Cervical erosion is a common pathology that occurs in more than a third of women. Modern medicine recognizes that surgical treatment is appropriate only in extreme cases. In IMMA clinics, the necessary studies are performed, observation and treatment of pathological conditions associated with changes in the epithelium of the cervix is carried out. The patient can count on highly qualified assistance in solving the problem that has arisen.
In our clinics you can:
- Get a consultation with a gynecologist;
- Receive pregnancy planning services;
- Undergo hysteroscopy;
- Remove vaginal cyst;
- Treat cervical erosion with radio wave coagulation;
- Get professional advice from other specialists and much more!
For more details and any questions, please contact the number listed on the website.
In modern medicine, the term “cervical erosion” refers to two different pathologies that involve disruption of the epithelium. For diagnosis, a visual examination by a gynecologist is sufficient, so regular visits to the doctor will guarantee protection against possible complications.
Features of the structure of the cervix
The cervix is the lower part of the uterus that protrudes into the vagina. In its center there is a canal that connects the cavities of the uterus and vagina. In normal condition, the surface of the organ is pink and smooth. The epithelium of the outer side consists of several layers of cells:
- basal tissue, in this layer of the mucosa there is continuous cell division, which ensures the replacement of the upper layers of the mucosa;
- an intermediate layer consisting of maturing cells formed in the basal tissue;
- superficial or functional tissue, consists of flat cells that provide mechanical and biological protection from adverse factors.
The inner surface of the uterus is lined with another type of tissue - single-layer epithelium, consisting of cylindrical cells. The appearance of the surface differs from the surface of the neck in a brighter, often red color. In normal condition, the tissue of cylindrical cells is not accessible during a gynecological examination. The junction point of the flat and cylindrical types of epithelium is located inside the cervical canal; normally it cannot be seen.
Why is colposcopy necessary?
A definitive diagnosis of erosion can only be made with colposcopy. After treating the cervical surface with Lugol's solution, all existing defects become noticeable:
- With true erosion, a bright red area of desquamated epithelium is detected, on the surface of which the vessels are clearly visible.
- With pseudo-erosion, an area of replacement of healthy multilayered squamous epithelium with areas containing pathological glands, cysts, and unusual cells is visible.
- With ectropion, an inversion of the tissues of the cervical canal into the vagina is detected. The affected neck has a bright red eroded surface. Scar tissue changes are often observed.
For final diagnosis, a cytology smear is taken to find out what cells the modified area consists of. If a gynecologist discovers cancer cells, the disease moves from the category of erosions to oncological ones. This is why erosion is dangerous - without treatment it can increase, become infected and transform into uterine cancer.
True erosion
By the term “cervical erosion,” experts understand two different pathological conditions of the epithelium that are interconnected.
True erosion is damage to the upper layer of the epidermis and is essentially a wound. This disorder looks like a bright red round ulcer with irregular edges. It is characterized by swelling, inflammation, purulent and bloody discharge.
Such erosion does not always require special treatment; the healthy layer of the epithelium restores itself within two to three weeks. If the damage is shallow, there is no infection attached to it, and the body has a strong immune system, then the epithelium quickly recovers. However, the healing process must be supervised by a specialist to avoid the development of complications.
The causes of true cervical erosion can be different:
- mechanical damage as a result of childbirth, abortion, rough sexual intercourse;
- inflammatory processes in the vagina and cervical canal. Acrid secretions can corrode the top layer of cells;
- the influence of infections, pathogens injure the delicate epithelium.
In some cases, complications such as scarring may occur. They deprive the upper layer of the cervix of the necessary elasticity, which threatens damage and rupture during natural childbirth.
Symptoms of true cervical erosion have been erased. This is due to the peculiarity of the structure of this organ: there are no nerve endings here, so damage, ulcers and wounds bother the woman little and heal independently and imperceptibly.
If complications occur, for example, infection or the development of an inflammatory process, signs of true cervical erosion become more obvious. Unpleasant sensations appear during sexual intercourse, pain in the lumbar region, and discharge with blood elements is observed.
