Pharmacodynamics and pharmacokinetics
This substance inhibits the processes of synthesis of deoxyribonucleic and ribonucleic acids , proteins, reduces membrane permeability and the intensity of aerobic metabolism of harmful bacteria. The medicine has a wide spectrum of action, the drug is effective against gram-negative or gram-positive bacteria . The drug inhibits the vital functions of: streptococci , staphylococci , Shigella dysenteriae , Shigella boydii , Escherichia coli , Shigella flexneri , Shigella sonnei , Proteus spp .
The medicine has a high absorption capacity. After penetration of the substance into the gastrointestinal tract, the bioavailability of the product is about 50%. Eating increases the bioavailability of the substance. The smaller the crystals of a chemical compound, the better they dissolve and penetrate into the systemic bloodstream. The microcrystalline form is absorbed faster and reaches maximum concentration in urine in a shorter period of time. About 60% binds to blood plasma proteins. The substance undergoes metabolism in the liver and muscle tissues. The half-life is 20 to 25 minutes.
The drug crosses the blood-brain barrier, penetrates the placenta, and is excreted in breast milk. The drug does not accumulate in the body and is completely eliminated by the kidneys, about 40% unchanged.
Pharmacological properties of the drug Nitrofurantoin
Synthetic antimicrobial agent, a derivative of nitrofuran. It has a bacteriostatic effect, but can also act bactericidal depending on the concentration and sensitivity of microorganisms. Disturbs the synthesis of DNA, RNA and protein in bacterial cells. Resistance of microorganisms to nitrofurantoin rarely develops. Nitrofurantoin is active against several Gram-positive bacteria, including Staphylococcus aureus, S. saprophyticus , coagulase-negative staphylococci (eg, S. epidermidis ), Enterocuccus faecafis, Streptococcus agalactiae, group D streptococci, Streptococcus viridans , and Corynebacterium spp. Nitrofurantoin is also active against many gram-negative bacteria, such as Citrobacter anomalonaticus, C. diversus, C. freundii, Klebsiella oxytoca, K. ozaenae, Enterobacter spp., Escherichia coli, Neiserria spp., Salmonella spp., Shigella spp . Nitrofurantoin is well absorbed from the digestive tract. Simultaneous food intake increases the degree of adsorption of nitrofurantoin. Nitrofurantoin is 20–60% bound to plasma proteins. Penetrates through the placenta and into breast milk. The half-life is about 20 minutes. In patients with impaired liver function, the concentration of nitrofurantoin in the body is higher and its half-life is longer. Nitrofurantoin is partially metabolized in the liver. The maximum concentration of nitrofurantoin in the blood serum after oral administration is achieved within 30 minutes.
Indications for use
The drug is prescribed:
- for the treatment of urinary tract infections caused by organisms sensitive to the active substance ( pyelitis , cystitis, urethritis, pyelonephritis );
- as a prophylactic agent during catheterization, cystoscopy and other urological studies and operations.
Contraindications
The medicine is contraindicated:
- with severe disturbances in kidney function;
- patients with chronic renal or heart failure stages 2 and 3;
- with oliguria ;
- pregnant women;
- with glucose-6-phosphate dehydrogenase ;
- children under 1 month;
- if allergic to the active substance;
- persons suffering from chronic hepatitis or cirrhosis of the liver ;
- for acute porphyria ;
- while breastfeeding.
Particular care must be taken in the presence of fibrotic changes in the lungs and in patients with bronchial asthma .
Furadonin tab 0.05 No. 10 (nitrofurantoin)
Full description
[RU]
Tradename
Furadonin
International nonproprietary name
Nitrofurantoin
Dosage form
Tablets 50 mg
Compound
One tablet contains:
active substance – nitrofurantoin (furadonina) – 50 mg;
excipients: colloidal anhydrous silicon dioxide, calcium stearate, potato starch.
Description
Flat-cylindrical tablets of yellow or greenish-yellow color, with a chamfer.
