Hemoglobin levels in children vary depending on age and differ from adults.
In children from 6 months to 5 years, anemia is considered to be a decrease in hemoglobin level below 110 g/l, from 5 to 11 years - below 115 g/l; at older ages, the hemoglobin level approaches the norm for adults. Before the age of 6 months, children sometimes experience so-called physiological anemia of newborns, while the hemoglobin level can decrease to 90 g/l, and in the absence of other causes, this condition does not require treatment.
Anemia can be critical to a growing and developing child's body. With low levels of red blood cells and hemoglobin, organs and tissues receive insufficient oxygen. If this condition continues for a long time, the physical, psychomotor and mental development of the child is disrupted. That is why it is important not only timely diagnosis and treatment of anemia, but also its prevention in risk groups.
About the disease
Anemia is a very common pediatric problem.
WHO data indicate that more than 47% of preschool children and more than 25% of school-age children suffer from anemia. The main function of the red blood cell is the transport of oxygen molecules. Hemoglobin, a special protein containing iron, delivers oxygen to organs and tissues. Normal hemoglobin levels in g/l (grams per liter) depend on age:
- in newborns – from 180 to 240;
- from 1 to 6 months – from 115 to 175;
- from 6 months to 5 years – from 110 to 140;
- from 5 to 12 years – from 110 to 145;
- from 12 to 15 years – from 115 to 150.
Anemia in children develops for many reasons, and rapid body growth predisposes to this.
In children, erythropoiesis (the formation of red blood cells) is accelerated; the number of cells and the volume of circulating blood must constantly increase to keep up with growth. This process is often disrupted due to age-related immaturity of hematopoiesis. In order for hematopoiesis to proceed without failure, the following substances must be uninterruptedly supplied and absorbed in full into the child’s body:
- iron;
- proteins of animal and vegetable origin;
- vitamins;
- microelements.
The supply and absorption of these molecules is easily disrupted by dietary errors, infections, and various types of intoxication.
Children under 6 months of age have a neonatal iron reserve. Subsequently, this reserve is depleted, and if the supply of nutrients from food and the absorption of nutrients in the intestine are disrupted, the preconditions are created for the development of anemia. With a prolonged decrease in hemoglobin levels, the child develops hypoxia - oxygen deficiency, as a result of which all organs and tissues suffer. Due to anemia, children may lag behind in physical and intellectual development, and they are more likely than healthy peers to develop chronic diseases and complications.
Based on their occurrence, the following groups of anemia are distinguished:
- due to bleeding - posthemorrhagic;
- due to disruption of the hematopoietic process - iron deficiency, iron-saturated, megaloblastic (due to deficiency of folic acid and B12), aplastic (due to bone marrow diseases);
- due to the predominance of the process of destruction of red blood cells - hemolytic.
Iron deficiency anemia in infants and young children
Anemia and anemic syndrome, caused by many causes, can be mentioned among the most common pathological conditions that general pediatricians have to deal with every day. This group includes various diseases and pathological conditions characterized by a decrease in the content of hemoglobin and/or red blood cells per unit volume of blood, leading to disruption of the oxygen supply to tissues. The following laboratory criteria for anemia are applied (N.P. Shabalov, 2003). Depending on the age of the children, the hemoglobin level is:
- 0–1 day of life - < 145 g/l;
- 1–14 days of life - < 130 g/l;
- 14–28 days of life - < 120 g/l;
- 1 month - 6 years - < 110 g/l.
Of all anemias, the most common is iron deficiency (IDA), which accounts for approximately 80% of all anemias. According to the World Health Organization (WHO), more than 500 thousand people worldwide suffer from IDA. The prevalence of IDA in children in Russia and developed European countries is: about 50% in young children; more than 20% - in older children.
IDA is a clinical and hematological syndrome characterized by impaired hemoglobin synthesis as a result of iron deficiency, developing against the background of various pathological (physiological) processes, and manifested by signs of anemia and sideropenia.
Iron is one of the main microelements in the human body. Normally, the adult body contains 3–5 g of iron in bound form. 70% of the total amount of iron is part of hemoproteins. The iron in these compounds is bound to porphyrin. The main representative of this group is hemoglobin (58% iron); Iron is also contained in myoglobin (8%), cytochromes, peroxidases, catalases - up to 4%. Iron is also part of non-heme enzymes (xanthine oxidase, nicotinamide adenine dinucleotide (NADH) dehydrogenase, aconitase, localized in mitochondria); transport form of iron (transferrin, lactoferrin). Iron reserves in the body exist in two forms: in the form of ferritin (up to 70%) and hemosiderin (up to 30%). The peculiarity of iron distribution in young children is that they have a higher iron content in erythroid cells and less iron in muscle tissue.
