Peritonitis is a process of inflammation of the peritoneum. With peritonitis, organ functioning is disrupted due to severe intoxication of the body. The connective tissue of the peritoneum envelops all the internal organs of the abdominal cavity and serves as a limiter between the internal environment of the abdominal cavity and the abdominal muscles.
When exposed to pathogenic microorganisms or chemical agents on the surface of the peritoneum, it is capable of releasing special substances that stop this process. If the number of pathogenic factors is large, then the peritoneum becomes involved in inflammation and peritonitis occurs. Peritonitis is a very life-threatening condition. If it occurs, emergency medical attention and urgent treatment are required, otherwise death is possible.
Causes of peritonitis
Peritonitis is a very serious condition!
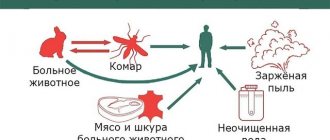
Peritonitis is classified as primary or secondary. In primary peritonitis, the causative agent is microorganisms that entered the peritoneum along with the blood flow from the infectious focus in the body. At the same time, the integrity of the peritoneum is preserved.
Primary peritonitis is classified as:
- spontaneous childhood primary peritonitis (usually girls under 7 years of age);
- spontaneous adult primary peritonitis (due to ascites, side effect of hemodialysis);
- primary peritonitis in persons suffering from active tuberculosis.
Secondary peritonitis is accompanied by damage or rupture of all layers of the peritoneum as a result of penetrating trauma to the abdomen or a violation of the integrity of one of the internal organs.
Secondary peritonitis is classified into:
- peritonitis caused by a violation of the integrity of internal organs;
- peritonitis caused by penetrating or blunt abdominal trauma;
- peritonitis, which developed in the postoperative period.
There is tertiary peritonitis, which develops in the abdominal cavity after peritonitis has already occurred. That is, in essence, this is a relapse of peritonitis. Fortunately, it is rare. Its peculiarity is an erased course, severe intoxication and failure of almost all internal organs. It occurs when the body's defenses are severely depleted. Such peritonitis often does not respond to therapy and ends in the death of the patient.
Peritonitis
Treatment of severe forms of peritonitis is a complex task that requires an integrated approach.
Already in the case of local peritonitis or the reactive phase of widespread (spread) peritonitis, the treatment program includes measures determined by the characteristics of the body’s response to the inflammatory process and the presence of concomitant diseases. If we are talking about the peritoneal form of abdominal sepsis, especially about severe sepsis and especially about its phase, which is called infectious-toxic (septic) shock (ITS), the implementation of a coherent system of sequential, timed therapeutic measures begins in the intensive care unit (and, if indicated, in the intensive care unit), continues during anesthesia, surgery, and then in the postoperative period.
However, in relation to peritoneal sepsis, they have a number of features. This applies to solving several problems. One of them is restoration of the volume and content of the body’s internal media. Research has established that in severe abdominal (peritoneal) sepsis, the loss of intracellular fluid reaches 15-18%, which is the maximum permissible value. It is clear that without eliminating cellular dehydration, i.e. Without restoring the main environment where vegetative processes occur, it is impossible to count on the correction of metabolic disorders. Therefore, the need to introduce large quantities
low-concentrated polyonic solutions (up to 100-150 ml per 1 kg of body weight) largely determine the content of infusion therapy on the first day of treatment. At the same time, the elimination of cellular dehydration must be the replenishment of the central nervous system, the restoration of ion-electrolyte, colloid-osmotic and acid-base relationships. In intensive care units equipped with an express laboratory, it is desirable to draw up an individual infusion therapy program during the first day of treatment, which is adjusted in accordance with the main indicators.
Another equally important task for patients with severe widespread peritonitis is the elimination of tissue hypoxia. Along with infusion-transfusion therapy, restoration of external respiration using modern equipment and auxiliary ventilation modes plays a special role in this regard.
The problem of detoxification is also solved in a comprehensive manner . Controlled hemodilution with forced diuresis is combined here with the rational use of extracorporeal detoxification methods, and the greatest intensity of activities in this group occurs in the postoperative period, when measures to eliminate the sources of endotoxemia have already been implemented. Also in the postoperative period, the tasks of restoring and maintaining plastic and energy potential are solved.
The development of peritonitis is accompanied by massive catabolism. The body's needs for energy and plastic resources increase sharply. On average, patients with peritonitis should receive at least 2500-3000 kcal per day.
The use of enteral tube feeding for peritonitis (from 3-4 days of the postoperative period) is promising. General somatic (symptomatic) therapy measures are individual in nature. It is important to emphasize once again that in case of widespread (spread) purulent peritonitis, surgical intervention plays a central and most important role in a comprehensive treatment program.
Preoperative preparation, along with generally accepted hygienic measures, includes the above areas of therapeutic influence (with the exception of extracorporeal detoxification, which involves preliminary elimination or delimitation of the source of endotoxemia). Note that the designation of the sufficiency of preoperative preparation for widespread peritonitis does not have clear universal criteria. It is generally accepted that for the vast majority of patients, the preparation time for surgery should not exceed one and a half to two hours. Moreover, taking into account some individual differences depending on the age of patients, body weight (which is determined approximately), and the presence of concomitant diseases, the general scheme of preoperative preparation should include:
• jet (in the presence of cardiopulmonary failure - drip) intravenous administration of low-concentrated polyionic crystalloid solutions in quantities of up to 1000-1500 ml, preferably under central venous pressure control;
• administration of 400-500 ml of colloidal solutions to replenish the volume of circulating fluid;
• intravenous use of broad-spectrum antibiotics 30-40 minutes before the start of surgery;
• correction of central and peripheral hemodynamics.
