A fistula always comes suddenly, when the inflammation has already been cured or the surgical wound has long healed. Its appearance cannot be predicted, although its formation does not occur without symptoms, but it is impossible to guess that a fistula will occur in this place. But it is very difficult to confuse an emerging fistula with something else.
- What is a fistula?
- Types of fistulas
- Causes of fistulas
- Symptoms of appearance
- Diagnostic methods
- Methods for treating fistulas
- Prevention of fistulas
What is a fistula?
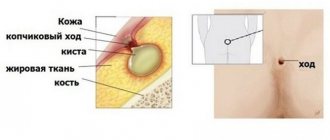
A fistula is an anastomosis formed as a result of a pathological process between the hollow organs of the gastrointestinal tract and/or genitourinary system. A fistula is also a convoluted tubular passage from an organ, passing through soft tissues with access to the skin.
A more euphonious name for a fistula, borrowed from Latin, is “fistula,” but this medical concept is broader, since it also includes artificially formed anastomosis, such as a surgically created fistula between a vein and an artery in dialysis patients. In one form, a fistula is a fistula; in another, it is an artificially created anastomosis; a fistula is always a miraculous pathology.
A fistula always has a beginning - an internal opening, localized in the primary focus of inflammation with suppuration. The beginning of a fistula can be a non-healing wound from injury or surgery, which is especially typical for organs of the gastrointestinal tract that produce secretions: gastric, intestinal or pancreatic juice, bile.
The external opening of the fistula can open into another organ or onto the skin, as in the case of a rectal fistula, but this opening is not necessary - some fistula tracts blindly end in soft tissues, muscles or fiber, forming purulent cyst-like cavities there - leaks.
How to treat a fistula
The concept of fistula implies an open channel between any organ and the surface of the body, otherwise it is also called a fistula.
As a rule, a fistula forms as a result of a complication after surgery or an advanced disease. Fistula can only be treated surgically; only granular fistulas can heal on their own. What types of fistulas are there:
Rectal, rectovaginal, duodenal, bronchial, gastric. Based on its shape, the fistula can be complete or incomplete.
What are the causes of fistula
- tuberculosis, Crohn's disease;
- actinomycosis;
- tumors;
- paraproctitis;
- surgical intervention;
- diseases of ENT organs;
- Dental complications.
Types of fistulas
The classification of fistulas is diverse; each organ has its own gradation of fistulas by location, sometimes the degree of involvement of surrounding tissues, and even by the volume of secretion released through the fistula.
Complete fistulas have an external and internal opening, incomplete fistulas have only an internal opening.
Those opening in the skin are called external fistulas, while fistulas connecting organs are called internal .
Depending on the number of organs involved in the process, internal fistulas can be combined or isolated . Isolated fistulas are named after the organ that gave rise to them: pancreatic, biliary, intestinal, vaginal, ureteric, and so on.
When there is an anastomosis of two or more organs - a combined type of fistula - a “combined” name is used, so with a fistula between the rectum and the vagina - rectovaginal fistula, with a fistula from the gallbladder to the stomach - cholecystogastric fistula, between the pancreas and the stomach wall - pancreatogastric or pancreas-gastric fistula.
According to the number of tracts, fistulas are divided into single-channel or simple and multi-channel or complex , as well as branched or indirect and unbranched or direct .
According to the condition of the tissues and course - infected or complicated fistulas, as a rule, purulent and “clean” uninfected or uncomplicated fistulas with the release, for example, of bile or pancreatic juice.
| Depending on the number of holes | Complete fistulas | They have two openings - they connect two organs to each other or one organ to the surface of the skin. |
| Incomplete fistulas | They only have one hole. | |
| Depending on the location of the second hole (for complete fistulas) | Internal fistulas | Connects internal organs. |
| External fistulas | Connect internal organs to the surface of the skin. | |
| Depending on the number of organs involved | Isolated fistulas | They are named after only one organ that gave rise to the fistula. |
| Combined fistulas | Two or more organs are involved. | |
| Depending on the course of the fistula | Single channel (simple) | One fistula tract. |
| Multichannel (complex) | Several fistula tracts. | |
| Branched (indirect) | There is a branching of the fistula. | |
| Unbranched (straight) | No ramifications. | |
| Depending on the presence of complications | Uncomplicated (uninfected) | There are no signs of infection. |
| Complicated (infected) | There are signs of an infectious process in the fistula. | |
| Depending on the current | Primary | The fistula was discovered for the first time. |
| Recurrent | The process either subsides or reactivates: inflammation develops, new fistula tracts appear or old ones open. |
Fistulas are divided into primary and chronically occurring - recurrent , when the process either subsides or becomes inflamed again with the formation of new passages and, sometimes, the closure of old ones.