Iron absorption occurs predominantly in the duodenum and proximal jejunum. The daily diet usually contains about 5–20 mg of iron, and only about 1–2 mg per day is absorbed. The degree of iron absorption depends both on its amount in food consumed and bioavailability, and on the state of the gastrointestinal tract (GIT).
Iron is more easily absorbed in heme (meat products) - 9–22%. Absorption of non-heme iron is determined by diet and gastrointestinal secretion patterns.
Iron absorption is especially active from breast milk, although its content is low - only 1.5 mg per liter; The bioavailability of iron in breast milk is up to 60%. This is facilitated by the special form in which it is presented - in the form of the iron-containing protein lactoferrin. In the lactoferrin molecule, two active binding sites for Fe3+ ions are identified. Lactoferrin is found in breast milk in saturated and unsaturated forms. The ratio of lactoferrin forms varies depending on the lactation period. During the first 1–3 months of life, the saturated iron transport form of lactoferrin predominates. The presence of specific receptors for lactoferrin on the epithelial cells of the intestinal mucosa promotes the adhesion of lactoferrin to them and its more complete utilization. In addition, lactoferrin, by binding excess iron that is not absorbed in the intestine, deprives the opportunistic microflora of the microelement necessary for its life and triggers nonspecific bactericidal mechanisms. It has been established that the bactericidal function of immunoglobulin A is realized only in the presence of lactoferrin.
Physiological losses of iron in urine, sweat, feces, through the skin, hair and nails do not depend on gender and amount to 1-2 mg per day, in women during menstruation - 2-3 mg per day. In children, iron loss is 0.1–0.3 mg per day, increasing to 0.5–1.0 mg per day in adolescents.
The daily requirement of a child's body for iron is 0.5–1.2 mg per day. In young children, due to rapid growth and development, there is an increased need for iron. During this period of life, iron reserves are quickly depleted due to increased consumption from the depot: in premature infants by the 3rd month, in full-term infants by the 5th–6th month of life. To ensure the normal development of a child, the daily diet of a newborn should contain 1.5 mg of iron, and for a child 1–3 years old - at least 10 mg.
Iron deficiency in children leads to an increase in infectious diseases of the respiratory system and gastrointestinal tract. Iron is necessary for the normal functioning of brain structures; if it is insufficient, the child’s neuropsychic development is disrupted. It has been established that in children who had iron deficiency anemia in infancy, at the age of 3–4 years, disturbances in the transmission of nerve impulses from the centers of the brain to the organs of hearing and vision are determined due to impaired myelination and, as a consequence, impaired nerve conduction.
The causes of iron deficiency in children are very diverse. The main cause of IDA in newborns is considered to be the presence of IDA or hidden iron deficiency in the mother during pregnancy. Antenatal causes also include complicated pregnancy, impaired uteroplacental circulation, fetomaternal and fetoplacental bleeding, fetal transfusion syndrome in multiple pregnancies. Intrapartum causes of iron deficiency are: fetoplacental transfusion, premature or late ligation of the umbilical cord, intrapartum bleeding due to traumatic obstetric care or abnormal development of the placenta or umbilical cord. Among the postnatal causes of sideropenic conditions, the first place is taken by insufficient intake of iron from food. In this case, newborns who are bottle-fed with unadapted milk formulas, cow's and goat's milk suffer the most. Other postnatal causes of IDA are: increased body need for iron; iron losses exceeding physiological ones; gastrointestinal diseases, malabsorption syndrome; deficiency of iron stores at birth; anatomical congenital anomalies (Meckel's diverticulum, intestinal polyposis); consumption of foods that inhibit iron absorption.
Premature children and children born with a very large weight, children with a lymphatic-hypoplastic type of constitution are always at risk.
In children of the first year of life, iron deficiency is most often caused by an unbalanced diet, in particular, feeding exclusively with milk, vegetarianism, and insufficient consumption of meat products.
