Tuberculosis is an infectious disease that occurs due to Koch bacilli entering the human body. The disease is dangerous because it affects the respiratory system. Less commonly susceptible to tuberculosis are the bones, skin, lymphatic, genitourinary, nervous, lymphatic systems, as well as other organs and systems.
The immune system (the body's natural defense against infection and disease) of most healthy people kills the bacteria without causing symptoms. Sometimes the immune system cannot kill bacteria, but can stop it from spreading in the body. In this case, no symptoms develop, but the bacteria remain in the body. This is called latent (hidden) tuberculosis.
Methods of transmission
- Airborne - through the sneezing, coughing of a patient with an open form of the disease, and even when drying out, the bacillus retains its pathogenicity.
- Alimentary – through the digestive tract. The infection enters the body due to poor hand hygiene or poorly washed and unprocessed food.
- Contact – the infection enters a person through the conjunctiva of the eyes, through kissing, sexual contact, through contact of contaminated objects with human blood, or the use of other people’s hygiene items.
Standards and detected deviations
Normally, there should be no mycobacteria in the body. Their presence is regarded as a positive result of the diagnosis of tuberculosis. A negative result indicates that the patient does not have this pathology. Some methods are nonspecific and do not have high diagnostic value. They are used to assess general condition. Bacteriological techniques are more specific and their positive results can be considered confirmation of the diagnosis. A negative result is a reason for repeat tests if there are clinical signs of the disease.
Types of tuberculosis
- Open form - the disease is clearly expressed, bacteria are easily detected in sputum and feces. The patient himself poses a danger to others, since the infection is transmitted by airborne droplets. Microbacteria can be found in sputum, urine, and feces.
- Closed form - not dangerous to others. Characterized by the difficulty of detecting infection in sputum. The most common tuberculosis is pulmonary tuberculosis, but this infection can also affect bones, joints, genitourinary system, intestines, peritoneum, meninges, central nervous system, peripheral lymph nodes, skin
Pneumoconiosis
The diagnosis is established if the patient worked in highly dusty conditions (in a mine, stone quarry, etc.). The process develops gradually without symptoms of intoxication characteristic of tuberculosis, but with signs of bronchitis. Decreased breathing due to emphysema and dry wheezing as a manifestation of bronchitis can be heard over the lungs.
The radiograph shows bilateral symmetrical focal shadows mainly in the mid-lateral sections. The lesions are clearly contoured against the background of fibrous deformation of the pulmonary pattern. Sometimes the lymph nodes are calcified at the root, more at the periphery, which creates an “eggshell” appearance. There is often a discrepancy between large changes on the radiograph and relatively minor clinical manifestations.
The first symptoms of tuberculosis
In the early stages, the disease is practically asymptomatic. As it develops, the patient's condition worsens, but no specific symptoms are observed. Increased fatigue, weakness, sudden weight loss for no apparent reason, a temperature of 37-38 ° C that does not subside for a long time, and night sweats appear. In children, the disease progresses faster than in adults.
The pulmonary form of tuberculosis is accompanied by a cough. Mild at first, it begins to progress over time. If your cough continues for more than three weeks, you should seek medical help immediately. The cough is initially dry, paroxysmal, especially at night and in the morning. Later, yellow-green sputum begins to be released, and at the cavity stage, hemoptysis is observed.
In the form of tuberculosis that affects the brain and its membranes, in addition to symptoms of general intoxication, sleep disturbances and headaches are observed, the intensity of which gradually increases.
Pneumonia
Pneumonia - bilateral focal pneumonia is manifested by radiological pulmonary dissemination syndrome. Its causative agents are staphylococci, streptococci, pneumococcus viruses, pneumocystis, legionella. Therefore, clinical symptoms are not always the same. Classic bacterial pneumonia begins acutely with symptoms of sore throat, pharyngitis, laryngitis, chills, and high body temperature. Clearly expressed bronchopulmonary syndrome: cough is dry, then wet, with auscultation - a lot of dry and wet wheezing, shortness of breath. With the same prevalence of the process in patients with tuberculosis, the general condition is lighter, auscultatory changes are scanty, there are no symptoms of catarrh of the upper respiratory tract. In the hemogram for pneumonia, high leukocytosis is noted (often more than 15 x 10 h / l) and: a significant shift of the formula to the left, increased ESR.
