Urinary tract infections are a common disease in everyday urological practice. Significant progress in the treatment of urinary tract infections has been observed over the past twenty years. The article touches upon such important issues as the etiology, pathogenesis and treatment of urinary tract infections in adults.
Urinary tract infections (UTIs) are a serious problem due to their prevalence and associated morbidity. According to statistics, they account for approximately 20% of all community-acquired and approximately 50% of nosocomial infections. Advances in recent decades have contributed to a better understanding of the pathogenesis of urinary tract infections and have elucidated the important role of both bacterial and patient-related factors in the development or prevention of infection.
The dynamic development of antibacterial therapy has greatly facilitated the correct treatment of UTIs, but the inappropriate and widespread abuse of antibacterial drugs has led to an increase in drug resistance of microorganisms.
Epidemiology of UTIs
The content of the article
Urinary tract infections are one of the most common infectious diseases in humans.
The incidence of UTI depends on the sex and age of the subjects, as well as on the specific characteristics of the study population.
- In the neonatal period, UTI is detected in approximately 60% of cases in boys, which is associated with a higher incidence of congenital urinary tract defects.
- From the age of three months, this trend is reversed, and the incidence of urinary tract infections in girls and women is ten times higher than in their male counterparts.
- Every second woman suffers from cystitis at least once in her life, and 10% of sexually active women develop UTIs once a year.
- Urinary tract infections are rare in men under 50 years of age, but in patients over 60 years of age the number of reported cases is growing rapidly. This is associated with the appearance of bladder obstruction, most often in the form of benign prostatic hyperplasia.
- The incidence of UTIs is much higher among people hospitalized for any reason or living in nursing homes or nursing homes.
Benign Prostatic Hyperplasia
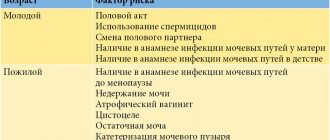
The risk of UTI increases when there is an obstruction to the flow of urine or when circumstances favor bacterial colonization and growth. Physiological factors that predispose to UTIs include pregnancy, old age, and medical conditions such as diabetes and urolithiasis.
Etiology and pathogenesis of UTI
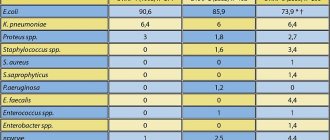
The most common causes of UTIs are bacteria, and less commonly viruses, fungi, or parasites. The prevalence of certain types of bacteria isolated from patient urine depends largely on the population being studied. The situation is completely different for patients receiving outpatient treatment than for patients in hospitals.
Under physiological conditions, the urinary tract is sterile except at the end of the urethra. The first episode of UTI in an outpatient setting is caused by Escherichia coli in 80% of cases, Staphylococcus saprophyticus in 10-15% (except for the group of young sexually active women, in which it accounts for about 30%), other gram-negative bacteria (Proteus mirabilis, Klebsiella spp.) or gram-positive (staphylococci, streptococci, enterococci). 70% of recurrent community-acquired infections are caused by Escherichia coli. Also, the most common nosocomial infections are caused by Escherichia coli (about 50%), Enterobacter spp., Pseudomonas spp., Serratia marcescens, as well as staphylococci, enterococci and fungi.
Escherichia coli
In 95% of patients, a UTI is the result of infection with a single strain of bacteria. Infection with several strains is observed in 5% of patients, mainly in catheterized patients with weakened immunity, neurogenic bladder disorders or defects of the urinary system.
Infection of the urinary system can occur through the ascending route (urogenic infections), the bloodstream (hematogenous infections - very rarely caused mainly by Staphylococcus aureus), the lymphatic route, or continuously (in the presence of a urogenital or urogenital fistula).
A UTI is almost always caused by bacteria entering the urethra. Under physiological conditions, bacteria often enter the urinary tract, but due to the body's defense mechanisms, the development of UTIs is rare.
The most important natural defense mechanisms against UTIs are:
- length of the urethra in men;
- ureteral peristalsis, normal function of vesicoureteral valves;
- acidification and concentration of urine;
- correct bacterial flora of the vagina and area around the urethra;
- antibacterial properties of prostate secretion;
- mechanisms for preventing bacterial adhesion in the urinary tract: mechanical impact of a stream of urine, mucopolysaccharides of the bladder wall, IgG and IgA antibodies.