The need for intravenous administration of antibiotics in the preoperative period is determined by the inevitable mechanical destruction during surgery of biological barriers delimiting the area of the infectious process and the natural intestinal biocenosis. Therefore, surgery for peritonitis should be performed against the background of creating a therapeutic concentration of antibacterial drugs in the blood and tissues. Targeted studies have shown that, for example, the therapeutic concentration of penicillin and cefuroxime is achieved 50-60 minutes after the start of intravenous administration of the drug.
Preoperative preparation begins immediately after the diagnosis is made and ends in the operating room, gradually moving into the anesthesiological support of the operation. Surgery for widespread (spread) peritonitis is always performed under multicomponent general anesthesia with artificial ventilation.
Surgical intervention for widespread (spread) peritonitis involves the following main tasks:
• elimination of the source of peritonitis;
• intraoperative sanitation and rational drainage of the abdominal cavity;
• creation of conditions for prolonged sanitation of the peritoneal cavity in the postoperative period;
• drainage of intestines in a state of paresis;
• creation of favorable conditions for influencing the main pathways of resorption and transport of toxins (for special indications).
The most rational access for widespread peritonitis is a median laparotomy, which provides the possibility of a full inspection and sanitation of all parts of the abdominal cavity.
After opening the peritoneum, the pathological contents are removed as completely as possible - pus, blood, bile, feces, etc. This can be done most fully and less traumaticly with the help of an electric suction equipped with a special tip that prevents suction of intestinal loops and the greater omentum. Particular attention is paid to places where exudate accumulates - subdiaphragmatic spaces, lateral canals, and the pelvic cavity.
Then a thorough examination of the abdominal organs is performed to identify the source of peritonitis. This stage may be preceded by the injection of 150-200 ml of 0.25% novocaine solution into the root of the mesentery of the small intestine and under the parietal peritoneum.
To eliminate the source of peritonitis, the simplest and fastest method is used. In this case, it is necessary to balance the volume of intervention with the severity of the patient’s condition and not to expand the operation, striving in all cases to radically eliminate the underlying disease that caused peritonitis. Operations such as extensive resections and extirpations of organs in conditions of peritonitis should be considered a forced exception.
The next stage of the operation is sanitation of the abdominal cavity. It is necessary to pay special attention to this moment of intervention. Its inferiority cannot be compensated for by any efforts in the postoperative period. Sanitation consists of an additional revision after eliminating the source of infection and careful removal of exudate and pathological contents from the abdominal cavity, and when the process extends to all its parts, the best method of intraoperative sanitation is repeated washing of the abdominal cavity with sterile solutions. Usually saline solution and chlorhexidine solution are used. Washing is carried out in a gentle way, without eventrating the intestinal loops. The solution, heated to a temperature of 35-38 ° C, is poured into the abdominal cavity in such a quantity that the intestinal loops float in it. After washing the abdominal cavity, the solution is removed using an electric suction. Rinsing is carried out until “clean water”. Solid particles of food masses, feces, fibrin films, etc. carefully remove with tweezers or a tupper moistened with novocaine solution. For sanitation of the abdominal cavity, 4 to 8 liters of solution are usually used.
Then the issue of drainage of the small intestine is decided. It is indicated for severe signs of paralytic intestinal obstruction. The detection during operations of loops of the small intestine sharply distended by the contents, with flabby cyanotic walls covered with fibrin, with dark spots of subserous hemorrhages should be considered the basis for drainage of the intestinal tube.
In order to more objectively assess the potential for independent restoration of intestinal motility during peritonitis, determination of the regime of intrawall blood flow by transillumination tensometry is sometimes used. The absence of pulsating intramural arterial blood flow and a drop in blood pressure, determined by transillumination, to 40 mm Hg. Art. and below indicates deep ischemic changes in the intramural apparatus and is regarded as an indication for drainage of the intestinal tube.
Decompression of the small intestine can be quite effectively accomplished by nasogastroenteric drainage with a Müller-Ebott probe. In this case, of particular importance is the emptying and prolonged drainage of the initial section of the jejunum (50-70 cm from the ligament of Treitz), where the contents pose the greatest threat to the development of endotoxicosis. It is important to ensure complete drainage of the stomach itself, since insertion of the probe disrupts the function of the pyloric and cardiac sphincter, and the amount of intestinal contents entering the stomach may exceed the drainage capabilities of the probe, causing regurgitation and reflux of contents into the respiratory tract. To avoid this, it is not enough to have holes in the part of the tube that is in the stomach. You need either a separate probe channel ending in the stomach, or a separate probe inserted through another nasal passage. The drainage is retained in the jejunum for 3-4 days and is removed after the intestinal contents cease to flow through it (with mandatory monitoring of the patency of the probe!) and the appearance of intestinal sounds during auscultation. In the event that drainage of the intestinal tube involves dissection of adhesions caused by previous operations, the small intestine is drained along its entire length, and the probe is stored for 7-8 days. Only under this condition can it perform a frame function and eliminate the risk of developing adhesive intestinal obstruction in the immediate and late postoperative period.