Another common consequence of improper repair of the epidermis is the replacement of the multi-layered, cylindrical appearance of tissue with flat cells lining the inner surface of the uterus. This condition is called ectopia or false erosion.
Is it necessary to treat erosion?
Timely treatment of erosion allows you to avoid the development of serious infectious and inflammatory processes, since the pathological area of tissue is an open gate for various pathogens. In addition, long-term untreated erosion may be accompanied by bleeding and the appearance of uncharacteristic vaginal discharge, which complicates sexual activity and causes discomfort in the woman.
An even greater danger is the degeneration of eroded tissues into cancerous ones. This, alas, also happens not so rarely.
Ectopic cervix
This phenomenon occurs in more than a third of the fair sex. Ectopia was excluded from the list of gynecological diseases. In modern medicine, it is considered a structural feature of the epidermis and requires urgent treatment only in certain cases.
The following reasons for the appearance of false erosion of the cervix are identified:
- hormonal imbalances caused by disruption of the adrenal glands, ovaries, and thyroid glands;
- sexually transmitted infections;
- long-term inflammatory processes in the vagina and cervical canal with a large amount of secretions that damage the delicate layer of the epithelium;
- vaginal dysbacteriosis, microflora disturbance as a result of non-compliance with hygiene rules, unprotected sexual intercourse, frequent change of sexual partners;
- decreased immunity;
- complications during the healing of true erosion and other damage to the cervix.
Recent studies have shown that already at the stage of intrauterine development in girls, the development of false erosion is observed. The true causes of the phenomenon are poorly understood. This pathology does not require treatment and usually disappears on its own before the age of 25, when the process of maturation of epithelial cells of the vagina and cervix ends.
Causes of the disease
There are many of them, as well as risk factors. Any changes in the mucous membrane of the cervix can lead to the development of erosion. Such changes occur in diseases of the genitourinary system, after childbirth, after artificial termination of pregnancy, and are observed during hormonal diseases. Often, sexually transmitted diseases lead to erosion - their pathogens enter the body through the mucous membrane, damaging the epithelial tissue.
There is no specific age category susceptible to this disease. Erosion can develop both in adolescence and in old age.
Types of ectopia
The spread of squamous epithelium can affect the deep layers of the surface of the cervix and cause various neoplasms and changes in tissue structure. There are three forms:
- clean look. The modified surface is smooth and has a brighter red color. Usually occurs with congenital pathology.
- glandular, involves deep tissue changes, its appearance resembles a sponge.
- cystic, accompanied by the appearance of tubercles with signs of an inflammatory process.
- mixed, combining both types.
A complicated recurrent false ulcer requires close monitoring by a physician, as it can cause a malignant tumor. In this case, it may be necessary to remove the cervical erosion.
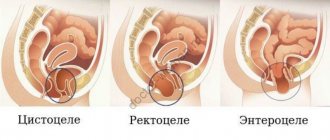
Ectropion and ectopia
Cervical ectropion is an inversion of the mucous membrane of the cervical canal into the vagina, which can occur as a result of rupture of the cervix after childbirth or abortion. Eversion is usually localized around the external os of the cervix from the posterior lip, but can be more pronounced.
Cervical ectopia (also called “endocervicosis”) is a condition in which columnar epithelial cells covering the inside of the cervix enter the area of stratified squamous epithelium covering the outer part of the cervix. When examining the cervix in the speculum, an area of hyperemia around the external os of the cervical canal is visualized, ranging in width from several mm to 2 cm without clear boundaries.
In rare cases, ectopia may be congenital. They are formed during the prenatal period due to the displacement of the zone covered by columnar epithelium outside the cervical canal. They are often small in size, bright red in color, have a smooth surface and are not accompanied by an inflammatory process. Congenital erosions can go away on their own, but if they persist until puberty, they tend to become infected in the future.
The cylindrical epithelium covers the resulting defect, but also gradually grows into the tissues, forming peculiar branching glandular ducts. It produces its own secretion, which accumulates in the formed channels. If they are highly branched, the outflow of secretions from them becomes difficult, which leads to the formation of cysts of different sizes and numbers. They can be very small and invisible to the naked eye or reach a large size and become clearly visible even during a standard gynecological examination. Sometimes cysts form in the area of erosion so large that they resemble cervical polyps.