Bleeding of various etiologies can lead to sideropenia. The source of this may be: hiatal hernia, esophageal varices, gastrointestinal ulcers, tumors, diverticula, ulcerative colitis, hemorrhoids, as well as bleeding from the genitourinary tract and respiratory tract. Taking certain medications, such as nonsteroidal anti-inflammatory drugs, salicylates, coumarins, and glucocorticosteroids, can also lead to iron loss. Iron deficiency always accompanies diseases accompanied by impaired intestinal absorption (enteritis, Crohn's disease, parasitic infestations, etc.). Intestinal dysbiosis also interferes with normal digestion of food and thereby reduces the body's ability to absorb iron. In addition, there may be a disruption in iron transport due to insufficient activity and decreased transferrin levels in the body.
It is extremely important to recognize the cause of the development of IDA in each specific case. Focus on nosological diagnosis is necessary, since in most cases, when treating anemia, it is possible to influence the underlying pathological process.
IDA manifests itself with general symptoms. One of the main and visible signs is pallor of the skin, mucous membranes, and conjunctiva of the eyes. Noteworthy are general lethargy, moodiness, tearfulness, easy excitability of children, decreased overall body tone, sweating, lack or decreased appetite, shallow sleep, regurgitation, vomiting after feeding, decreased visual acuity. Changes in the muscular system are detected: the child has difficulty overcoming physical activity, weakness and fatigue are noted. In children of the first year of life, regression of motor skills may be observed.
In the second half of life and in children older than one year, signs of damage to epithelial tissue are observed - roughness, dry skin, angular stomatitis, painful cracks in the corners of the mouth, glossitis or atrophy of the oral mucosa, fragility and dullness of hair, hair loss, dullness and brittleness of nails, tooth decay (caries), retardation in physical and psychomotor development.
Depending on the severity of the disease, symptoms of damage to organs and systems are identified: cardiovascular - in the form of a functional heart murmur, tachycardia; nervous system - in the form of headaches, dizziness, fainting, orthostatic collapse. Possible increase in the size of the liver and spleen. From the gastrointestinal tract, there is difficulty swallowing, bloating, diarrhea, constipation, perversion of taste - the desire to eat clay, earth.
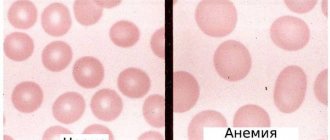
The diagnosis of IDA is made based on the clinical picture, laboratory signs of anemia and iron deficiency in the body: hypochromic (color index < 0.85) anemia of varying severity, hypochromia of erythrocytes, decrease in the average hemoglobin concentration in erythrocytes (less than 24 pg), microcytosis and poikilocytosis of erythrocytes (in peripheral blood smear); decrease in the number of sideroblasts in bone marrow aspirate; decrease in iron content in blood serum (<12.5 µmol/l); an increase in the total iron-binding capacity of serum (TIBC) of more than 85 µmol/l (an indicator of “starvation”); an increase in the level of transferrin in the blood serum, with a decrease in its saturation with iron (less than 15%); decreased serum ferritin levels (<15 µg/L).
Treatment of IDA
Treatment of IDA in young children should be comprehensive and based on four principles: normalization of the child’s regimen and nutrition; possible correction of the cause of iron deficiency; prescription of iron supplements; concomitant therapy.
The most important factor in correcting iron deficiency is a balanced diet, and primarily breastfeeding. Breast milk not only contains iron in a highly bioavailable form, but also increases the absorption of iron from other foods consumed at the same time. However, intense metabolic processes in infants lead to the fact that by the 5th–6th month of life, antenatal iron reserves are depleted even in children with a good perinatal history and babies fed with breast milk.
Among other foods, the greatest amount of iron is found in pork liver, beef tongue, veal kidneys, egg yolk, oysters, beans, sesame seeds, seaweed, wheat bran, buckwheat, pistachios, chick peas, peaches, oatmeal, spinach, hazelnuts and etc. (table).
Iron absorption is inhibited by tannins contained in tea, carbonates, oxalates, phosphates, ethylenediaminetetraacetic acid used as a preservative, antacids, and tetracyclines. Ascorbic, citric, succinic and malic acids, fructose, cysteine, sorbitol, nicotinamide enhance iron absorption.
Long walks in the fresh air, normalization of sleep, a favorable psychological climate, prevention of acute respiratory viral infections (ARVI), and limitation of physical activity are necessary. The child's diet should be balanced and include foods rich in iron and substances that enhance its absorption in the intestines. Children suffering from IDA need to be introduced to complementary foods 2–4 weeks earlier than healthy ones. It is advisable to start introducing meat complementary foods at 6 months. You should avoid introducing cereals such as semolina, rice, and bearberry into your child’s diet, giving preference to buckwheat, barley, and millet.