Elderly patients with severe cardiopulmonary insufficiency, as well as wounded patients with concomitant damage to the chest organs, are difficult to tolerate nasogastroenteric drainage. For them, retrograde drainage through the ileum by enterostomy according to I.D. may be recommended. Zhitnyuk. For this purpose, a purse-string suture is placed on the wall of the ileum 20-60 cm from the ileocecal angle. A drainage tube is inserted through a puncture in the center of the pouch and advanced proximally to the level of the Treitz ligament. As the tube advances, the colon is emptied using an electric suction. The intestinal wall around the pouch is fixed to the peritoneum through a separate incision in the left iliac region. If the cecum is sufficiently mobile, it is permissible to perform a cecoenterostomy using the same technique. If the source of peritonitis is located in the upper floor of the abdominal cavity, and the most pronounced changes are in the proximal parts of the jejunum, it is more appropriate to apply a gastrostomy with a drainage tube passed distally through the ligament of Treitz.
The next task of the surgical aid is to create conditions for complete sanitation of the abdominal cavity in the postoperative period. This problem can be solved in different ways depending on specific conditions. An effective method of postoperative sanitation of the abdominal cavity is to irrigate it with an antiseptic solution (previously widely used solutions with antibiotics, as meta-studies have shown, do not have any advantages over conventional antiseptics, but at the same time contribute to the development of antibiotic resistance!). For this purpose, a drainage tube with a diameter of 3-4 mm with multiple perforations throughout the part that is located in the abdominal cavity is inserted through punctures in the right and left hypochondrium in the transverse direction. Both extended ends of the tube are used for drip (better) or fractional (worse) introduction of the solution into the abdominal cavity. If necessary, below the level of the first tube, at a distance of 10-15 cm, another is inserted in the same way.
In order to remove accumulated fluid, a double-lumen drainage tube is inserted into the pelvic cavity through an incision in the groin area on the left or right, allowing for active aspiration with the introduction of rinsing fluid through the nipple canal. The patient is placed horizontally and the head end of the bed is raised. If additional drainage of the lateral channels of the peritoneum is necessary, it is also carried out with double-lumen tubes through additional punctures of the abdominal wall.
Attempts to carry out postoperative sanitation of the abdominal cavity through several nipple drainages introduced into various sections between the intestinal loops or into the lateral channels of the peritoneum turned out to be ineffective. After a few hours, small closed cavities form around such microdrainages, which limit the contact of solutions with the peritoneum.
The primary operation is completed in case of widespread peritonitis and fully completed sanitation of the abdominal cavity by suturing the abdominal wall wound. In the presence of severe intestinal paresis or severe signs of inflammation of the visceral and parietal peritoneum, only the skin with subcutaneous tissue is sutured.
This, firstly, prevents the harmful consequences of an increase in intra-abdominal pressure in the first days after surgery, and secondly, it provides the opportunity to perform repeated programmed sanitation of the abdominal cavity a day later - two days later in case the surgeon is dissatisfied with the sanitation measures during the first operation. Sometimes, for this purpose, provisional sutures are placed on the abdominal wall or a closing device with a “zipper” is fixed on it, which some surgeons do not quite accurately designate as a “laparostomy”.
There are recommendations for the use of a true laparostomy, when the abdominal wall is not sutured and the intestinal loops are covered with ointment tampons, or when the treatment of an open abdominal wound is carried out in chambers with an abacterial environment, cause a critical attitude and, apparently, can only be used in exceptional cases.
When such situations develop secondarily as a result of repeated eventrations, leading to the formation of a wound of the abdominal wall with fixed edges, the bottom of which consists of intestinal loops, they must be isolated from direct contact with the external environment.
For this purpose, after short-term preparation with sanitizing dressings with water-soluble ointments, the intestinal loops are covered with a split perforated (dermotomy) free flap of autoskin. The damage from a false ventral hernia of the abdominal wall resulting from this technique is “compensated” by preventing the death of the patient from widespread peritonitis or from the formation of multiple small intestinal fistulas.
In recent years, in connection with the development of endovideosurgical technologies, it has become possible to carry out with their help programmed or indicated repeated sanitation of the abdominal cavity after surgery for widespread peritonitis, without resorting to relaparotomy. The special elevators available for this make it possible to avoid the need for massive insufflation of gas into the abdominal cavity and to successfully perform inspection and sanitation of various parts of the abdominal cavity.
General measures for the treatment of abdominal sepsis are carried out in accordance with the principles set out in Chapter IV of this manual. Certain features represent two areas of complex treatment of abdominal sepsis caused by widespread peritonitis: providing adequate nutrition in the catabolic phase of the postoperative period and antibacterial therapy.
The first direction involves the introduction, along with modern technologies of parenteral nutrition, of methods of early enteral nutrition using special nutritional compositions and the simultaneous introduction of digestive enzymes. If tube feeding is not possible (the source of peritonitis is located in the upper abdominal cavity), enterostomy can be used for these purposes in the initial parts of the jejunum using endovideosurgical technology. The experience of the still few observations of the use of this technique encourages a positive assessment of its prospects.
Intra-abdominal hypertension syndrome
During the treatment of abdominal sepsis and widespread peritonitis, especially in the early postoperative period on days 1-3, a complication began to emerge more and more often, requiring separate consideration due to the peculiarities of its pathogenesis.
Intra-abdominal hypertension syndrome (SIAH) (Abdominal Compartment Syndrome) was first described by Kron et al in 1984 as a possible complication after surgery for a ruptured abdominal aortic aneurysm. In the subsequent period, a large number of studies were devoted to this complication, and now it has become possible to believe that the frequency of SIAH in the postoperative period (after operations on the abdominal organs) reaches 15-20%, but critical forms with the development of multiple organ failure syndrome are much less common .