A rectal fistula is classified in relation to the anal sphincter, and fistulas that are localized above the anus and go around it like a horseshoe, with an opening into the rectum, are also graded according to 4 degrees of complexity.
Complete pancreatic fistulas can be small with the release of up to half a glass of juice, medium - up to 700 milliliters and large.
There are as many classification options as there are types of fistulas in human nature.
Consequences that cause fistulas
A postoperative fistula can provoke the development of sepsis.
A postoperative fistula itself does not pose a threat to life. But if the patient lets everything take its course, then the pathogenic bacteria that are inside the fistula opening will begin to infect healthy organs and tissues, and this will provoke the appearance of quite serious diseases.
In addition, the body may refuse to respond correctly to medical therapy, which in turn can also cause quite serious complications.
The most common complications in the treatment of fistula after surgery:
- Abscess . Purulent masses fill the entire internal cavity of the fistula opening
- Phlegmon. In this case, the pus, in addition to tissues, also begins to affect fatty tissue.
- Sepsis. A fistula opening occurs inside the human body. The pus ends up on the patient’s internal organs.
- Fever by a purulent mass. Temperatures can rise to maximum levels. In this case, a person may lose consciousness and have difficulty oriented in space.
Causes of fistulas
Most fistulas are formed as a result of a complicated course of the inflammatory process : in acute pancreatitis, inflammation of the tissue surrounding the rectum - paraproctitis, ulcerative necrotizing colitis - Crohn's disease.
Destructive processes in internal organs can also give rise to the formation of a fistula tract, as occurs when pressure sores of the gallbladder wall are caused by a large stone, when compression of the tissues leads to their thinning and subsequent rupture. In three out of four women with cholelithiasis, bedsores are the leading cause of the formation of a biliary fistula.
A similar mechanism of local tissue destruction is activated when a gastric ulcer perforates or penetrates into the pancreas, resulting in the opening of the gastro-pancreatic fistulous tract.
Some researchers believe that the cause of fistula formation is ischemic changes in the rectal wall with frequent use of rectal suppositories with NSAIDs.
Surgical , birth and spontaneous are one of the leading causes of fistula formation. Surgical injuries can be accidental - not noticed during inspection and almost microscopic dissections of tissue in the operation area and delayed, when the body rejects the materials used in surgery: suture silk or stapler staples.
In addition to accidental surgical trauma, fistulas can be caused by surgical assistance during the opening of purulent paraproctitis. We are not talking about inadequate surgery, it’s just such an unfavorable place: poor blood supply to fiber - the main site of action, with the impossibility of stopping the transit through the intestine of feces, which are replete with intestinal microflora. There is no sterility and pathogenic microorganisms are always present - there are no conditions for the surgical wound to heal.
Injuries during childbirth , especially ruptures due to inadequate obstetric care, as well as injuries undetected during postpartum examination, are the most common cause of vaginal fistulas.
Changes in soft tissues after long-term radiation therapy , especially with combined irradiation of cervical or uterine cancer, and rectal cancer, can also lead to the formation of fistulas. Several factors predispose to the formation of a tract: impaired tissue nutrition as a result of post-radiation fibrosis in the presence of abundant intestinal and vaginal microflora. Post-radiation fistulas are quite difficult to differentiate from true malignant fistulas that form due to necrosis of a progressive or recurrent malignant tumor.
Pancreatic cysts, filled with caustic pancreatic secretions, are able to spontaneously find a way out for their contents, melting the tissue with enzymes and forming fistulous tracts from the abdominal cavity to the chest - between the pancreas and the pleura or bronchi.
A similar result, only with access to the skin, is possible with puncture drainage of cystic cavities of the pancreas, performed for therapeutic purposes in a weakened patient, or with drainage of a common bile duct blocked by a stone or tumor.
Each fistula has its own specific cause and combination of unfavorable conditions for healing.
Symptoms of appearance
The process of fistula formation is difficult to track; it can take several days, as happens with acute pancreatitis, or several months, as with post-radiation tissue changes.
Manifestations at the initial stage of fistula formation are due to its root cause, as a rule, a local inflammatory process resulting in purulent melting of tissue with pain and infiltration, often intoxication and fever.
Without an exacerbation of the inflammatory reaction, the fistula can be felt as a cord. The size of the compaction around the fistula tract is due to inflammatory infiltration and branching of the fistula tracts themselves, cicatricial changes in the surrounding tissues, previously involved in the inflammatory conglomerate.
A formed fistula has an entrance and, sometimes, an exit, the tissues around it are compacted, and discharge can be squeezed out of the hole: pus, bile, pancreatic juice, and so on. With a fistula, feces may leak from the intestine into the vagina from the genital organs; when there is an anastomosis of the intestine with the bladder, urine leaks from the anus. The discharge from the intestinal fistula has a fecal smell, and the purulent secretion from the vagina also has a specific smell. The smell of a discharged fistula, leading from the zone of disintegration of a malignant tumor, seems especially heavy to others.