On the radiograph, there are foci of low intensity with unclear contours, the size of the shadow is mainly in the lower parts of the lungs, the apexes are not affected. In cases of abscess formation, cavities with a horizontal level of fluid are formed more often in the middle or lower parts of the lungs.
It is necessary to perform a bacteriological examination of sputum to isolate a possible pathogen and determine its sensitivity to antibiotics. At the same time, they are searching for MBT. Adequate antibiotic therapy gives a rapid clinical and radiological effect. Diagnostic criteria for nonspecific pneumonia:
- pronounced symptoms of intoxication, the general condition is more severe;
- Numerous wet and dry rales are heard over the site of the lesion;
- blood test - a significant increase in leukocytes, a shift of neutrophils to the left, a sharp increase in ESR;
- as a rule, nonspecific foci are in one lung, in the lower parts and in the hilar region, and the apices remain unchanged;
- there is no decay cavity, no foci of contamination;
- in sputum analysis forum MBT;
- nonspecific changes in inflammation resolve completely after 2-3 weeks from the start of treatment with nonspecific broad-spectrum antibiotics.
How is tuberculosis diagnosed?
To diagnose the disease, you must first consult with your primary care physician, who, if tuberculosis is suspected, will refer you to a phthisiatrician (tuberculosis specialist) for further diagnosis and treatment. Diagnosis will depend on the type of disease.
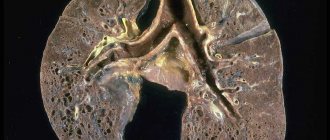
Diagnosis of pulmonary tuberculosis
An X-ray of the chest is required, which provides an image of the lungs. For pulmonary TB, the scan should show changes in the appearance of the lungs, such as scarring.
To confirm the diagnosis, samples of mucus and sputum are taken and analyzed under a microscope for the presence of tuberculosis bacteria.
Examination for extrapulmonary tuberculosis
- CT scan
- magnetic resonance imaging (MRI)
- ultrasound examination (ultrasound)
- blood tests
- Analysis of urine
- biopsy - a tissue sample is taken from the affected area to be tested for the presence of tuberculosis
Examination for latent tuberculosis
To prevent the disease, every person is required to undergo fluorography and an X-ray of the lungs at least once every two years.
Collection of material and preparation for research
To test urine for tuberculosis, a morning portion is used. It is necessary to toilet the external genitalia and not touch them to the reservoir for collecting material. The container must be sterile and dry. The collected biomaterial must be delivered to the laboratory as soon as possible, and must not be allowed to dry out or heat up. The day before the test, you need to give up foods such as blueberries, carrots, beets and other brightly colored vegetables and fruits. You should also limit your intake of diuretics, vitamins, and acetylsalicylic acid. Women should remember that urine tests are not taken during menstruation. A medium, intermediate portion of urine is given.
Blood donation occurs on an empty stomach, since food intake can distort the results of the study. It is worth consulting with your doctor about discontinuing certain medications. The day before you should not consume coffee, alcohol, or tobacco. Blood collection occurs under sterile conditions, in compliance with the rules for collecting material. Some studies require capillary blood, and some require venous blood.
Sputum is collected on an empty stomach, following the basic rules. The material must be coughed out so that mucus from the mouth or nasopharynx does not get into the container. A special spittoon made of dark glass with a tight lid is used. The sputum should not become chapped or dry out.
No special preparation is required for instrumental research methods. The exception is the use of a contrast agent. Renal function should be assessed before use. Most radiopaque substances are excreted by this organ, and the doctor must be sure that the excretory system can withstand this load.
How to treat tuberculosis?
Treatment of the pathology depends on its type, but most often a course of antibiotics is prescribed. Tuberculosis is a dangerous disease that requires immediate treatment. This allows the person to return to their normal lifestyle.
Antibacterial therapy is aimed at suppressing the proliferation of the tuberculosis pathogen.
Treatment takes place in 2 phases: in the first, several drugs are used at once to reduce the population of microbacteria, the second phase is maintenance therapy. Antibiotics stop the proliferation of bacteria and their release into the environment, the inflammatory process.
After taking such potent medications, a person needs additional supportive therapy that will strengthen the body and reduce the toxic effect. For this, immunostimulants (restore liver function), sorbents (remove toxic breakdown products of chemotherapy drugs) and vitamin complexes are prescribed.