Urinary tract infections rarely occur in healthy people with normal anatomical structure and physiological function of the urinary tract. In case of obstructed urine outflow or weakening of the body due to systemic diseases (diabetes, gout, tumor process), we often encounter inflammatory changes in the urinary system.
Gout
The most common factors contributing to the development of a urinary tract infection include:
- 1st pregnancy,
- old age,
- obstruction to the outflow of urine - urolithiasis, prostate adenoma,
- atrogenic factors - urinary tract instrumentation (cystoscopy, bladder catheterization, ascending pyelography),
- congenital malformations of the urinary tract - double cup-pelvic system, retrograde vesicoureteral outflow,
- diabetes, gout,
- neurogenic bladder,
- end-stage renal failure (dialysis),
- sexual relations,
- prolonged immobilization in bed.
Urine in the urinary tract of a healthy person is sterile. The presence of bacteria in it indicates infection.
The main symptom for diagnosing a UTI is the so-called significant bacteriuria, when the number of bacteria in 1 ml of fresh, aseptically collected urine exceeds 100,000.
The occurrence of significant bacteriuria by gender and age is presented below:
| Age | women | Men |
| School age | 1% | 0,03% |
| 15-25 years | 3% | 0,5% |
| 30-35 years | 5-10% | up to 1% |
| 50-70 years | > 10% | up to 4% |
| over 80 years old | > 20% | > 10% |
In people with dysuria, the presence of up to 100 bacteria may indicate a urinary tract infection. Treatment for UTIs should begin as soon as clinical symptoms appear.
Tasks of a urologist:
- fight against bacteriuria,
- refusal of instrumentation of the urinary tract - bladder catheterization,
- proper treatment of systemic diseases.
General principles of treatment of urinary infections
- Antibacterial treatment.
- When choosing a drug and method of its use, the following are taken into account:
- drug sensitivity of the bacterial strain;
- patient tolerability of the drug;
- severity of infection;
- medical expenses.
- Symptomatic treatment depending on the type of disease:
- bed rest;
- regular and complete emptying of the bladder;
- painkillers, antispasmodics;
- fluid intake (diuresis more than 1.5 liters per day);
- refusal of nephrotoxic drugs.
Fluid intake
The main goal of antimicrobial treatment is to eliminate pathogenic bacteria and prevent recurrent UTIs. Treatment procedures are differentiated depending on the severity of the infection and the sensitivity of the bacteria to the drugs used.
We now have a number of medications that are particularly useful in treating UTIs. These include antibiotics, fluoroquinolones, chemotherapeutic agents (eg, Bactrim, Urotrim, Bispetol) and herbal preparations.
The basic principle of antimicrobial treatment is to perform an antibiogram of bacteria growing from the inflamed area and carry out targeted treatment. In the case of acute infections with unpleasant signs, high fever and general symptoms, urologists prescribe broad-spectrum antibiotics that act on gram-negative bacteria as first-line drugs. In these cases, the use of fluoroquinolones is increasingly recommended.
The patient must submit urine for bacteriological analysis and antibiogram before starting treatment, as well as 2, 14, 30 days after starting treatment. If urinary sepsis is suspected during the peak of fever, blood is taken for culture and antibiogram, and additional treatment with two broad-spectrum antibiotics is started.
Antibioticogram
MAIN PATIENTS
Uncomplicated infections
MVP in more than 95% of cases is caused by a single microorganism, most often from the
Enterobacteriaceae
.
The main pathogen is E.coli
- 80-90%, much less often
S.saprophyticus
(3-5%),
Klebsiella
spp.,
P.mirabilis
, etc. With
complicated UTI infections
E.coli
isolation decreases, other pathogens are more common -
Proteus
spp.,
Pseudomonas
spp.,
Klebsiella
spp., mushrooms (mainly
C.albicans
).
Renal carbuncle (cortical abscess) is 90% caused by S.aureus
.
The main causative agents of apostematous pyelonephritis, kidney abscess localized in the medullary substance are E. coli, Klebsiella
spp.,
Proteus
spp.