However, these measures are insufficient and do not lead to the cure of IDA, so the basis of therapy is iron supplements. The main ones used orally include: ferric iron compounds - hydroxide-polymaltose complex (iron polymaltose), maltofer, maltofer foul, ferrum lek and iron-protein complex (iron protein succinylate) - ferlatum; divalent iron compounds - actiferrin, ferroplex, tardiferon, hemofer, totema, ferrous fumarate, ferronate.
Therapy should be started with drugs for oral administration and only if they are poorly tolerated (nausea, vomiting, diarrhea), malabsorption syndrome, resection of the small intestine, etc. - iron supplements are prescribed parenterally. When prescribing oral forms, preference should be given to nonionic iron compounds - protein (ferlatum) and hydroxide-polymaltose Fe3+ complexes (maltofer, maltofer foul, ferrum lek). These compounds have a large molecular weight, which makes it difficult for them to diffuse across the intestinal mucosal membrane. They enter the blood from the intestines as a result of active absorption. This explains the impossibility of overdosing on drugs, unlike iron salt compounds, the absorption of which occurs along a concentration gradient. There is no interaction between them and food components and medications, which allows the use of non-ionic iron compounds without disturbing the diet and treatment of concomitant pathologies. Their use significantly reduces the incidence of side effects usually observed when prescribing oral iron supplements (nausea, vomiting, diarrhea, constipation, etc.). In addition, in young children, the dosage form of the drug is of great importance. At this age, it is convenient to use drops and syrups, which also provides the possibility of precise dosing of drugs and does not cause a negative attitude from the child.
When prescribing any iron supplements, it is necessary to calculate the individual need for it for each patient, based on the fact that the optimal daily dose of elemental iron is 4–6 mg/kg. The average daily dose of iron in the treatment of IDA is 5 mg/kg. The use of higher doses does not make sense, since the amount of iron absorption does not increase.
The use of parenteral iron supplements is indicated to quickly achieve an effect in severe anemia; gastrointestinal pathology combined with malabsorption; nonspecific ulcerative colitis; chronic enterocolitis; with severe intolerance to oral forms of drugs. Today in the Russian Federation, only one drug is approved for intravenous administration - venofer (iron sucrose), while ferrum lek can be used for intramuscular administration.
It must be remembered that in young children, iron deficiency is never isolated and is often combined with a deficiency of vitamins C, B12, B6, PP, A, E, folic acid, zinc, copper, etc. This is due to the fact that nutritional deficiency and impaired intestinal absorption, leading to iron deficiency, also affects saturation with these micronutrients. Therefore, it is necessary to include multivitamin preparations in complex therapy for IDA.
The effectiveness of IDA therapy can be judged after 7–10 days by an increase in reticulocytes by 2 times compared to the initial number (the so-called reticulocyte crisis). The increase in hemoglobin is also assessed, which should be 10 g/l or more per week. Accordingly, achievement of the target hemoglobin level is observed on average 3–5 weeks from the start of therapy, depending on the severity of anemia. However, treatment with iron supplements should be carried out in sufficient doses and for a long time (at least 3 months) even after normalization of hemoglobin levels in order to replenish iron reserves in the depot.
If within 3-4 weeks there is no significant improvement in hemoglobin levels, then it is necessary to find out why the treatment was ineffective. Most often we are talking about: an inadequate dose of iron supplement; ongoing or unknown blood loss; the presence of chronic inflammatory diseases or neoplasms; concomitant vitamin B12 deficiency; incorrect diagnosis; helminthic infestation and other parasitic infections.
Contraindications to the use of iron supplements are:
- lack of laboratory confirmation of iron deficiency;
- sideroachrestic anemia;
- hemolytic anemia;
- hemosiderosis and hemochromatosis;
- infection caused by gram-negative flora (enterobacteria, Pseudomonas aeruginosa, Klebsiella).
With the development of severe anemia, accompanied by inhibition of erythropoiesis and a decrease in erythropoietin production, the administration of recombinant human erythropoietin (rhEPO) preparations is indicated. The use of rhEPO is of particular importance in the development of early anemia of prematurity, which develops in the second month of life and occurs, according to various authors, in 20–90% of cases. The administration of rhEPO drugs (Recormon, Eprex, Epocrine) leads to a sharp activation of erythropoiesis and, as a consequence, to a significant increase in iron requirements.