If the pathology is not detected in a timely manner and treatment is not started, the number of cysts will progressively increase, which will provoke thickening of the cervix (hypertrophy). Depending on what cystic formations are formed, different types of cervical ectopia are distinguished:
- follicular or glandular - characterized by the presence of clearly marked cysts and glandular ducts;
- papillary - characterized by the presence of papillary growths on the surface of cystic formations with characteristic signs of inflammation;
- mixed - have features of both types of pseudo-erosions.
Doctor's comment: Cervical ectropion is a favorable environment for the proliferation of pathogenic microorganisms that cause inflammatory diseases. Ectopia of any kind itself becomes the cause of inflammation, and with a long course it leads to pathological changes in epithelial cells, in particular atypia and dysplasia. Since the presence of dysplasia is considered to be a precancerous condition of the cervix, such erosions require treatment as quickly as possible, and surgically.
For pregnant women, the presence of erosion can increase the likelihood of miscarriage or premature birth. But treatment is not carried out during this period, since it will further increase the likelihood of miscarriage.
Doctor's comment: Sometimes erosions of nonspecific etiology can self-epithelialize after a short time (from 3-5 days to 1-2 weeks), but, unfortunately, this outcome is extremely rare.
Signs of ectopia
Symptoms and signs of false cervical erosion are as follows:
- copious, odorless discharge;
- pain during sexual intercourse;
- spotting after sexual intercourse or medical procedures;
- burning sensation.
If complications occur, for example, an infection or an inflammatory process, the symptoms intensify, the discharge becomes purulent with a pungent odor, and vaginal itching may appear.
Erased symptoms and irregular visits to the doctor lead to the fact that the pathology develops for many years. Under the influence of complications, there may be a threat of malignant tissue degeneration.
Symptoms of uterine erosion
Often this disease does not produce pronounced symptoms, being detected only during a colposcopic examination by a gynecologist (standard examination using a special device), but sometimes the disease manifests itself with the following symptoms:
- The presence of light yellow, whitish or bloody cloudy discharge, sometimes with an unpleasant odor;
- Light bleeding, expressed in the appearance of a small amount of blood in the form of drops or smears after sexual intercourse.
To determine the direction of therapy as accurately as possible, specialists prescribe a comprehensive laboratory test, colposcopy and other diagnostic measures.
Causes of ectopia
In modern medicine, there are several theories that reveal the causes and mechanisms of the appearance of false erosion. The most common opinion is that the disease is inflammatory in nature. Inflammation in the vagina and cervical canal leads to the formation of a large amount of discharge that irritates the epithelium of the cervix. True erosions occur, but due to an unfavorable environment and lack of treatment, healing is accompanied by the replacement of cylindrical cells with flat ones.
It is believed that hormonal imbalance can cause ectopia. Decreased steroid production leads to tissue replacement. This phenomenon can be observed in girls during puberty, in pregnant women and women experiencing menopause.
Ectopia occurs with mechanical damage during childbirth, eversion and prolapse of the pelvic organs.
How to prepare
Before treating erosion, a woman needs to undergo some tests and make sure there are no contraindications. It is mandatory to pass:
- General blood and urine analysis;
- Blood clotting test;
- Test for HIV, hepatitis, syphilis;
- Fluorography;
- ECG;
- Cytological analysis of the cervix;
- Colposcopy;
- Ultrasound examination of the pelvic organs;
Also, before the operation, a consultation with a general practitioner is required, and in the presence of chronic diseases, a consultation with specialized specialists.
If the tests indicate inflammation or infectious diseases, it is first recommended to carry out treatment and retake the tests.
When planning to undergo radio wave therapy with the Surgitron apparatus, it is recommended that you familiarize yourself with the following recommendations:
- Radio wave treatment of the cervix is carried out from 5 to 10 days of the cycle.
- 10 days before the upcoming treatment, you should avoid baths, saunas, swimming pools and swimming in open water.
- In some cases, doctors recommend taking a daily dose of antibacterial drugs the day before the procedure to prevent inflammation. Please discuss this with your doctor.