As with other bacterial infections, the sensitivity of pathogens to antibiotics is critical when choosing a drug for empirical therapy. In Russia, in recent years, there has been a high frequency of resistance of community-acquired E. coli
to ampicillin (uncomplicated infections - 37%, complicated - 46%) and co-trimoxazole (uncomplicated infections - 21%, complicated - 30%), therefore these AMPs cannot be recommended as drugs of choice for the treatment of UTI infections. The resistance of uropathogenic strains of Escherichia coli to gentamicin, nitrofurantoin, nalidixic acid and pipemidic acid is relatively low and amounts to 4-7% for uncomplicated and 6-14% for complicated MVP. The most active are fluoroquinolones (norfloxacin, ciprofloxacin, etc.), the level of resistance to which is less than 3-5%.
Classification of urinary tract infections
Depending on the location of the infection, the age of the patient, the severity of symptoms and the presence of additional diseases, the following classification of UTIs has been proposed:
Depending on the severity of clinical symptoms:
- Symptomatic urinary tract infections.
A. simple - in people without aggravating factors:
- acute inflammation of the lower urinary tract;
- recurrent inflammation of the lower urinary tract;
- acute pyelonephritis.
Acute pyelonephritis
b. complex - in people with aggravating circumstances:
- acute inflammation of the lower urinary tract;
- recurrent inflammation of the lower urinary tract;
- acute pyelonephritis.
- Asymptomatic bacteriuria:
A. in patients without additional risk factors;
b. in patients with additional risk factors.
Depending on the location of the infection:
- Infections of the upper urinary tract: kidneys, vesico-pelvic system, perinephric area.
- Infection of the lower urinary tract: bladder, urethra.
Asymptomatic bacteriuria
Most often it is discovered by chance during routine periodic examinations, since there are no subjective symptoms prompting the patient to seek medical help, and no noticeable changes in the urinary system are detected.
In the absence of concomitant disturbances in the outflow of urine, the course is usually mild and does not require treatment. In patients with urinary tract obstruction, symptoms usually do not resolve spontaneously. Antibacterial treatment is recommended for this group of patients.
Additionally, treatment should be started in the following cases:
- pregnancy (risk of pyelonephritis, premature birth, low birth weight of the newborn);
- before planned surgery (mainly on the urinary tract);
- diabetes.
In the first trimester of pregnancy, an antibiogram should always be performed before starting treatment for a UTI.
Acute pyelonephritis
Bacterial nonspecific inflammation of the renal system. The infection is mainly caused by Escherichia coli or other gram-negative bacilli: Klebsiella spp., Proteus vulgaris. It most often occurs in girls over 5 years of age and in women before menopause.
In the case of pyelonephritis, the following is observed:
- sudden onset;
- fever (up to 40 ° C);
- chills;
- pain in the lumbar region (positive Goldflam sign on this side);
- nausea, vomiting;
- increased ESR, peripheral blood leukocytosis;
- in urine: numerous bacteria, leukocytes, leukocyte cells, protein, red blood cells.
Nausea with pyelonephritis
In case of AP, in addition to urine analysis and culture, abdominal ultrasound and urography (after the disappearance of acute symptoms) should always be performed to visualize disturbances in the outflow of urine.
Patients with mild acute pyelonephritis can be treated on an outpatient basis. In severe cases, patients must be hospitalized. Initially, medications are used parenterally. Only 24 hours after the fever has disappeared, they can be administered orally.
Hospitalization of patients with acute pyelonephritis is carried out in the following cases:
- severe infection;
- no improvement after 2 days of targeted antibiotic therapy;
- difficult outflow of urine, mainly in older people and patients with diabetes;
- pregnancy.
If fever and low back pain persist after 3 days of treatment, repeat urine culture and repeat abdominal ultrasound to look for peri- or intrarenal abscess or previously unrecognized hip joint abnormalities.
The most common complications of acute pyelonephritis include chronic pyelonephritis, urinary tract sepsis, hydronephrosis, perirenal abscess, renal papillary necrosis, and scarring of the renal cortex.
Chronic pyelonephritis most often affects women. It is characterized by an insidious onset, a long, rarely symptomatic course with periodic exacerbations. Often leads to kidney failure.