Therefore, the use of rhEPO is an indication for the administration of iron supplements, usually parenteral. Currently, a- and b-epoetins are approved for use in the Russian Federation and are included in the list of additional medicinal products. Prescribing rhEPO allows, in most cases, to avoid blood transfusions, in which there is a high probability of complications (transfusion reactions, sensitization, etc.). The preferred route of administration of rhEPO preparations, especially in early childhood, is subcutaneous. The subcutaneous route of administration is safer and more economical, since smaller doses are required to achieve an effect than with intravenous administration. Until recently, in the countries of the European Union and in the Russian Federation, mainly β-erythropoietins were used for the treatment of hyporegenerative anemia in children, which, when administered subcutaneously, did not cause significant adverse reactions, unlike a-erythropoietins, when administered subcutaneously, there was a high risk of developing red cell aplasia. The most widely used drug among β-erythropoietins is Recormon (F. Hoffmann-La Roche), which is easy to use and leads to a rapid increase in the level of erythrocytes and reticulocytes without affecting leukopoiesis, increases the level of hemoglobin, as well as the rate of incorporation of iron into cells.
Since 2004, European countries have allowed subcutaneous administration of a-erythropoietins, among which in our country the most commonly used are Eprex (Jansen-Silag) and Epocrine (Sotex-GosNII OCHB).
The goal of rhEPO treatment is to achieve hematocrit levels of 30–35% and eliminate the need for blood transfusions. The target hemoglobin concentration values may vary depending on the days and months of the child’s life, but cannot be lower than 100–110 g/l. Depending on the dose, target hemoglobin concentrations and hematocrit are achieved after approximately 8–16 weeks of rhEPO treatment.
To prevent iron deficiency anemia, rhEPO is prescribed to premature newborns born weighing 750–1500 g before the 34th week of pregnancy.
Treatment with erythropoietin should begin as early as possible and continue for 6 weeks. The drug Recormon is administered subcutaneously at a dose of 250 IU/kg 3 times a week. However, it must be taken into account that the younger the child is, the higher doses of erythropoietin he requires, so the dose can be increased.
As mentioned above, rhEPO therapy leads to a sharp increase in iron intake, therefore, in most cases, especially in premature infants, along with an increase in hematocrit, serum ferritin levels decrease. Rapid depletion of iron reserves in the body can lead to IDA. Therefore, all patients receiving rhEPO therapy are prescribed iron supplements. Therapy with iron supplements should continue until serum ferritin levels are normalized (at least 100 mcg/ml) and transferrin saturation (at least 20%). If serum ferritin concentration remains persistently below 100 mcg/ml or there are other signs of iron deficiency, the dose of iron should be increased, including the use of parenteral drugs.
Prevention of IDA in young children includes: antenatal (correct regimen and nutrition of the pregnant woman, timely detection and treatment of anemia in the pregnant woman, preventive administration of iron supplements to women at risk for developing IDA); postnatal (observance of hygienic living conditions for the child, long-term breastfeeding and timely introduction of complementary foods, adequate choice of formula for children on mixed and artificial feeding, prevention of the development of rickets, malnutrition and ARVI in the child). The following people need prophylactic administration of iron supplements:
- women of reproductive age suffering from heavy and prolonged menstrual bleeding;
- regular donors;
- pregnant women, especially repeat pregnancies following a short interval;
- women with iron deficiency during lactation.
Preventive administration of iron supplements is indicated for children at risk for developing IDA:
- premature babies (from 2 months of age);
- children from multiple pregnancies, complicated pregnancies and childbirths;
- large children with high rates of weight gain and height;
- children with constitutional anomalies;
- suffering from atopic diseases;
- those who are artificially fed with unadapted formulas;
- with chronic diseases;
- after blood loss and surgical interventions;
- with malabsorption syndrome.
The dose of iron prescribed for preventive purposes depends on the degree of prematurity of the child:
- for children with birth weight less than 1000 g - 4 mg Fe / kg / day;
- for children with birth weight from 1000 to 1500 g - 3 mg Fe/kg/day;
- for children with birth weight from 1500 to 3000 g - 2 mg Fe/kg/day.
The significance of the problem of IDA in young children is due to its high prevalence in the population and its frequent development in various diseases, which requires constant vigilance among doctors of all specialties. Nevertheless, at the present stage, the doctor’s arsenal has enough diagnostic and therapeutic capabilities for early detection and timely correction of sideropenic conditions.
Literature
- Anemia in children / ed. V. I. Kalinicheva. L.: Medicine, 1983. 360 p.
- Anemia in children: diagnosis and treatment / ed. A. G. Rumyantseva, Yu. N. Tokareva. M., 2000. 128 p.