After taking the drugs for two weeks, most people are no longer contagious and feel much better. However, it is very important to continue taking your medications as directed by your doctor and complete your entire course of antibiotics.
Carcinomatosis
These malignant tumors of the mammary, thyroid glands, bones, genitals, adrenal glands, and lungs can metastasize to the lungs with the formation of radiological pulmonary dissemination syndrome. According to tuberculosis, in the initial stages, patients are worried about a dry cough, weakness, loss of appetite, and elevated body temperature. Subsequently, the patient’s condition worsens: shortness of breath increases, a dry cough becomes hysterical, and chest pain is possible. Fine bubbling or dry wheezing and harsh breathing may be heard over the lungs.
The hemogram for tuberculosis and carcinomatosis is similar, but anemia and significantly increased ESR are more characteristic of carcinomatosis. The Mantoux test for carcinomatosis is often negative. Bronchoscopy is performed, although its positive results and tumor cells are often found in the contents of the bronchi if metastasis is caused by lung cancer.
With carcinomatosis, radiographs reveal foci in both lungs that can be of varying sizes, but more often monomorphic and clearly defined than with tuberculosis. Mostly their number and size increase in the apicocaudal direction. To establish a diagnosis, information about previous surgery and searches for tumors in other organs are important.
Diagnostic criteria for carcinomatosis:
- history of surgery or other treatment for the tumor;
- detection of a tumor in another organ;
- low-symptomatic onset (possible dry cough, weakness, and sometimes fever);
- The patient's condition is steadily deteriorating - shortness of breath, chest pain, and dry cough appear and constantly progress. Sometimes a slight increase in body temperature is detected;
- X-ray: with carcinomatosis, X-rays reveal lesions in both lungs that can be of varying sizes, but more often monomorphic;
- the lesions are clearly defined and localized mainly in the lower parts of the lungs, closer to the roots;
- the pulmonary pattern against the background of the lesions is not visible;
- The hemogram for tuberculosis and carcinomatosis is similar, but anemia and a significant increase in ESR are more typical for carcinomatosis.
Other treatments for tuberculosis
Surgery
The goal of therapy is the elimination of tuberculosis foci in the lungs with ineffective treatment, elimination of the consequences of pulmonary tuberculosis, and elimination of organ damage. All this is necessary to prevent the recurrence of the disease and to exclude the occurrence of complications.
Indications for surgical intervention can be any form of respiratory tuberculosis, especially in the case of complications that threaten a person’s life.
Chemotherapy
used with an optimal combination of anti-tuberculosis drugs aimed at eliminating mycobacteria and suppressing their reproduction. The duration of such treatment can reach up to a year - it all depends on the form and stage of development of the pathology.
If chemotherapy is stopped early, exacerbation or complications of tuberculosis may occur. Therefore, it is important to follow all doctor's recommendations. And the doctor, for his part, must draw up a detailed treatment plan and make adjustments throughout the entire therapy.
A patient who is indicated for chemotherapy as a treatment for tuberculosis must be prepared for the negative consequences of such an aggressive method. Side effects on the action of medications often occur. There are 2 types of adverse reactions: toxic and allergic. Dysbacteriosis may also occur.
The doctor may prescribe outpatient treatment if the disease is detected at an early stage and there is no infection to others. In this case, you need to regularly visit your doctor and undergo diagnostics. Most often, the patient is transferred to outpatient treatment after observation in a hospital and undergoing an extensive course of therapy in a tuberculosis clinic. At this time, the patient is no longer contagious.
Bronchiolitis
This is a common lesion of very small bronchi and bronchioles, which causes the development of severe obstruction and, as a consequence, respiratory failure. More often, the disease occurs in the spring and winter during the flu or ARVI.
Diagnostic criteria for bronchiolitis:
- the development of bronchiolitis is preceded by a nonspecific disease or influenza;
- the temperature after 4-5 days with bronchiolitis drops to normal levels;
- in patients, multiple fine bubbling and dry rales are heard;
- The radiograph shows small foci, areas of infiltrative shadows (foci are fused together), which are located in the hilar and lower parts of the lungs;
- changes in physical and radiographic examination quickly normalize.