A few words about the urinary system of a healthy person
Urine, which is one of the waste products of our body, is formed and accumulated in the organs of the urinary system. Urine is produced in the kidneys and passes down the ureters to the bladder. The bladder serves as a reservoir for storing urine, which is then emptied through the urethra. The urethra ends at the penis in men and the area above the vagina in women.
The kidneys are a pair of fist-sized organs located in the lumbar region that serve as a filter for the body, removing waste products from the blood in the form of urine. The kidneys also regulate the balance of various chemicals in the body (sodium, potassium, calcium, phosphorus, etc.) and control the acidity of the blood. The kidneys produce several hormones that help regulate blood pressure, stimulate the production of red blood cells, and promote the development of strong bones.
The ureters are two muscular tubes that transport urine to the bladder.
Normal urine is sterile and free of bacteria. However, bacteria can enter the urine from the urethra and then travel to the bladder.
Cystitis - inflammation of the bladder
Acute cystitis in people under 50 years of age applies only to women. This is an inflammation of the mucous membrane, sometimes of the deeper layers of the bladder wall.
Cystitis
Symptoms:
- sudden onset;
- symptoms of bladder irritation (pollakiuria, urge, painful urination);
- pain above the pubic joint;
- red blood cells, white blood cells and numerous bacteria are found in the urine.
Young women with dysuria usually develop one of three types of infection: inflammation of the bladder, urethra, or vagina. These diseases are differentiated based on clinical symptoms and laboratory urine test results.
| Diagnosis | Piuria | Hematuria | Bacteriuria |
| Cystitis | usually | Sometimes | From 100 to 100 thousand |
| Urethritis | usually | rarely | up to 100 |
| Vaginitis | rarely | rarely | up to 100 |
With vaginitis, there is discharge, itching in the vagina, pain during sexual intercourse, but there is no pollakiuria or painful urge to urinate.
Treatment of cystitis should be carried out from 3 to 7 days. In the uncomplicated form, the effectiveness of 3-day treatment is the same as that of 7-day treatment, but fewer side effects were found.
Urologists use longer treatment in women with the following conditions:
- pregnancy, diabetes;
- symptoms last more than 7 days;
- vaginal contraception;
- age over 65 years.
Urethritis
Most often, the disease is associated with sexual contact, catheterization or endoscopy of the bladder. Urethritis always occurs in patients with an indwelling urinary catheter. The opening of the urethra is red, patients complain of a number of symptoms:
- burning pain and itching in the urethra;
- leakage of mucous, glassy or purulent discharge;
- lower abdominal pain.
Until recently, the most common cause of urethritis was gonorrhea. The infections are now twice as likely to be caused by Chlamydia trachomatis and Ureoplasma urealyticum. In 30% of cases, gonorrhea infection coexists with two others.
Urethritis
Standard urine cultures are often sterile, followed by immunological tests and isolation of microorganisms on specially prepared media.
The most common treatments are a single dose of fluoroquinolones and doxycycline for 7 days.
Antimicrobial prophylaxis
Patients with recurrent UTIs associated with sexual intercourse are recommended to take the drug after coitus. With this prevention regimen, the dose of the drug, the incidence of adverse reactions, and the selection of resistant strains are reduced;
The decision to prescribe ABT should be made after a detailed discussion with the doctor if behavioral therapy and non-antimicrobial prophylaxis measures are ineffective.
The rate of synthesis of new antibacterial and antimicrobial agents is significantly lower than the rate of development of antibiotic resistance. Prevention of recurrent UTIs is often ineffective or even dangerous, leading to an even greater increase in resistant strains of bacteria and the occurrence of adverse reactions. Alternative methods of treating infectious diseases of the urinary system can rightfully include virulent bacterial viruses (bacteriophages). A review of publications in recent years indicates a significant increase in interest in phage therapy for infections of the urinary system. The use of the phage typing technique will make it possible to use bacteriophages as a therapy for recurrent UTIs, as well as in patients undergoing hospital treatment who have been exposed to aggressive nosocomial flora. Bacteriophages are safe for patients who need UTI prevention. The species-specific action of phages ensures the stability of the intestinal flora.
Recurrent urinary tract infections
Recurrent UTIs are caused by the same pathogen as the first case, usually within 2 weeks after stopping treatment. Mostly relapse occurs in women, and most often it is inflammation of the bladder. After the first episode of urinary tract infection, approximately 20% of UTIs are rediagnosed within one year.