- Arkadyeva G.V. Diagnosis and treatment of iron deficiency anemia. M., 1999. 59 p.
- Beloshevsky V. A. Iron deficiency in adults, children and pregnant women. Voronezh, 2000. 121 p.
- Borisova I.P., Skobin V.B., Pavlov A.D. Early administration of recombinant erythropoietin in premature infants/7th National Congress “Man and Medicine”. M., 2000. P. 125.
- Vakhrameeva S.N., Denisova S.N. Latent form of iron deficiency anemia in pregnant women and the health status of their children // Russian Bulletin of Perinatology and Pediatrics. 1996. No. 3. pp. 26–29.
- Dvoretsky L. I., Vorobyov P. A. Differential diagnosis and treatment for anemic syndrome. M.: Newdiamed, 1994. 24 p.
- Dvoretsky L.I. Iron deficiency anemia//Russian Medical Journal. 1997. No. 19. pp. 1234–1242.
- Idelson L.I. Hypochromic anemia. M.: Medicine, 1981. 190 p.
- Kazakova L. M., Makrushin I. M. Immunity in iron deficiency // Pediatrics. 1992. No. 10–12. pp. 54–59.
- Kazyukova T.V., Samsygina G.A., Levina A.A. Iron deficiency in children: problems and solutions//Consilium medicum. 2002. pp. 17–19.
- Malakhovsky Yu. E., Manerov F. K., Sarycheva E. G. Mild form of iron deficiency anemia and latent iron deficiency are borderline conditions in children of the first two years of life // Pediatrics. 1988. No. 3. pp. 27–34.
- Papayan A.V., Zhukova L.Yu. Anemia in children: a guide for doctors. St. Petersburg: Peter, 2001. 382 p.
- Prigozhina T. A. Efficacy of recombinant erythropoietin in the complex prevention and treatment of early anemia of prematurity: abstract. dis. ...cand. honey. Sci. M., 2001. 19 p.
- Rumyantsev A. G., Morshchakova E. F. Pavlov A. D. Erythropoietin. Biological properties. Age-related regulation of erythropoiesis. Clinical application. M., 2002. S. 137–144; 266–270.
- Rumyantsev A. G., Morshchakova E. F., Pavlov A. D. Erythropoietin in the diagnosis, prevention and treatment of anemia. M., 2003. 568 p.
- Sergeeva A. I., Sultanova K. F., Levina A. A. et al. Indicators of iron metabolism in pregnant women and young children // Hematology and Transfusiology. 1993. No. 9–10. pp. 30–33.
- Tetyukhina L.N., Kazakova L.M. Prevention of iron deficiency as a measure to reduce morbidity in children // Pediatrics. 1987. No. 4. pp. 72–73.
- Dallman PR, Looker AC, Johnson CL et al. Iron Nutrition in Health and Disease. Eds. Hallberg L., Asp N. G. Libbey; London. 1996; 65–74.
- Messer Y., Escande B. Erytropoietin and iron in the anemia of prematurity. TATM 1999; 15–17.
- Ohls RK The use of erythropoetin in neonatoles//Clin Perinatol. 2000; 20(3):681–696.
- Ulman J. The role of erythropoietin in erythropoiesis regulation in fetuses and newborn infants//Ginekol. Pol. 1996; 67:205–209.
L. A. Anastasevich , Candidate of Medical Sciences A. V. Malkoch , Candidate of Medical Sciences, Russian State Medical University, Moscow
Symptoms of anemia
Signs of anemia affect many organs and systems. The first visible signs appear on the skin, which becomes pale and flaky. Nails and hair become brittle, flake, and lose their shine. If you examine the earlobes in the light, you will see their transparency (Filatov’s symptom). The tongue may become inflamed, and aphthae (superficial ulcers) appear in the mouth. The nervous system suffers: babies become lethargic, whiny, they often feel dizzy, and there is noise in their ears. Sleep becomes shallow, bedwetting (enuresis), and fatigue may occur. Children who experience severe anemia before the age of 1 year may fall far behind their peers in development. Cardiovascular system disorders manifest themselves in low blood pressure, fainting, and rapid heartbeat. Systolic (at the moment of contraction) heart murmurs may appear.
Why does the disease occur?
The causes of anemia in childhood are as follows:
- the predominance of dairy foods in the diet;
- vitamin deficiency;
- lack of iron intake from diet;
- lack of food;
- consequences of infectious diseases in the body;
- worms;
- vegetarian food;
- genetic defects.