The rise in intra-abdominal pressure that develops after closure of the abdominal cavity in patients operated on for generalized peritonitis can lead to the development of a syndrome similar in clinical picture to multiple organ failure syndrome. It should be noted that if typical MOF in patients with sepsis, regardless of the nature of the latter, develops as a result of the induction of an inflammatory cascade by microorganisms or their metabolic products with subsequent disruption of microcirculation in distant organs, then an increase in intra-abdominal pressure itself causes a disruption of microcirculation in the splanchnic system.
Microcirculation disorders in the form of sludge and increased permeability of the vascular wall are the leading link in the pathogenesis of SIAH. Carrying out large-volume infusion-transfusion therapy under these conditions leads to an increase in the volume of extracellular fluid. The effect subsequently increases as a result of a decrease in the elasticity of the anterior abdominal wall, as a result of increasing ischemia and tissue edema. This, in the most general form, is the pathogenesis of SIAH.
The risk group for developing SIAH includes patients who have developed, for a number of reasons, an increase in the volume of internal organs in the peritoneal cavity. Among them are patients with severe widespread peritonitis, requiring large volumes of infusion therapy in the postoperative period. This group also includes patients with intestinal obstruction in whom, for one reason or another, drainage of the small intestine failed (was not performed).
The clinical manifestation of SIAH is the rapid development of renal failure (in the form of oliguria) and progressive respiratory failure. The genesis of oliguria in SIAH is renovascular compression, therefore a characteristic clinical sign of oliguria in SIAH is its resistance to infusion therapy and stimulation. An increase in pressure in the airways during artificial ventilation of the lungs, requiring an increase in pressure in the circuit of the device in order to provide the necessary tidal volume - along with resistant oliguria, an early and reliable sign of SIAH.
The most accessible and clinically effective diagnostic technique to identify increasing intra-abdominal pressure is catheterization of the bladder and determination of intravesical pressure. The basis for extrapolating intravesical pressure to pressure in the abdominal cavity was the fact that when the bladder is filled from 50 to 100 ml, it is a passive diaphragm, reflecting intra-abdominal pressure. In this regard, the method for determining intra-abdominal pressure includes filling the bladder with 70-100 ml of solution (physiological, antiseptic, etc.) with subsequent recording of the pressure level.
According to the literature, the pressure is less than 10-15 mm Hg. is clinically insignificant, 16-20 mmHg. is insignificant, 21-30 mmHg. moderate, more than 30-35 mm Hg. - potentially dangerous. It should be immediately emphasized that this gradation is very arbitrary and its main purpose is to assess the dynamics of intra-abdominal pressure. The appearance of clinical signs of SIAH, along with increased intra-abdominal pressure, makes it possible to make an early diagnosis.
Treatment for SIAH is surgical only. In 93% of cases, laparotomy and release of internal organs with the formation of a temporary laparostomy lead to success - rapid regression of developing MODS. The average lifespan of a laparostomy in this situation is 2-4 days.
Antibacterial therapy for peritonitis: basic principles
After adequate surgical sanitation of the focus of peritonitis, the rational use of antibiotics in the complex treatment of abdominal sepsis takes first place in importance. The choice of antibiotic therapy regimen is determined by several important factors. The first, and one of the most important, is the type of peritonitis, which means primary, secondary, tertiary. Each of them is characterized by its own set of microorganisms, knowledge of which allows you to plan competent empirical therapy. After receiving the results of a microbiological study, adjustments to antibacterial therapy regimens are made, but only in cases where it is ineffective.
Primary peritonitis accounts for approximately 1% of all clinical cases of peritonitis. It develops in patients suffering from severe underlying diseases, and the main pathogens are pneumococci - Strept. pneumoniae and gram-negative bacilli - Esherichia coli, Klebsiella spp. As a rule, there are no anaerobic microorganisms among the pathogens, and the infectious process is caused by a single pathogen and not by a polymicrobial flora. Pathogens enter hematogenously or through translocation through the intestinal wall. The choice of antibiotic is determined taking into account the sensitivity of the microflora and the toxicity of the drug, as well as taking into account the underlying disease (liver cirrhosis, chronic renal failure, etc.). Among the most commonly used drugs are the following: aminoglycosides (gentamicin, amikacin, netromycin), cephalosporins III - IV (ceftriaxone, ceftazidime, etc., cefepime).
Secondary peritonitis, most often encountered in clinical practice, is caused by enteral gram-negative pathogens and obligate anaerobes. The choice of antibiotic is significantly influenced by the following factors. Firstly, this is, of course, the localization of the primary focus. Depending on whether the source is the upper gastrointestinal tract or the lower, biliary and urinary tracts, the predominant microflora growing in this zone is determined. Secondly, the most important factor is the severity of the patient’s condition and the degree of organ failure. These parameters are assessed using widely used scales - SAPS (most common in European countries) or APACHE II (used in the USA and Canada) and SOFA (see Chapter III). Depending on the severity of the patient’s condition, one or another regimen of antibacterial therapy is selected.
The general principle is that the more severe the patient's condition, the more powerful and less toxic antibiotics should be used. It is appropriate to emphasize that the use of reserve antibiotics ( IV generation cephalosporins, carbapenems) immediately after the start of antibacterial therapy in severe and extremely severe patients not only provides a better prognosis due to a wide spectrum and less toxicity, but is also economically more profitable.