- Drugs that affect blood clotting should be discontinued for 10-14 days before the procedure.
Erosion during pregnancy
The appearance of ectopia during pregnancy is a consequence of changes in a woman’s hormonal levels, a decrease in immune defense, and does not require special treatment. The danger lies in possible complications. The affected areas of the cervix do not perform a protective function, so the threat of infection and the occurrence of an inflammatory process increases. The doctor chooses the most gentle medications allowed during pregnancy.
Prevention of complications is to follow the rules of personal hygiene and use condoms during sexual intercourse.
Injuries during childbirth can cause true erosion. Against the background of recovery processes and the removal of lochia, the disease goes unnoticed by the young mother.
Complications of erosion
Erosion, like any other non-healing wound, is an open gate for infections, therefore, with untreated erosion, the risk of additional illness is increased significantly. Pathogenic microorganisms multiply on the surface of erosion very quickly, gradually penetrating the uterus and ovaries, and this is a direct path to diseases such as endometritis, myometritis, adnexitis, HPV, herpes and others. The consequence of this effect on a woman’s reproductive system can be infertility.
A more serious complication of erosion is the risk of degeneration of a benign process into a malignant one, that is, into a cancerous tumor of the cervix.
Diagnostic methods
Pathological changes in the epithelium of the cervix are clearly visible during a gynecological examination. To make an accurate diagnosis and determine a treatment strategy, the following studies are carried out:
- colposcopy;
- smear;
- cytology;
- tests for infections, including AIDS;
- bacteriological culture;
- biopsy.
Colposcopy. This examination method involves a careful study of pathology using special equipment. The colposcope magnifies the image thirty times, allowing you to accurately determine the nature of the changes. To determine the type of fabric, solutions of iodine (Lugol) or vinegar are used. They do not harm the mucous membrane, but due to the reaction of the tissue, they paint it in different colors, which makes it possible to highlight problem areas. The specialist carefully studies the modifications, notes areas that require the use of additional research methods, including cytological analysis and biopsy.
Cytological examination. Cytological analyzes show modifications in the structure of cells, the presence or absence of signs of malignant changes. To conduct the study, the doctor makes a scraping.
Biopsy. This test involves examining tissue for signs of malignant changes. During a colposcopy, the doctor identifies areas that require checking. The tissue plucking procedure is painless and may be accompanied by slight discomfort. This study is mandatory before determining treatment methods for cervical erosion.
Tests for the presence of infections, determination of the state of microflora. One of the first steps in treating erosion is identifying infections and inflammatory processes. They can be the cause of a disease, after elimination of which the normal outer covering will be restored.
Diagnostics
Diagnostics includes examination, instrumental methods and laboratory tests. Diagnosis is often delayed due to the fact that in the absence of pronounced symptoms, patients simply do not consult a doctor. If there are symptoms, they are usually associated with the disease that provoked the development of erosion. Thus, the disease can be detected in a timely manner only by undergoing preventive examinations. A standard visual examination of the cervix allows the gynecologist to suspect the development of erosion, and colposcopy is used to confirm the diagnosis - this method allows one to examine pathological tissues under magnification.
If the doctor suspects that the process of development of malignant tumors has already begun, then a study such as extended colposcopy is used. First, the affected area is treated with an iodide solution, and then examined under magnification. If dysplasia is suspected, a biopsy may be required for histological analysis in the laboratory.
Treatment methods
The results of the examination will enable the doctor to determine how to treat cervical erosion. First of all, it is necessary to eliminate infections and inflammatory processes.
Treatment of cervical erosion is not always required. For example, with congenital ectopia and minor changes in the epithelium that do not cause discomfort, one observation is sufficient.
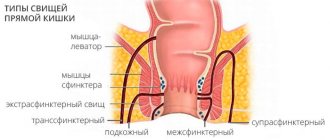
If ectopia does not go away after 25 years, occupies a large area, and is accompanied by complications, then various techniques are used, which are based on the same mechanism. The pathological layer of cells is destroyed so that normal epithelium is restored in its place. There are several methods. Varying in availability and possible consequences:
- diathermoregulation;
- cryodestruction;
- radio wave exposure;
- laser therapy.