The factors will be somewhat different if anemia occurs in an infant. At this age, the role of the iron depot, which was formed during intrauterine life, plays a role. If the mother suffered from iron deficiency, then the likelihood of pathology in the baby increases sharply. Eating unadapted formulas worsens the course of the disease in children with congenital iron deficiency.
Causes
According to the time of occurrence of anemia there are:
- Intrauterine.
During intrauterine development, the fetus creates an iron reserve, on average 300 mg. Peak iron accumulation occurs in the third trimester. If the period from 28 to 32 weeks is unfavorable (threat of miscarriage, placental abruption, fetoplacental insufficiency), the fetus does not have time to stock up on iron. The likelihood of anemia is high in premature babies and children born from multiple pregnancies. - Intranatal and early neonatal.
During childbirth, prerequisites for the development of anemia can also be created - early placental abruption, rupture of umbilical cord vessels, and fetal injuries. After birth, the main danger is fetal hemolytic disease (destruction of fetal red blood cells by maternal antibodies) and genetically determined bone marrow diseases. - Purchased.
Anemia is subsequently caused by poor nutrition. This happens if there is little iron in breast milk, inappropriate formulas or cow's milk are used. Premature babies and those children whose body weight is higher than normal require more iron than usual. Anemia occurs when there is insufficient supply of B vitamins, macro- and microelements, and when the baby lives in poor sanitary and hygienic conditions.
At risk are children with blood diseases, frequent nosebleeds, food allergies and atomic dermatitis (a childhood form of eczema), impaired absorption in the intestines. In children, anemia develops with any more or less severe infection (pyelonephritis, bronchiectasis), helminthic infestation, connective tissue diseases (rheumatoid arthritis).
Causes of B12 deficiency anemia
A lack of vitamin B12 may be due to the following reasons or a combination of them:
- impaired absorption of the vitamin in the intestine: gastritis associated with Helicobacter pylori infection, Crohn's disease, previous intestinal surgeries, polyposis of the gastric mucosa, cancer, intestinal fistulas, etc.;
- congenital metabolic disorders;
- chronic intoxication with nitric oxide, used as sedation in anesthesiology.
- minor absorption disorders, for example, a decrease in the availability of B12 in food with chronic pancreatitis, moderate atrophic gastritis, taking metformin, medications to reduce the production of hydrochloric acid, etc.;
- poor diet, vegetarianism;
- chronic alcoholism.
One form of B12 deficiency anemia is Addison-Biermer disease. With it, autoantibodies appear against the cells of the gastric mucosa.
It is worth noting that B12 and folate deficiency anemias are closely related. Folic acid (vitamin B9) also takes part in the formation of red blood cells. Even a full supply of these components in food does not guarantee the absence of anemia in cases where there is an increased consumption or there is a violation of utilization in the bone marrow. This may be due to parasitosis, intestinal dysbiosis, pregnancy, liver and blood diseases.
Diagnosis of anemia
The diagnosis is established after a laboratory blood test, namely the number of red blood cells and hemoglobin.
They speak of anemia if the amount of hemoglobin is less than 110 g/l, red blood cells are less than 3.5 x 10¹²/l. These indicators correspond to a mild degree of anemia. Moderate anemia is established with the following indicators: hemoglobin less than 90 g/l, red blood cells up to 2.5x10¹²/l, severe anemia with hemoglobin less than 70 g/l, red blood cells less than 2.5x10¹²/l. When anemia is detected, the child is consulted by specialized specialists: gastroenterologist, nephrologist, allergist and others as appropriate.
What is anemia
To understand what anemia is, you first need to understand how blood cells function. Blood is made up of several types of cells, almost half of which are red blood cells (RBCs). These cells contain a red pigmented protein - hemoglobin. The function of hemoglobin is to carry oxygen from the lungs to the tissues, and carbon dioxide, formed during metabolism, from the tissues to the alveoli of the lungs. Anemia occurs when there is not enough hemoglobin in red blood cells or when there are not enough healthy red blood cells to transport oxygen throughout the body. Anemia can cause problems with cell function and growth.
Treatment of anemia
Methods for correcting anemia depend on age.
When breastfeeding, it is necessary to introduce vegetable, fruit and meat complementary foods on time, and spend a lot of time in the fresh air, including in the sun. The room must be well ventilated, kept clean, and sanitary rules for child care must be observed. For older children, it is enough to streamline their diet and daily routine to improve their blood tests. The diet includes beef liver, legumes, seafood, fresh vegetables and fruits, and herbs. If necessary, the timing of vaccination is postponed, massage and ultraviolet irradiation are used.