Inflammation causes pain ranging from slight discomfort to unbearable pain. Tumor fistulas do not hurt because they form inside a disintegrating tumor.
When the infection activates with the formation of streaks of purulent contents, a general reaction occurs: intoxication, high temperature, sweating and pallor, palpitations and rapid breathing.
Purulent fistula on a surgical suture - treatment
Treatment of purulent fistula
- As you probably already understood, a purulent fistula is not a death sentence and, with proper treatment, almost always responds quite well to treatment. But still, in most cases, surgery is usually required for a favorable outcome.
- If the doctor decides to delay the intervention, the patient will be prescribed conservative treatment. But it should also be carried out under the strict supervision of a specialist and preferably in a hospital setting. Typically, such treatment is aimed at eliminating pathogenic microflora that provokes inflammation
- If the therapy is chosen correctly, the fistula opening will heal fairly quickly and the patient will be able to return to normal life. To treat an inflamed area of skin, drugs that have antiseptic, antibacterial and bactericidal effects are usually used
- In addition, the patient must be prescribed antibiotics and vitamins, which help maintain the body’s defenses at a normal level. But I would like to immediately say that conservative treatment does not provide a 100% guarantee that the fistula will not reopen. Therefore, most doctors suggest not to suffer and immediately perform surgery to remove the purulent focus
Only surgical intervention can help completely get rid of the fistula.
- After washing the wound, drainage is usually installed in it. In the postoperative period, the drainage is washed daily and sterile dressings are changed. If after a few days the amount of purulent masses does not begin to decrease, then the patient is additionally prescribed anti-inflammatory drugs, antibiotics and vitamin E
- In addition, bandages and ointments can be used to stimulate the healing process. In this case, for example, troxevasin ointment may be prescribed. As soon as the purulent ceases to be released, the drainage is removed from the wound and then the patient can only make sure that no infection gets into it and periodically change the bandage
Diagnostic methods
Diagnosis of a simple unbranched single-channel fistula is not difficult - it is enough to feel a cord in the local seal, from which contents can leak when pressed.
All external exits of the fistula are examined with a button probe, this is how the localization of the passages is determined. The probe is inserted from the side of the skin, carefully pushing it all the way; if a rectal fistula is being examined, then the passage of the probe inside the rectum is determined with the index finger.
Next, a test is carried out with a dye - methylene blue, which is injected into the outer hole with a syringe. In case of rectal fistula, a cotton swab is inserted into the intestine before the test, and the exact location of the internal opening is determined by the dye marks on it.
For any fistula, the paint output can be recorded during endoscopy: anoscopy, rectoscopy, colonoscopy, cystoscopy, colposcopy, and so on. Endoscopic examination is one of the leading ones and is performed repeatedly in the process of diagnosis and treatment.
In some cases, fistulography is performed - an x-ray of the anatomical area before and after the injection of a contrast agent into the fistula. The procedure is not required only for simple and short rectal fistulas without exacerbation of inflammation.
Imaging methods - CT and MRI also make it possible to clarify the localization of tracts and leaks, branching and the root cause of the disease.
When the rectum is involved, ultrasonography (ultrasound) with a special rectal sensor is informative, when a computer program allows you to see the pathology in a three-dimensional image. When planning the operation, the function of the anal sphincter is additionally determined.
| Examination stage | Techniques | What are they used for? |
| Techniques used in the doctor's office during the initial examination |
|
|
| Lab tests |
|
|
| Instrumental studies |
|
|
Ointment for the treatment of postoperative fistula
Ointment with calendula for healing fistulas.
Home-made ointments have also proven themselves to be quite effective. They eliminate the cause of the infection quite well and contribute to a faster restoration of the dermatological integument. But even in this case, it is extremely important to be very careful when applying the ointment, as well as pre-treatment of the wound.
You need to protect yourself from re-infection of the fistula opening. After all, if you apply unsterile dressings and use a product of questionable quality, you are unlikely to improve your condition.
The most popular ointments:
- At home, you can also use an ointment that will have anti-inflammatory and healing properties. To prepare it, you will need pine resin, natural honey, butter, aloe pulp and medical tar. All ingredients are mixed in equal parts and brought to homogeneity in a water bath. The resulting product should be applied to previously disinfected areas of the skin.
- Another effective remedy is ointment made from fresh calendula flowers. They need to be tightly folded into a half-liter jar and filled with melted pork fat or butter. Leave the product in a dark place to brew for 10-12 hours. Then transfer it to a clay pot and simmer for 48 hours in the oven at 70 degrees. After the ointment has cooled, transfer it to a container with an airtight lid and store in a cool, dark place. You can simply lubricate the fistula opening with the resulting product or make medicinal dressings from it.