Radio wave exposure is the most gentle method of treatment. After it, a scab does not form, since the pathological layers of cells do not simply die, but evaporate, and a film appears instead. Healing occurs quickly, there are no scars.
The answer to the question of whether cervical erosion should be cauterized depends on each individual case.
Treatment
Radical treatment is predominantly surgical. But there are situations in which dynamic observation and conservative therapy are preferable.
Basic principles of treatment:
- For congenital pathology, observation is preferable. Removal is required if the pathology develops or symptoms that are unpleasant for the patient are present.
- True and pseudo-erosions require correction of the underlying disease. If, along with the cure of the primary disease, regression of erosion does not occur, then removal is prescribed.
- If there are signs of infectious inflammation, the pathogens are first eliminated (most often these are microorganisms that cause the development of sexually transmitted diseases).
- If the erosion is in the active stage (true), then surgery is not indicated. Gentle treatment methods are used, aimed primarily at eliminating unpleasant symptoms.
Surgical treatment using modern means is aimed at destroying the layer of cylindrical cells. After this, rejection occurs, and the growth of normal squamous epithelium begins at the site of the pathology.
Basic surgical methods:
- thermocoagulation
Thermocoagulation is a method that is based on cauterization under the influence of current. The disadvantage of this method is the possibility of scar formation. For this reason, thermocoagulation is offered only to patients who do not plan to have children in the future. Complete healing takes up to three months.
- use of laser
Laser cauterization requires careful sanitation. This method is painless and leaves no scars. Complete regeneration takes four weeks.
- Radio wave destruction of erosion is performed using special equipment and has advantages over standard electrocoagulation in the form of healing without scar formation.
- cryodestruction
- Cryodestruction (cryocoagulation)
Cryocoagulation is destruction by cold using liquid nitrogen.
When prescribing surgical treatment, a study is required to exclude the development of oncology. And if the process of development of a malignant tumor has already begun, removal can provoke tumor growth.
Prevention consists of timely treatment of inflammatory and infectious diseases, as well as regular visits to the gynecologist and preventive examinations. Erosion can be detected during a routine examination by a gynecologist, and treatment should begin as early as possible.
In the multidisciplinary CELT clinic, you can undergo a complete diagnosis, after which the doctor will develop a treatment regimen, if necessary. It’s easy to be healthy – together with attentive doctors and modern treatment methods.
Prevention and observation are the key to health
A frivolous attitude towards ectopia can lead to serious complications: infertility, cancer. The affected epithelium does not perform protective functions, therefore the risks of inflammation and infection with infectious diseases increase. Unjustified aggressive methods of exposure can lead to scars and relapses.
High-quality observation and treatment of cervical erosion in Moscow is carried out in IMMA clinics. The availability of the latest equipment, the ability to conduct high-precision laboratory tests, and the professionalism of our employees guarantee success in the prevention of gynecological diseases.
Regular gynecological examinations are necessary to maintain women's health!
Our services
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Colposcopy | 1 800 |
| Taking a biopsy for diseases of the cervix using radiosurgery (excluding the cost of histological examination) | 5 000 |
| Coagulation using radiosurgery in the treatment of cervical diseases | 3 000 |
| Coagulation using radiosurgery in the treatment of cervical diseases with simultaneous biopsy taking (excluding the cost of histological examination) | 7 500 |
| Appointment with a surgical doctor (primary, for complex programs) | 3 000 |
All services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
If the doctor found “erosion”: part 2
Unfortunately, despite my indignation, most obstetricians-gynecologists continue to use the definition of “cervical erosion” in everyday practice.
This does not mean that they studied poorly or do not know something, but the problem is that such a diagnosis sometimes misleads patients, and there is often no time to explain.
So what to do if sacramental words were nevertheless spoken during the inspection?
- Could you see if I have erosion? - Certainly. We will need a smear “for cancer cells” and a colposcopy. - What, you can’t just watch how other doctors look and simply say whether there is erosion or not?