Medicines are prescribed by a doctor. Iron supplements and vitamins are indicated. The minimum duration of drug treatment is 1 month.
Diagnostic features
Treatment of B12-deficiency anemia is prescribed after a comprehensive examination. The doctor will order the following laboratory hematological and other tests:
- general blood analysis;
- biochemical and immunological studies: determination of the level of B12 in plasma, assessment of the level of homocysteine in serum or blood plasma, determination of antibodies to gastric parietal cells, etc.;
- bone marrow aspiration or trephine biopsy.
Gastroscopy may also be required to detect atrophic gastritis.
The diagnosis is made by a doctor based on complaints, manifestations of the disease, and laboratory test parameters. It is important to find out the cause of the syndrome, especially to detect Addison-Biermer disease.
In addition, a specialist needs to distinguish this type of anemia from other diseases accompanied by disturbances in hematopoietic processes. Thus, if liver cirrhosis is suspected, disorders associated with long-term use of certain drugs (sulfonamides, anticonvulsants), sideroblastic anemia will require differential diagnosis.
Prevention of anemia
Prevention begins with good nutrition for the pregnant woman, allocating sufficient time for walking and sleeping. Children of the first year of life need to add complementary foods to breast milk after 6 months of age; for older children, a varied, balanced diet should be organized. It is important that during the warm season the baby spends as much time outdoors as possible and takes sunbathing. The team of doctors at the SM-Doctor clinic will help your baby cope with anemia and develop individual preventive measures. Contact professionals to create ideal conditions for the growth and development of your child!
Features of treatment
Treatment of B12 deficiency anemia is based on replenishing the deficiency with vitamin B12 preparations. In almost all cases, this allows you to get a positive effect. Sometimes parenteral administration is advisable. Intramuscular injections are given daily or every other day, dosage is up to 500 mcg, depending on the severity of the condition. In the presence of a precomatous state, a dose of up to 1000 mcg may be required.
The dosage is reduced as the number of red blood cells and hemoglobin levels increase. Therefore, it is important to perform intermediate monitoring; the doctor will tell you how often you will need to take a blood test during therapy. Typically, the course of treatment takes at least 21–28 days.
If there are symptoms of funicular myelosis (paresthesia - numbness of the limbs), vitamin B12 is administered in large dosages daily for at least 10 days. Then the dose is reduced, and the course of therapy is supplemented with vitamin B1 at 100 mcg per day.
The criterion for the effectiveness of treatment is: an increase in the number of reticulocytes on the fifth – seventh day from the start of the course of therapy. As soon as remission is achieved, the patient is transferred to maintenance therapy. It consists of using the B12 drug at a dosage of 100–200 mcg 2–3 times a month, taking into account the daily requirement.
It is worth noting that patients with severe neurological symptoms can be transferred to lifelong maintenance therapy: 1 mg monthly.
It is important to understand that the form of the drug does not matter - drugs in tablets and injection solution are absorbed equally well. But the second method is preferable in cases where there are diseases of the gastrointestinal tract or impaired absorption of vitamins in the intestines.
Folic acid is used intramuscularly or orally, the standard dose is 50–60 mg. It is usually combined with B12. However, it is important to know that the use of folic acid causes an increased consumption of B12, sometimes leading to increased paresthesia in the limbs. The doctor will develop a treatment regimen for B12-deficiency anemia, taking this fact into account individually, especially for pregnant patients.
If there is a significant decrease in hemoglobin levels, blood transfusions may be indicated. Pre-comatose, comatose state, and cardiac symptoms are also grounds for serious intervention. It is preferable to choose red blood cell transfusion in a course of up to 6 transfusions.
Prognosis and prevention
Timely treatment of B12-deficiency anemia in most cases can completely eliminate the hematological disorder. Already on days 4-5, changes in test results can be detected; an increase in hemoglobin and the number of red blood cells is observed on the 7th day. These indicators are completely normalized after 8 weeks.
Neurological symptoms can go away for quite a long time, up to six months. Spinal cord damage associated with anemia is irreversible, so it is very important to promptly consult a doctor: a hematologist or therapist.
Increased attention to the prevention of this disease should be paid to patients who have undergone bariatric surgery or gastrectomy. At risk are vegetarians, people on strict diets with limited meat and offal, pregnant women and women who have recently given birth. Prevention consists of using the B12 drug in the form of tablets or injections; the doctor will select a safe prophylactic dose.