Manifestations of infection of the upper respiratory organs
Signs of infection may appear in different respiratory organs. To recognize the disease in time, you should know its symptoms. At the beginning of the development of tuberculosis, the patient develops dryness and soreness in the nose and oropharynx, and he cannot swallow food normally. In addition, there is severe shortness of breath and a hoarse cough.
After some time, severe chills appear, body temperature rises, and breathing becomes difficult. After another period, the voice changes and hemoptysis begins. At the same time, patients lose a lot of weight because they cannot eat properly due to pain.
Tuberculosis of the larynx is manifested by improper mobility of the vocal cords and leads to hoarseness, breathing problems, soreness, and changes in voice.
When the throat is affected, there is severe pain, a sensation of a foreign body in the throat, increased salivation, swelling, rashes and redness of the pharynx mucosa. If we are talking about nasal tuberculosis, then all the symptoms are very similar to ordinary sinusitis: itching, burning, crusts in the nose, frequent bleeding, congestion, pain, the presence of mucopurulent discharge.
Symptoms may be constant, come and go, or progress slowly (sluggish tuberculosis). Rapid progress is also common, when a person can die from the manifestations of the disease in a few weeks.
Congestion in the lungs
Congestion in the lungs develops with left ventricular insufficiency, which happens with decompensated mitral heart defects, hypertension, coronary heart disease, post-infarction cardiosclerosis, etc. Blood stagnation: in the pulmonary circulation can cause the formation of bilateral focal shadows in the lungs, similar to shadows with disseminated tuberculosis.
Diagnostic difficulties arise in the case of gradual, chronic development of this process, especially if the patient also has post-tuberculosis changes in the lungs. But, unlike disseminated tuberculosis, with congestive phenomena in the lungs there are no signs of intoxication, progressive shortness of breath, dry, and sometimes (with congestive bronchitis, wet) cough predominates. From the anamnesis, you can learn about the patient’s treatment in the past for rheumatism and cardiac pathology. You should pay attention to changes in the configuration of the heart, murmurs, rhythm disturbances, and pathological changes on the ECG. If signs of right ventricular failure are added, edema and an enlarged liver are detected.
On the radiograph, in addition to changes in the configuration and size of the heart, symmetrically located focal shadows (from miliary to macrofocal) are visible, mainly in the lower and hilar areas of the lungs. The roots are expanded, “stagnant”. There may be an accumulation of transudate in the pleural cavity, reminiscent of disseminated pulmonary tuberculosis, complicated by pleurisy.
The clinical effect and disappearance of focal shadows occurs after treatment with diuretics, vasodilators, and cardiac glycosides.
Diagnostic criteria for congestion in the lungs:
- medical history data about rheumatism and other heart diseases;
- progressive shortness of breath, cough at normal body temperature;
- changes in the size and configuration of the heart, rhythm disturbances, heart murmurs, sometimes swelling, enlarged liver;
- on the radiograph: lesions mainly in the lower and basal areas, extended roots;
- clinical and radiological effect under the influence of diuretics, cardiac glycosides, etc.
It should be taken into account that pulmonary tuberculosis can develop in persons with cardiac pathology, therefore, in each case, a detailed examination and multiple searches for MBT are required.
Silicosis
This is an occupational disease that occurs due to damage to the lungs by dust from very small particles of mineral rocks. Most often, pneumoconiosis is where tuberculosis joins it.
Diagnostic criteria for silicosis:
- professional history;
- the clinical picture is dominated by symptoms of damage to the bronchi and lungs (cough with sputum, chest pain, increasing shortness of breath);
- X-ray - pneumosclerosis, emphysema, mainly of the basal parts;
- the presence of foci (silicotic nodules), 3-5 mm in size with clearly defined contours, their number increases downwards;
- the roots of the lungs are expanded and significantly compacted;
- in stages II-III, numerous scattered foci appear, in some places merging into large conglomerates, bullous emphysema, compaction of the interparticle and costal pleura
- antimycobacterial therapy does not have a positive result.