Causes of recurrent urinary tract infections include:
- incorrectly selected drug;
- route of administration, dosage, duration of treatment;
- obstruction to the flow of urine.
In treatment, urologists recommend constant use of antibacterial drugs and prophylaxis after sexual intercourse. For urinary tract infections less than twice a year, only episodes of infection are treated.
When infection occurs more than 3 times a year and is not associated with sexual intercourse, the drugs are administered daily or 3 times a week at night, while in the case of infection associated with sexual intercourse, the drugs are administered once immediately after sexual intercourse.
Treatment for 3–6 months reduces the incidence of urinary tract infections by up to 5–10%.
Introduction
Urinary tract infection (UTI) is a term used to describe a bacterial infection of the urinary system. The most common agent of UTI is E. coli
(85% of community-acquired and 50% of nosocomial UTI cases), less common are
Proteus spp.
,
Klebsiella spp.
,
Enterococcus faecalis
,
Staphylococcus saprophyticus
.
UTIs can also be caused by Chlamydia trachomatis
,
Mycoplasma hominis
,
S. aureus
,
S. epidermidis
,
S. saprophyticus
,
Haemophilus influenzae
,
Candida albicans
[1].
UTIs spread throughout the body:
urethral (ascending) route;
downward path;
hematogenous or lymphogenous route;
directly from foci of infection located near the organs of the genitourinary system.
The main risk factors for UTI include:
unprotected sexual intercourse;
surgeries or invasive diagnostic procedures;
diabetes;
elderly age;
use of a diaphragm, cervical cap, spermicidal gels.
In hospital settings, infection most often occurs when using urinary catheters [2].
Traditionally, complicated and uncomplicated UTI are clinically distinguished (Table 1).
The problem of UTI in urology has always been extremely relevant and remains in the field of view of specialists all over the world. In an era of increasing microbial resistance, adequate and rational prescription of antimicrobial drugs is of particular importance for the cure of a urological patient. The cost of diagnosis and treatment of bacterial UTIs is a major factor influencing healthcare costs today. The total economic burden consists of the costs of outpatient and inpatient treatment [2, 4]. The urinary tract is the most common site of nosocomial infection, with approximately 40% of nosocomial infections reported in acute care hospitals being urinary tract infections. The vast majority of hospital-acquired infections are associated with indwelling catheters. On average, a hospital-acquired UTI increases a patient's length of stay by 1 bed day, resulting in nearly a million additional days in the hospital. More than 100,000 hospitalizations per year are associated with urinary tract infections [5]. Uncomplicated cystitis, in particular, is the most common outpatient infection, while pyelonephritis accounts for the majority of hospitalizations.
Sources
- Schaeffer A.: Urinary tract infections. Campbell Urology, 1992.
- Naber K.G. et al.: Recommendations for the treatment of urinary tract and male genital tract infections, 2000.
- Grinevich V. et al.: Urinary tract infections. Urological review, 2000.
- Safir MH et al.: Urinary tract infections: simple and complex, 1998.
- Eichman V.: Treatment of bacterial infections of the genitourinary system. Urological Review, 2000.
- Macfarlane MT: Urinary Tract Infections, 1997.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
Why are cystitis and urethritis dangerous?
The main danger of cystitis and urethritis is the transition to a chronic form in the absence of timely treatment. Chronic inflammatory process of the urinary tract is a problem that will require multiple courses of treatment and periodically remind itself for many years. The chronic form of the disease creates conditions for the emergence of microbial colonies that are resistant to popular antibiotics, which makes treatment in the future even more difficult.
Another danger of these diseases is the vertical progression of infection, which ends in kidney damage. As a result, pyelonephritis develops - an acute, often purulent, inflammation of the kidney tissue. Therefore, at the first signs of possible inflammation of the urinary tract, you should consult a doctor. Any self-medication is more likely to increase the chances of getting a chronic form of the disease than to recover without visiting a doctor. In addition, different diseases of the genitourinary system have similar symptoms, but require different approaches to therapy. Treatment without a diagnosis confirmed by a specialist can lead to self-selected medications being ineffective. For example, urethritis can be easily confused with inflammation of the prostate due to similar symptoms: both diseases are manifested by painful and frequent urination.