Methods for treating fistulas
Fistulas rarely close on their own; this can only be hoped for by creating favorable conditions, for example, limiting and partially controlling the movement of feces through the rectum using cleansing enemas. In the vast majority of cases, conservative therapy is ineffective; the only radical treatment is surgical, that is, excision of the pathological area, including reconstruction of the missing tissue.
Technically simple surgical intervention, including endoscopic, and a hundred surgical modifications cannot cure about half of the patients who suffer from relapses. It is especially difficult to achieve success with intestinal and urinary fistulas, since they are always contaminated with microflora. In some cases, it is necessary to resort to the formation of an intestinal stoma, temporarily stopping the movement of feces through the pathologically changed area of the intestine for several months.
In isolated cases, they resort to “old-fashioned methods” of treatment with scraping the mucous membrane of the tract, burning it with chemical reagents and enzymes, achieving sticking of the walls. Better results - in approximately 50% - are achieved by introducing fibrin glue into the fistula tract, which glues the walls together.
Tampons made of biomaterials act similarly to glue, sealing the internal opening; emptying of the passage can cause the walls to stick together and close the fistula.
Until now, the role of antibiotics in the treatment of fistulas caused by inflammation has not been determined, since drugs are not able to penetrate into the infiltrate due to massive scar changes. However, with fistula tracts due to Crohn's disease, specific drug therapy is mandatory and not unsuccessful.
Surgery for fistulas using the LIFT method
Why are ligature fistulas dangerous?
Since the thread in the case of a fistula becomes a source of chronic infection, the fistula leads to intoxication of the body, impaired immune reactions, and, in the early period, to suppuration of the wound and failure of the sutures. Treatment of ligature fistulas
- conservative
- Washing the wound with antiseptics, taking antibiotics, vitamins, immunomodulators, and anti-inflammatory drugs helps cope with fresh ligature fistulas. Minimally invasive techniques are also used: cauterization of excess granulations with an electrocoagulator and laser, ultrasound treatment of fistulas.
- surgical
If a patient has a long-existing ligature fistula, it is treated surgically, the same can be said in case of complications from the wound (suppuration, suture dehiscence). In this case, the ligatures are removed, the edges of the wound are refreshed, fibrous tissues and excess granulations are removed and new sutures are applied using sterile atraumatic synthetic material with different resorption times.
Prevention of fistulas
Not all diseases can be prevented, especially fistulas, which complicate the course of purulent paraproctitis. However, it is possible to adequately treat the diseases that lead to paraproctitis - hemorrhoids and fissures, and this is precisely what will prevent the formation of fistulas.
Complicated childbirth cannot be prevented, but high-quality and timely obstetric care, attentive attention to the woman and a thorough postpartum examination are available preventive measures.
The high incidence of post-radiation tissue damage and fibrosis progressing over time forced oncologists to abandon high doses of radiation therapy and even change approaches to the treatment of malignant tumors of the genital area.
Particular importance is attached to the correct choice of method of surgical treatment of diseases of the hollow organs and adequate management of the postoperative period.
In our clinic, a complicated course of the disease is very rare, because we not only know about prevention methods, but also actively use them.
| Price : | |
| Primary consultation with a surgeon | 5100 rub. |
| Repeated consultation with a surgeon | 4600 rub. |
| Consultation with a surgeon Ph.D. | 6900 rub. |
| Primary consultation with an oncologist | 5100 rub. |
| Repeated consultation with an oncologist | 4600 rub. |
| Consultation with oncologist Ph.D. | 6900 rub. |
| Consultation with an oncologist, MD. | 10500 rub. |
| Fistulography | 41800 rub. |
Book a consultation 24 hours a day
+7+7+78
Bibliography:
- Shelygin Yu.A., Blagodarny L.A. /Handbook of coloproctology// -M.: Litterra; 2012.
- Becker A., Koltun L., Sayfan J. /Simple clinical examination predicts complexity of perianal fistula// Colorectal Dis.; 2006; 8.
- Gaertner WB, Hagerman GF, Finne CO, et al. /Fistula-associated anal adenocarcinoma: good results with aggressive therapy// Dis Colon Rectum; 2008; 51.
- Genadry RR, Creanga AA, Roenneburg ML, Wheeless CR /Complex obstetric fistulas // Int. J. Gynaecol. Obstet.; 2007; Vol. 99; Suppl. 1.
- Ommer A., Herold A., Berg E. / S3-Leitlinie: Rektovaginale Fisteln (ohne M. Crohn) // Coloproctology; 2012; Vol. 34.
- Sahni VA, Ahmad R., Burling D. / Which method is best for imaging of perianal fistula?// Abdom Imaging.; 2008; 33.
- Zoulek E., Karp DR, Davila GW/ Rectovaginal fistula as a complication to a Bartholin gland excision // Obstet. Gynecol.; 2011; Vol. 118; N 2.