Diagnostic criteria for silicosis and silicotuberculosis
| Silicosis | Silicotuberculosis |
| Complaints | |
| Cough, shortness of breath, chest pain | Additionally - symptoms of intoxication |
| Objective examination results | |
| Signs of bronchitis, emphysema (dry wheezing, boxy percussion sound above the lower parts of the lungs) | In addition, local moist rales, in the presence of infiltrates - dullness of percussion sound over the upper parts of the lungs |
| Laboratory data | |
| Normal hemogram, MBT- | Possible leukocytosis, shift to the left, lymphopenia, increased ESR, MBT + |
| Changes on the X-ray | |
| Deformation of the pulmonary pattern, nodular shadows in the mediolateral sections, “chopped off” roots | Against this background, the appearance of new polymorphic foci, infiltrates or decay cavities, especially in the upper parts of the lungs |
Cystic fibrosis (ecrinosis, cystic fibrosis of the pancreas - Fanconi syndrome)
This is a hereditary disease characterized by systemic damage to the glands (pancreas, intestines, respiratory tract, as well as sweat, lacrimal, salivary glands) due to blockage of their excretory ducts with a viscous secretion. A characteristic sign of cystic fibrosis is an increase in the viscosity of the secretions of glands that still form mucus.
Diagnostic criteria for cystic fibrosis:
- the presence in the anamnesis of patients with lung damage of repeated bronchitis with a severe course, difficult to treat, as well as pneumonia (usually bilateral) with the development of polysegmental atelectasis with a long course;
- a typical complaint is an unbearable cough with viscous sputum, in connection with which the cough may end in vomiting;
- a significant proportion of patients (up to 80%) experience complaints caused by damage to the digestive system: alternating diarrhea and constipation, rumbling in the abdomen, poor fat tolerance, pain in the right hypochondrium due to concomitant cholecystitis;
- Patients with cystic fibrosis are characterized by a chronic runny nose;
- Various wet and dry rales are heard in the lungs as a result of obstruction of the bronchi with mucus and an infectious process. In the upper parts of the lungs there may be weakened breathing due to emphysema;
- X-ray changes should be diffuse, but the upper lobe of the right lung is more often affected. The pulmonary pattern is strengthened and deformed, with rough mesh-linear structures. In some cases, lobular, subsegmental or segmental atelectasis are observed. In the presence of emphysema, an increase in the transparency of the pulmonary fields is detected, mainly in the upper sections. Pneumonic infiltration often appears;
- bronchological examination reveals typical changes: “breaks” of the bronchi, fragmented filling, uneven contours. More than a third of patients are diagnosed with bronchiectasis, which is localized mainly in the lower parts of the lungs;
- The study of sweat electrolytes (sweat test) using the Gibson Cook method is extremely important in the diagnosis and differential diagnosis of cystic fibrosis. A chloride content of more than 60 mmol/l and a sodium content of 70 mmol/l is considered absolute evidence of the presence of the disease.
Sarcoidosis (Besnier-Beck-Schaumann disease)
Stage II sarcoidosis, like disseminated tuberculosis, most often begins asymptomatically or with minimal symptoms with a dry cough, slight shortness of breath, and chest pain. Auscultatory changes, even with a significant prevalence of the process, are scanty. Possible simultaneous damage to the eyes, salivary glands, skin, heart and other organs, and an increase in certain groups of peripheral lymph nodes.
Tuberculin tests are predominantly negative or weakly positive. The hemogram shows leukopenia, lymphopenia, and a possible slight increase in ESR. The x-ray shows multiple foci and enlarged lymph nodes, usually of the bronchopulmonary group, which happens with disseminated tuberculosis. Unlike tuberculosis, decay cavities do not form.
Diagnostic criteria for stage II sarcoidosis:
- the presence of Löfgren's syndrome (temperature 38-39 ° C, joint pain);
- localization of foci mainly in the lower and middle parts of the lungs;
- the lesions are of the same type, their number decreases in the direction from the roots of the lungs;
- X-ray changes in the pulmonary form of sarcoidosis without visible enlargement of the intrathoracic lymph nodes are characterized by the presence of focal shadows and interstitial compactions in the lungs, more often in the middle sections; with enlarged lymph nodes, a uniform shadow is noted, sharply demarcated from the surrounding tissue;
- In sarcoidosis, hypercalcemia and increased activity of angiotensin-converting enzyme are often observed. If the corresponding antigen is present, the Kveim test is performed;
- during bronchoscopic examination, a delicate vascular network is found on the bronchial mucosa, sarcoid plaques, and signs of atrophic bronchitis;
- the use of antimycobacterial drugs for treatment is ineffective; positive changes come from the administration of corticosteroids.