additionally, it is recommended to avoid consuming large amounts of fatty and fried foods, smoked foods and alcohol several days before the test.
Important!
On the eve of the test, you should discuss with your doctor the effect of medications taken on the test results. If possible, it will be necessary to temporarily interrupt the course of treatment to obtain reliable values. In addition to drugs that directly affect the blood coagulation system, androgens, antioxidants and oral contraceptives can distort the indicators.
Drawing blood for fibrinogen testing is a relatively simple and quick procedure. It is not much different from most other laboratory diagnostic methods for which venous blood is used. Typically, it does not have serious side effects. The amount of blood taken is insignificant.
Blood for fibrinogen testing is taken from a vein. Photo: npstockphoto/Depositphotos
Sometimes after the procedure a person may feel slight dizziness or general weakness. There may also be mild soreness or a slight bruise at the injection site in the cubital fossa - both are harmless. These symptoms usually go away within a few days.
Fibrinogen level in blood
Normal levels of fibrinogen in the blood depend on the specific laboratory in which the study is performed, reagents and equipment. Therefore, normal values are often indicated on the form next to the obtained indicator. Physiological fluctuations are also observed during pregnancy (Table 1).
In most cases, the concentration of fibrinogen in blood plasma is considered to be within the range of 1.8 - 3.5 g/l.
In infants, normal values are considered to be 1.25-3 g/l. Table 1. Normal fibrinogen levels depending on the week of pregnancy
| Weeks of pregnancy | Normal values |
| 1-13th | 2.12 - 4.33 g/l |
| 13-21st | 2.9 - 5.3 g/l |
| 21st-29th | 3 - 5.7 g/l |
| 29-35th | 3.2 - 5.7 g/l |
| 35-42nd | 3.5 - 6.5 g/l |
Danger during pregnancy
During pregnancy, it is normal if the analysis shows that fibrinogen is elevated in the blood. However, an excessive increase in fibrinogen leads to:
- pathologies of placenta functioning;
- development of vascular thrombosis in the umbilical cord;
- late toxicosis;
- the dangers of early spontaneous abortion;
- stopping the development of pregnancy;
- premature labor.
In order to prevent complications, a woman is regularly prescribed several coagulograms throughout the entire period of bearing a child. In early pregnancy, this allows assessment of initial fibrinogen. An analysis taken immediately before birth helps to promptly identify the risk of thrombosis.
Causes of elevated blood fibrinogen
High levels of fibrinogen in the blood (hyperfibrinogenemia) are associated with an increased risk of intravascular coagulation and thrombosis. However, in some cases, this phenomenon is a normal response of the body to certain changes. These, in addition to pregnancy, include:
- menstruation;
- taking oral contraceptives;
- previous operations;
- received burns and injuries;
- vegetarianism;
- taking medications from the group of androgens (male sex hormones), antioxidants.
Previous operations are one of the reasons for the increase in fibrinogen.
Photo: photographee.eu / Depositphotos Also, the following diseases and pathological conditions can be the causes of increased levels of fibrinogen in the blood plasma:
- inflammatory diseases of various localizations: pyelonephritis, glomerulonephritis, pancreatitis, hepatitis, pneumonia;
- infections: influenza, infectious mononucleosis, COVID-19, tuberculosis;
- malignant neoplasms;
- myocardial infarction, stroke;
- autoimmune pathologies: amyloidosis, scleroderma;
- endocrine pathologies, including diabetes mellitus, hypothyroidism, rheumatoid arthritis.
Literature
- Thachil J., Tang N., Gando S., et al. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J. Thromb Hemost. 2020; 18(5): 1023–1026. DOI: 10.1111/JTH.14810.19
- Garrido I., Liberal R., Macedo G. Review article: COVID-19 and liver disease - what we know on 1st May 2022. Alimentary pharmacology and Therapeutics. 2020; 52:267–275. DOI: 10.1111/apt.15813
- Temporary guidelines “Prevention, diagnosis and treatment of new coronavirus infection (COVID-19).” Ministry of Health of the Russian Federation, 2022. Version 7. 166 p. Access mode: https://mpmo.ru/content/2020/06/Metodicheskie-recomendatsii-minzdrava-RF-versiya-7.pdf.
- Tang N., Li D., Wang X., Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020; 18(4): 844–847.
- Huan H., Lan Y., Liu R., et al. Prominent changes in blood coagulation of patients with SARS-Cov2 infection. Clin Chem Lab Med. 2020; 58(7): 1116–1120. DOI: 10/1515/cclm-2020-0188
- Tang N., Li D., Wang X., Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Hemost. 2020; 18(4): 844–7. DOI: 10.1111/jth 14768
- Bulanov A.Yu., Roitman E.V. New coronavirus infection, the hemostatic system and problems of heparin dosing: this is important to say now. Thrombosis, hemostasis and rheology. 2020; 2: 11–18. DOI: 10.2555/THR.2020.2.0913.