One of the most difficult tasks, including the selection of antibacterial therapy, is the treatment of tertiary peritonitis, which
Initial (empirical) antibacterial therapy depending on the severity of the condition
| Severity of the condition | Antibacterial therapy regimens |
| SAPS < 12 | — Aminoglycoside III (Amikacin 1.0, netromycin 0.4 - 0.6 x 1 time i.v.) + metronidazole or clindamycin 0.3 x 3 i.v. — Amoxacillin/clavulanate 0.6 — 1.2 x 3-4 IV — Ampicillin/sulbactam — Cephalosporins III (ceftriaxone 1.0-2.0×1-2 IV) + metronidazole or clindamycin 0.3×3 IV |
| SAPS > 12 | — Cephalosporins IV (cefepime 1.0-2.0 x 2 i.v.) + metronidazole or clindamycin 0.3 x 3 i.v. — Carbapenems (Imipinem/cilastatin 0.5-1.0 x 3-4 i.v., Meropenem 0.5-1.0 x 3 i.v.) |
according to D.Fry, account for about 10% of all peritonitis. The causative agents in these situations are hospital strains that grow in specific intensive care units and general surgical departments. Data from epidemiological monitoring of microflora and its resistance can provide real assistance in choosing an antibiotic. Considering the fairly frequent involvement of methicillin-resistant Staphylococcus aureus, vancomycin or teicoplanin becomes the drug of choice (according to the literature, the use of a representative of the new group of antibiotics oxazolidinones, active against this pathogen - lincosamide - "Zyvox") is also very promising. Gram-negative microorganisms are covered by IV generation cephalosporins (cefepime), carbapenems (imipinem/cilastatin, meropenem - especially effective for infections caused by Pseudomonas aeruginosa).
When treating tertiary peritonitis, one must always remember the risk of developing a systemic fungal infection, especially often systemic candidiasis. Therefore, careful monitoring of all possible regions of its localization with periodic microbiological monitoring is necessary. The use of antifungal drugs as a prophylactic agent remains to this day an issue that does not have a clear solution. Most researchers are inclined to think that it is inappropriate to take fluconazole or itraconazole for prophylactic purposes. The extremely widespread belief about the preventive effectiveness of nystatin also not true, due to its extremely low bioavailability. It is effective only for candidiasis of the mucous membranes of the oral cavity and upper gastrointestinal tract.
Apparently, it is worth noting here that the selection, control and change of antibacterial drug regimens should be carried out by a trained specialist. Only in those conditions when the process of selecting and prescribing antibacterial drugs is based on deep knowledge and experience can one count on the success of the therapy, with minimal risk of the formation of resistant strains of microorganisms.
The process of development of peritonitis
The speed and severity of the development of peritonitis symptoms largely depends on the state of the body, on the pathogenicity of microbes, and on the presence of provoking factors.
The main points in the development of peritonitis are as follows:
- Intestinal paresis, as a result of which the absorption function is impaired, and the body loses a large amount of water and electrolytes.
- Dehydration and decreased pressure in blood vessels leads to strong heartbeat and shortness of breath.
- The rate of development of peritonitis and the severity of damage to the peritoneum depends on the number of pathogenic bacteria and the magnitude of intoxication.
- Autointoxication is added to intoxication caused by microbes. In response to the aggression of microorganisms, antibodies are released in the blood that attack the lipopolysaccharide wall of the bacterium. The compliment system is activated and many active substances are released, the effect of which is manifested by intoxication.
If the human body is weakened or the microorganism is highly pathogenic, then peritonitis is not limited, but becomes diffuse or widespread. The spread is especially facilitated by increased peristalsis, as well as blood and exudate in the abdominal cavity.
Secondary peritonitis
It occurs as a complication of one of the gynecological diseases - acute adnexitis, salpingitis, septic tubo-ovarian formations, suppuration of pelvic hematomas, etc. The diagnosis of “secondary pelvioperitonitis” is also made if the infection has spread from other organs - the appendix, intestines. In this case, treatment is complicated, because the doctor has to deal with several pathologies.
Microbes multiply quickly, causing inflammation, tissue swelling, severe pain and symptoms of general poisoning of the body. The result is blood poisoning, painful or septic shock.
The risk to life with pelvioperitonitis increases in women with chronic diseases of the liver, kidneys, and metabolism.
Clinical manifestations of peritonitis
The initial symptoms of peritonitis are very varied
Symptoms depend on the cause of the disease, so the initial signs can be very varied. But there are several successive stages, depending on the time of onset of symptoms.
Reactive stage
Develops in the first day. Severe pain occurs, the patient can clearly determine the location. If the cause of peritonitis is perforation of a hollow organ, then this pain is described as dagger-like. For example, perforation of a stomach ulcer is described as severe sharp pain in the epigastric region, rupture of the appendix is described as pain in the right iliac region.
The pain gradually spreads to other areas of the abdomen. Sometimes, after it occurs, the pain becomes less intense and does not bother the patient as much. This is how a symptom of imaginary well-being manifests itself. After some time, the pain returns.
The face of a patient with peritonitis is very typical. It is pale, sometimes even with an earthy tint. Covered with drops of sweat when pain occurs. Facial features become sharp due to dehydration. Severe pain forces the patient to take a comfortable position in order to somehow alleviate it. More often, a person lies on his side with his legs bent, sparing his stomach in every possible way, trying not to strain it.
When examining such a patient, tense abdominal muscles are found - a plank-shaped abdomen. The Shchetkin-Blumberg symptom is pronounced, in which a sharp removal of the hand from the surface of the abdomen at the time of palpation leads to increased pain.
Symptoms
Acute peritonitis occurs in three stages, each of which has its own manifestations.