I can not. The point here is not perfectionism and not that the term “erosion” makes me cringe. The fact is that any “incomprehensible red spot” on the cervix requires mandatory cytology and colposcopy. Because I know for sure: the pinkest and smoothest neck can turn out to be sick. Cytology must be taken from all sexually active women who have reached the age of 20 (earlier for early sexual debut), regardless of whether the doctor saw “erosion” or not.
However, if during an examination the doctor categorically declares: “You have erosion on your neck!”, this does not mean that it is time to run away without looking back. Most likely, the doctor is simply too lazy or has no time to go deeper. It doesn't matter what he says. What is much more important is what he will do next.
Step 1. The doctor will take a “smear for cancer cells” - a cytological examination
Cytological examination of smears from the surface of the cervix and cervical canal makes it possible to detect cancerous and precancerous changes on the cervix long before they become visible to the naked eye. The Greek scientist, Georgios Papanikolaou (1883–1963) developed a revolutionary technique for the early diagnosis of cervical pathology, which we still use today. Back in 1928, he published the first results of a cytological study of cervical smears, which were received very skeptically. However, the scientist was persistent. In 1943, he outlined his observations in the monumental work “Diagnosis of Uterine Cancer by the Vaginal Smear” and became the founder of a new direction in medical science.
Inexpensive and uncomplicated cytological examination of smears has made it possible to conduct large-scale screening studies. For whatever reason a woman came to the gynecologist, she always came for a cytological smear. It is for the sake of a cytological smear that women are “driven into the chair” during medical examinations.
According to WHO, mass cytological screening in national programs among women aged 25–64 years with an interval of 5 years can reduce mortality from cervical cancer by 84%.
Step 2. The doctor will perform a colposcopy
Hans Ginzelmann is considered the author of the method of intravital microscopic diagnosis of the condition of the cervix. He invented the first colposcope in 1925 and devoted his entire life to perfecting the technique.
“Anyone who is accustomed to examining the cervix at 10x magnification will never again be satisfied with a routine examination.” Hans Ginzelmann
In most cases, in young women, a red spot on the cervix will be an ectopia of columnar epithelium.
"Ectopia" is translated as "located outside." This is the very normal condition inherent in the juvenile type of cervical development. The columnar epithelium is located on the ectocervix and may be surrounded by a normal transformation zone. Ectopia is not a disease or even a risk factor for developing the disease. No treatment is required for simple ectopic columnar epithelium. The only exception would be a very large size of ectopia with a transition to the vaginal vaults and an accompanying chronic inflammatory process that is not amenable to correct and persistent conservative treatment.
To my deepest regret, the meaningless diagnosis of “cervical erosion” was transformed into an even more ridiculous one – “ectopia of the cervix.” The cervix does not stick out anywhere and is not “located outside”; it is an unsuccessful copy of cervical ectopia (fortunately, most thinking clinicians are already rearranging themselves and pronouncing the correct “cervical ectopia”). And it is absolutely unimaginable when the conclusion “cervical ectopia” is made without any colposcopic examination at all, just by eye.
Unexplained red spots" on the cervix cannot be somehow interpreted without using colposcopy. This is not just looking at the neck under 8-, 16-, 25-, 32-fold magnification. This is carrying out special vascular tests with a solution of acetic acid and Lugol's solution. Under the influence of simple solutions, the neck is transformed. And now the incomprehensible red spot acquires the clarity and granularity of cylindrical epithelium, or whitish areas appear, reminiscent of cobblestones. In pathological areas, the doctor examines abnormal vessels of bizarre shape or epithelial glands with bumpy keratinizing ridges.
Colposcopic conclusion is the most important component of diagnosis. If the colposcopist describes a normal appearance, in most cases no activity is required. Abnormal colposcopic pictures are a direct suspicion of pre-stage cancer. This requires attention and clarification.
Step 3. The doctor will take a biopsy from suspicious areas
“The most accurate diagnosis is made by a pathologist.”