- Galstyan G.M., Gaponova T.V., Zhiburt E.B. and others. Clinical use of cryoprecipitate. Hematology and transfusiology. 2020; 65(1): 87–114.
- Connors KP, Levy JH Thromboinflammation and the hypercoagulability of COVID-19. J Thromb Haemost. 2022. DOI: 10.1111/jth.14849
- Ranucci M., Ballotta A., Di Dedda U., et al. The procoagulant pattern of patients with COVID-19 acute respiratory distress syndrome (published online ahead of print 17 April 2020). J Thromb Haemost. 2020; 18: 1747–1751. DOI: 10.1111/jth.14854
- Xu L., Lu J., Yang D., Zheng X. Liver injury highly pathogenetic human coronavirus infections. Liver Int. 2020; 40:998–1004.
- Chau T.-N., Lee K.-C., Yao H., et al. SARS-associated viral hepatitis caused by a novel coronavirus; report of three cases. Hepatology. 2004; 39: 302–310.
- Cansu DU, Demirtas E., Andic N., et al. Is it required to routinely check fibrinogen level in patients with rheumatic diseases on tocilizumab? Case-based review. Rheumatol Int. 2019; 39(4): 743–750. DOI: 10/1007/s00296-019-04268-x
- Martis N., Chirio D., Queyrel-Moranne V., et al. Tocilizumab-induced hypofibrinogenemia: a report of 7 cases. Joint Bone Spine. 2017; 84(3): 369–370. DOI: 10.1016/j.jbspin.2016.04.008
- Imamura H., Momohara S., Yano K., et al. Tocilizumab treatment in patients with rheumatoid arthritis is associated with reduced fibrinogen levels and increased blood loss after total knee arthroplasty. Mod Rheumatol. 2018; 28(6): 976–980. DOI: 10.1080/14397595.2018.1428041
Causes of low fibrinogen in the blood
Fibrinogen deficiency in the blood plasma (hypofibrinogenemia) leads to impaired blood clotting and the inability to form a full thrombus. Clinically, this is manifested by prolonged bleeding.
The following pathologies and conditions may be the reasons for a decrease in fibrinogen levels:
- genetic diseases, including von Willebrand disease;
- renal failure due to liver cirrhosis, severe hepatitis;
- coagulopathies, disseminated intravascular coagulation syndrome (DIC);
- eclampsia (toxicosis during pregnancy);
- deficiency of vitamin C and B₁₂;
- amniotic fluid embolism;
- chronic myeloid leukemia;
- polycythemia - a pathology in which the bone marrow produces an excessive number of blood cells;
- previous blood transfusion;
- snake bite.
In some cases, low blood fibrinogen is the result of taking medications of the following groups:
- hormonal drugs from a number of anabolic steroids;
- thrombolytics (streptokinase, urokinase);
- medicines used for mental disorders and epilepsy (valproic acid);
- antiepileptic drugs (phenobarbital);
- preparations containing omega-3 and omega-6 fatty acids³.
A fibrin clot produced by adding thrombin to whole blood. Scanning electron microscopy. Photo: Sergey Obydenny / Wikipedia (CC BY-SA 3.0)
How to reduce fibrinogen in the blood?
First of all, it is important to identify the cause of the increased fibrinogen content in the blood plasma. As a rule, after the necessary diagnosis and elimination of the cause, the indicators return to normal values. If it is impossible to get rid of pathological changes, medications that prevent blood clotting are used:
- anticoagulants (sodium heparin, dicumarol, warfarin);
- antiplatelet agents (acetylsalicylic acid;
- thrombolytics (streptokinase, alteplase, tenecteplase).
In addition to medications, you can reduce the level of fibrinogen in the blood by adjusting your diet: you should increase the amount of fresh fruits and vegetables, berries, seafood, cocoa and dark chocolate in your diet.
Additional facts about fibrinogen
- The fibrinogen index, as a rule, is deciphered in conjunction with other tests, for example, PT and APTT.
- In the absence of a superficial reason for a decrease in the fibrinogen index and in the presence of some general clinical or medical history data, an immunological analysis of colorless protein is used to determine the basis of the disorders.
- To avoid incorrect results, blood testing for fibrinogen levels should not be performed on old specimens collected within 4 hours after administration of therapeutic doses of unfractionated heparin.
- High concentrations of unfractionated heparin may result in incorrect measurements of true fibrinogen levels.