On the first day from the onset of peritonitis, in the reactive stage, a local reaction to irritation of the peritoneum is noted. Initially, pain is localized where the source of inflammation is located, and can radiate to the shoulder, under the collarbone. Subsequently, the pain spreads throughout the abdomen. To alleviate the condition, a person assumes the “embryo” position, lying with his legs pressed to his stomach. The patient is concerned about dry mouth, nausea and vomiting, and loss of appetite. The toxic stage develops between four and seventy-eight hours. Characterized by increasing intoxication up to endotoxic shock, increased general manifestations - blood pressure decreases, heart rate increases, body temperature rises and breathing problems appear. The pain is diffuse in nature, its intensity decreases, as paralysis of the nerve endings of the peritoneum begins, bloating and constipation are noted.
In the terminal stage, after seventy-two hours from the onset of inflammation of the peritoneum, a gross disruption of vital processes inside the body occurs. The symptoms of peritonitis are dominated by manifestations of paralytic intestinal obstruction - intense abdominal pain, severe vomiting that does not bring relief, and severe bloating. The patient's condition is extremely serious, facial features are sharpened, blood pressure is sharply reduced, urine does not pass, consciousness is confused, limbs acquire a bluish or yellow tint, increased sweating and other signs of multiple organ failure are characteristic.
Chronic peritonitis is characterized by “blurred” symptoms that arise as a result of prolonged intoxication and the formation of adhesions in the abdominal cavity, disrupting the functioning of internal organs.
Pathology manifests itself:
- lack of appetite and weight loss;
- increased sweating;
- persistent low-grade fever up to 37.5 °C;
- bowel dysfunction;
- periodic abdominal pain and bloating.
Adhesions and dense scar cords make it difficult to empty the hollow organs, which is accompanied by dyspeptic symptoms - nausea, vomiting, flatulence, urination and menstrual disorders.
Methods for diagnosing peritonitis
Treatment of peritonitis - surgical method
In order to make a diagnosis of peritonitis, the doctor must rely on clinical data from the disease, medical history, external symptoms, and examination data of the patient.
Blood test and instrumental data are important.
Changes in the hemogram are aimed at increasing the number of white blood cells, shifting the formula to the left, and increasing ESR. These are universal signs of inflammation. Hemoglobin falls, the number of red blood cells decreases. Due to blood thickening, its clotting is impaired.
The main role is played by ultrasound of the abdominal cavity. It shows the primary localization of peritonitis, the affected organ and the degree of spread of the process throughout the peritoneum. The sooner a person with symptoms of peritonitis seeks help, the greater his chances of recovery. Therefore, if you have a disease that is accompanied by fever, uncontrollable vomiting, or abdominal pain, you must call a doctor. If he suspects peritonitis, he will urgently refer such a patient to the hospital.
Diagnostics
If, during a conversation with the patient and examination, the doctor suspects peritonitis in an adult or child, the patient is urgently hospitalized in a hospital inpatient unit, where further laboratory and instrumental studies are carried out to clarify the diagnosis.
The list of tests for peritonitis includes:
- Clinical blood test. During the purulent process, an increase in the number of leukocytes is determined, accelerated ESR, and the hematocrit changes.
- Biochemical blood test to determine indicators such as C-reactive protein, aspartate aminotransferase, alanine aminotransferase, total bilirubin, blood sugar, creatinine, lactate dehydrogenase, amylase, lipase, procalcitonin, interleukins 1, 6, 8, 10, tumor necrosis factor, urea, total protein and albumin.
- Hemostasis indicators, fibrinogen concentration, prothrombin time, INR, APTT.
- Content of electrolytes in the blood.
- General urine analysis.
Instrumental diagnosis of peritonitis consists of ultrasound and survey R-graphy of the abdominal organs, electrocardiography, magnetic resonance and computed tomography. In complex clinical cases, to clarify the nature of the causative agent of the disease and confirm peritonitis, abdominal puncture, bacteriological examination of peritoneal exudate and laparoscopy are performed.
Treatment methods for peritonitis
Peritonitis is treated surgically. The operation is prescribed urgently, after appropriate preparation of the patient. The surgeon will open the abdominal cavity, eliminate the cause of peritonitis, suture the diseased organ, perform an inspection, and wash the internal organs and peritoneum with an antiseptic and saline solution. If peritonitis has affected a large part of the peritoneum, the wound is not tightly sutured, but additional lavage of the abdominal cavity is performed on the second and third days.
Signs of peritonitis
The symptoms of peritonitis are very characteristic, so every surgeon can diagnose it!
Manifestations of peritonitis are due to the reasons that provoked its development. But the main signs of one stage or another are the same in any case.
Reactive stage
This is the first stage, it occupies the first day of the disease. The lesions are local in nature. Patients first feel sharp pains that appear unexpectedly. In this case, you can accurately determine the place where the pain comes from. Some compare the pain at this stage to the blow of a dagger.
The localization of pain is associated with the organ that became the source of the disease. For example, with appendicitis, pain will be felt in the inferolateral zone on the right. If this is a perforation of a stomach ulcer, then pain will appear in the left hypochondrium or in the epigastric region. The pain is felt strongly, and it gradually spreads.
Preoperative preparation and monitoring
- For successful surgical intervention, it is necessary to carry out preoperative preparation.
- The patient must have a peripheral and central vein and bladder catheterized and premedicated.
- Midazolam (5 mg) and 10–20 mg of cerucal are administered on the operating table. Atropine administration is contraindicated, as there is a high probability of developing bradycardia.
- Medicines are administered that help reduce the acidity of gastric juice (about 40 mg of omeprazole or famotidine/ranitidine 50 mg into a vein).