A cervical biopsy should be taken from all suspicious areas found during colposcopy. A piece of tissue can be pinched off using biopsy forceps or cut off with a loop of a radio wave device. The material is sent for histological examination. The tissue pieces are sent to the pathology laboratory, where they are processed, embedded in paraffin, cut into thin strips and fixed on glass slides. A pathologist (yes, the one who dissects corpses) will carefully examine the slides under a microscope, think, compare, scold poorly taken material, but still give a detailed description. It is the pathologist who formulates the final conclusion about what we saw in the colposcope.
A cervical biopsy could well become the gold standard for diagnosis if not for the notorious human factor. Firstly, the doctor may miss, even if the biopsy is performed under the control of a colposcope. Secondly, the material may not be taken deep enough or with damaged edges. In this case, you cannot count on an accurate conclusion; the pathologist is not a magician.
Cytology is in order, the colposcopy conclusion is “ectopia of columnar epithelium”, the biopsy is good - we can cauterize!
Alas, such stories are not uncommon. Of course, I would like to ask the question where the biopsy was taken from if the colposcopist did not see suspicious areas. And what exactly were they going to treat with “cauterization” if cytology, colposcopy and biopsy did not find pathological changes. The merciless fight against cervical ectopia under the banner of cervical cancer prevention has been going on in our country for more than forty years. Several generations of “cauterizer” doctors have already grown up, confident that they are doing a good deed.
Slowly and creakingly the realization comes - for many years we have been mercilessly treating completely healthy women. This would not be so terrible if we did not manage to miss those who really needed help. There is still a misconception that smears for oncocytology should be taken only from those who have “erosion”.
Unfortunately, harmless-looking pink necks can be very insidious. Not long ago, I did a colposcopy on a 26-year-old girl and came to the conclusion of H-SIL (pronounced colposcopic lesion, most likely CIN II-III - severe or moderate dysplasia).
- Why didn’t anyone tell me about this before? Why has no one seen this before?
- Probably because no one did a colposcopy on you. Absolutely any obstetrician-gynecologist can repeat this and, with sequential treatment with solutions of acetic acid and iodine, see rough whitish epithelium, mosaic and areas not stained with iodine.
Step 4. The doctor will see inconsistencies
It happens that the results of the examination do not add up to a single picture. Cytology is good, colposcopy is vaguely suspicious, biopsy is uninformative. Then, to make a decision, you will need one more “building block” - the results of HPV testing. If the test reveals highly oncogenic HPV (HPV-16 and HPV-18 are especially aggressive), the specialist will choose a more aggressive management tactic. If HPV is not found, it is more likely to simply continue monitoring.
Step 5. The doctor will make a diagnosis
Using a full arsenal of diagnostic capabilities, a doctor who confidently understands the pathology of the cervix will easily move from vague “erosion” to an absolutely specific conclusion. “Erosion” may be scar deformation after childbirth, ectropion (postpartum eversion), endometriosis, polyp, condyloma, leukoplakia. For each case there is a specific algorithm of actions. As soon as the doctor finds out what kind of “erosion” he is faced with this time, he will receive a clear and unambiguous answer to the question “What to do?”
Oksana Bogdashevskaya
Photo 1 - thinkstockphotos.com, 2 - teslasociety.com, 3 - 4 - provided by the author, 5 - shroudstory.com
How does a doctor determine the treatment method?
Having carefully studied the patient’s condition, determined the degree of development and depth of erosion, and also identified its cause, the gynecologist, based on the data obtained, determines the method of treatment that can have the maximum impact on the leading factor that caused the disease.
If an infectious-inflammatory process is observed, the gynecologist will prescribe antibiotics. Traumatic erosion requires a different treatment method. In this case, doctors most often recommend removing the damaged part of the tissue using one of the modern methods. Various techniques are used to treat erosion, the choice of which depends on the equipment of the clinic, the type of erosion and the capabilities of the patient.
Today, instrumental methods for eliminating erosion, such as laser destruction, electrocoagulation, radio wave surgery and cryodestruction, are considered the most effective and safe.
All of the methods listed are either completely painless, for example, laser, or simply unpleasant (electrocoagulation). In any case, a good doctor will not allow the patient to experience pain, so there is no need to be afraid of these procedures. If the pain threshold is high, modern anesthesia is used to relieve pain.