- During the operation, infusion therapy is carried out in an amount of at least 1.5 liters of physiological solution, and plasma and blood products are added if necessary.
- Perform artificial ventilation and administer oxygen.
In the case when the patient lies on the operating table and there is more than 25 ml of contents in the stomach, there is a real threat of aspiration. This is the name for the entry of stomach contents into the lumen of the bronchial tree. Gastric juice can cause a burn to the mucous membrane of the bronchi and trachea. Complications of aspiration include multiple pulmonary atelectasis, bronchospasm, respiratory failure, and pulmonary edema.
Aspiration of small amounts of gastric juice can subsequently lead to aspiration pneumonia.
Therefore, in anesthesiological practice in patients with peritonitis, ganglioblockers and anticholinergics - drugs that can reduce the tone of the lower esophageal sphincter - are not used.
Antibacterial therapy is carried out with a combination of antibiotics that act on both Gram-plus and Gram-minus bacteria. For community-acquired peritonitis, this is intravenous administration of cefotaxime and metronidazole. For in-hospital use - cefepime and metronidazole. If peritonitis develops in the hospital during antibiotic therapy, carbapenems are used.
Peritonitis - what kind of disease is it?
Peritonitis is an inflammatory disease of the peritoneum, accompanied by acute abdominal pain, tension in the muscles of the abdominal wall, elevated body temperature, nausea, flatulence, constipation and general severe malaise of the patient.
The peritoneum (lat. peritoneum) is a serous membrane consisting of parietal and visceral layers, between which there is a cavity filled with serous fluid. The visceral layer covers the internal organs in the abdominal cavity, and the parietal layer lines its inner wall. The peritoneum protects internal organs from infection, damage and other unfavorable factors affecting the body.
The main causes of peritonitis are internal diseases of the gastrointestinal tract, their perforation, as well as infection, mainly bacterial. For example, the cause of irritation, and then inflammation of the peritoneal wall, can be hydrochloric acid released from the stomach during an ulcer with perforation. The same consequences can occur in the presence of appendicitis, pancreatitis, diverticula, etc.
Peritonitis is a serious, life-threatening disease that requires emergency hospitalization and adequate treatment. If you delay the provision of medical care, the prognosis for the patient is very unfavorable.
Development of peritonitis
The course of peritonitis can be divided into three stages.
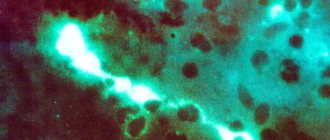
Stage 1 peritonitis (reactive, duration – up to 12 hours) is the body’s initial reaction to infection entering the abdominal cavity, accompanied by a local inflammatory reaction of tissues in the form of edema, hyperemia, and accumulation of exudate. The exudate is initially serous, and as bacteria and protective cells (leukocytes) accumulate in it, it becomes purulent. The peritoneum has an interesting feature - using the method of gluing and adhesions of leaves to separate (delimit) pathogenic microflora from other parts of the body. Therefore, due to fibrin deposits, at this stage, adhesions appear in the peritoneum and nearby organs. In addition, at the site of the inflammatory reaction, swelling and infiltration processes may be observed in nearby organs.
Stage 2 peritonitis (toxic, duration – up to 3-5 days) – is accompanied by the entry into the bloodstream and lymphatic system of bacteria, waste products of infection (endotoxins) and protein products (proteases, lysosomal enzymes, polypeptides, etc.), as well as more active immunological (protective) reaction of the body to the inflammatory process. There is inhibition of intestinal contractility, degenerative changes in surrounding organs, hemodynamic disorder (with a decrease in blood pressure), typical signs of septic (endotoxin) shock - blood clotting disorders, and others. In addition, symptoms such as nausea, diarrhea with constipation, general malaise, flatulence, increased and high body temperature, and abdominal pain are typical. The toxic phase of the disease can lead to the development of myocarditis, pericarditis and endocarditis, characterized by disruption of the entire cardiovascular system.
Stage 3 peritonitis (terminal, duration - from 6 to 21 days) - characterized by high temperature, which after some time drops to low levels, chills, rapid pulse, decreased blood pressure, pale skin, nausea, vomiting, rapid weight loss, acute abdominal pain, diarrhea. The function of the liver to produce protein decreases, which is why its level drops, and the amount of ammonium and glycol in the blood increases. The brain, whose cells swell and the amount of cerebrospinal fluid increases, does not remain unaffected.
Pathogenesis of peritonitis
On the part of the circulatory system, hypovolemia develops, which is accompanied by an increase in heart rate, an increase in blood pressure, which soon drops to low values, a decrease in the speed of portal blood flow, a decrease in venous return to the heart, and tachycardia.
From the gastrointestinal tract - intestinal atony appears as a reaction to the inflammatory process. Due to impaired blood circulation in the intestinal wall and irritation of its neuromuscular system by toxins, persistent paresis of the gastrointestinal tract develops, which in turn leads to hypovolemia, acid-base balance disorder, deposition of a large volume of fluid in the intestinal lumen, water disturbances, electrolyte, protein and carbohydrate metabolism. Signs of disseminated intravascular coagulation also appear.
On the part of the respiratory system - disorders appear mainly in the late stages of the development of peritonitis and are characterized by hypoxia, impaired microcirculation in the lungs and their edema, pulmonary perfusion appears, which, in combination with hypovolemia, leads to disruption of the myocardium and lungs.
On the part of the kidneys - as a result of the body’s general reaction to stress, at the first (reactive) stage of peritonitis, spasms and processes of ischemia of the cortical layer appear, which, in combination with arterial hypotension and hypovolemia, leads to a deterioration in the functioning of the kidneys, the final result of which can be acute renal failure (AKI) or renal-liver failure.
On the part of the liver - disorders are observed in the initial stages of the development of the disease, and are characterized by hypovolemia and hypoxia of liver tissue, which ultimately can lead to degeneration of the parenchyma.
Peritonitis statistics
The end result of the development of peritonitis in 20-30% of cases is death, and in case of complications, mortality increases to 60%.
Postoperative period
Antibiotic therapy for peritonitis is mandatory
In the postoperative period, some problems may arise related to the normal functioning of the intestines, severe pain, and the development of purulent complications. Recommended:
- observation of the patient, hourly assessment of respiratory rate, pulse, diuresis, central venous pressure, drainage discharge;
- infusion therapy with colloid and crystalloid solutions is carried out;
- to warm patients, infusion media are heated to body temperature;
- the lungs are ventilated for 72 hours to ensure sufficient oxygen supply to organs and tissues;
- a glucose solution is administered through a nasogastric tube;
- early restoration of intestinal motility;
- prevention of pain syndrome. Narcotic analgesics are used in combination with non-steroidal anti-inflammatory drugs. Fentanyl, morphine, ketorolac are used.
Primary peritonitis
Primary pelvioperitonitis is said to occur when pathogenic microorganisms penetrate the small pelvis directly - during gynecological operations and manipulations (surgical abortion, curettage, blowing of the fallopian tubes, etc.). Most often, it is associated with unsanitary conditions, violation of the rules for performing the operation, the use of reusable instruments, etc. For this reason, it is important to seek treatment in reliable modern clinics, where sterility standards are strictly monitored, and professional surgeons will not allow complications.
Treatment of pelvioperitonitis
Treatment of pelvioperitonitis
carried out only in a specialized hospital. Depending on the patient’s health condition, conservative therapy or surgical treatment may be performed.
As a rule, with a relatively mild course of pelvioperitonitis
, which began recently, the patient receives individual antibacterial therapy (depending on microscopic examination data). Recommendations also include bed rest, rest, cold on the lower abdomen, infusion-detoxification therapy, vitamin therapy (in food and intravenously), balanced, easily digestible nutrition, etc.
When an abscess forms in the space of Douglas, as well as when there is a threat of spread of the inflammatory process to the peritoneum, when conservative treatment is ineffective, when signs of pelvioperitonitis increase, surgical treatment (colpotomy, puncture), further antibacterial therapy, and drainage are indicated.
With timely provision of medical care, the prognosis for pelvioperitonitis
favorable. If you notice alarming symptoms that may indicate the development of pelvioperitonitis, consult a doctor immediately!
Symptoms of pelvioperitonitis
may be similar to the clinical picture of diffuse peritonitis (at the onset of the disease), acute appendicitis, impaired tubal pregnancy, torsion of the pedicle of an ovarian cyst and other diseases, each of which requires immediate provision of qualified medical care. It is very difficult for a non-specialist to distinguish one disease from another by eye.
Gynecologists at GUTA CLINIC, using today's most advanced specialized equipment, rich clinical experience and excellent diagnostic skills, can easily make an accurate diagnosis and prescribe individual treatment. By contacting a gynecologist on time, you will preserve not only your health, but also the desired quality of life.
Types of peritonitis
Peritonitis is classified as follows...
According to the clinical course:
- Acute peritonitis;
- Chronic peritonitis.
By the nature of the exudate:
- Serous - only the usual fluid produced by the serous membrane is present;
- Fibrinous - in the serous fluid there are fibrin fibers that form adhesion processes;
- Purulent - pathological exudate consists of pus;
- Hemorrhagic - pathological exudate contains blood impurities.
By etiology
- Infectious (bacterial) peritonitis - the cause of the disease is infection; — Aseptic; — Special forms:
- Peresitary;
- Rheumatoid;
- Granulomatous;
- Carcinomatous.
According to the nature of infection:
Primary – the infection penetrates the peritoneum by hematogenous (through the blood) or lymphogenous (through lymph) route.
Secondary – infection of the peritoneum occurs due to trauma or surgical diseases of the abdominal organs. Can be divided into:
- Perforated;
- Infectious-inflammatory;
- Traumatic;
- Postoperative.
Tertiary - the development of the inflammatory process occurs when the peritoneum is infected against a background of weakened immunity or exhaustion of the body - after injuries, operations, general pathological conditions due to exposure to adverse factors (frequent stress, hypothermia, hypovitaminosis, vitamin deficiencies, poor-quality nutrition, drug abuse without consultation with a doctor).
By prevalence:
Local - characterized by inflammation in one anatomical part of the abdominal cavity. May be:
- Limited peritonitis - characterized by the formation of abscesses or infiltrate;
- Unbounded – characterized by the absence of clear boundaries of inflammation.
Common - characterized by the formation of 2-5 inflammatory-pathological areas in various parts of the abdominal cavity.
General (total) – characterized by total damage to the peritoneum.
Signs of acute peritonitis in children
Peritonitis in a child has a number of features due to incompletely formed systems and organs. In children, the general condition deteriorates first. Local symptoms are not as pronounced. Clinical manifestations include high temperature (over 38 degrees), restlessness (lethargy), abnormal stool, repeated vomiting, bluish skin discoloration and the addition of symptoms of peritoneal irritation.
On our website you will find more detailed information. Our consultants will help you make an appointment with the right specialist and answer all your questions. The consequences of complications of peritonitis in children will be discussed further.