F armacotherapy group
Antibacterial drugs for systemic use. Other antibacterial drugs. Nitrofuran derivatives. Nitrofurantoin.
ATX code J01XE01
Pharmacological properties
Pharmacokinetics
Furadonin is well absorbed in the upper gastrointestinal tract and is quickly excreted in the urine. The half-life is about 30 minutes. Maximum urinary excretion occurs 2–4 hours after taking furadonin; the proportion of unchanged drug is about 40–45%. Penetrates the blood-brain barrier, placental barrier, and is excreted in breast milk.
Pharmacodynamics
A synthetic broad-spectrum antimicrobial agent. Acts bactericidal.
The mechanism of action is associated with the restoration of furadonin into an active intermediate that damages ribosomal proteins and disrupts the synthesis of protein, DNA, and RNA. In high doses, it disrupts the permeability of the bacterial cell membrane.
Active against gram-positive aerobic bacteria: Staphylococcus spp., Streptococcus spp.; gram-negative aerobic bacteria: Escherichia coli, Enterobacter spp., Klebsiella spp., Shigella spp. Weakly active against Enterococcus spp., fungi of the genus Candida. Not active against Pseudomonas aeruginosa, Acinetobacter spp.
Most strains of Proteus and Serratia are resistant to furadonin.
Indications for use
- uncomplicated urinary tract infections (acute cystitis, asymptomatic bacteriuria, urethritis, pyelitis, pyelonephritis);
— prevention of infections during urological operations and examinations (cystoscopy, catheterization).
Directions for use and doses
Take orally, during meals, with plenty of water.
Adult patients
Acute uncomplicated urinary tract infections: 50 mg four times daily for seven days. Severe recurrent infection: 100 mg four times daily for seven days.
Long-term maintenance therapy: 50 mg – 100 mg once daily.
Prevention: 50 mg four times a day for urological operations and examinations and 3 days after them.
Children over 6 years old
Acute uncomplicated urinary tract infections: 3 mg/kg/day in four divided doses for seven days. Maintenance therapy: 1 mg/kg once daily.
For children weighing less than 25 kg, it is recommended to use the drug in the form of a suspension.
Side effects
From the gastrointestinal tract: nausea, vomiting, lack of appetite, abdominal pain, diarrhea, pancreatitis, pseudomembranous colitis.
From the liver and biliary tract: cholestatic jaundice, cholestatic syndrome, chronic active hepatitis (sometimes fatal, usually with long-term therapy). If symptoms of hepatotoxicity appear, the drug should be discontinued.
From the nervous system: headache, drowsiness, dizziness, depression, euphoria, nystagmus, confusion, psychotic reactions, intracranial hypertension. In rare cases, severe and even irreversible peripheral neuropathy (including damage to the optic nerve) with symptoms of sensory and motor disorders. If the symptoms mentioned above occur, the drug should be stopped.
From the respiratory system: acute pulmonary reactions (usually develop during the first week of treatment and are reversible after discontinuation of the drug) are characterized by the sudden onset of fever, eosinophilia, cough, chest pain, shortness of breath, the formation of pulmonary infiltrate, pleural effusion.
Chronic pulmonary reactions are rare, occurring in patients who have received long-term therapy for 6 months or more, more often in elderly patients. The degree of severity depends on the duration of treatment after the first clinical symptoms. ECG changes associated with pulmonary reactions may occur, rarely - cyanosis, collapse. Loss of lung function may be irreversible.
When the first signs of a respiratory system disorder appear, the drug should be stopped.
From the skin and subcutaneous tissue: hypersensitivity reactions - skin rashes, maculopapular rash, urticaria, itching in some cases: angioedema, anaphylaxis, inflammation of the salivary glands, eczema, exfoliative dermatitis, erythema multiforme (including Stevens-Johnson syndrome), lupus-like syndrome .
From the hematopoietic and lymphatic systems: leukopenia, granulocytopenia or agranulocytosis, thrombocytopenia, megaloblastic anemia, aplastic anemia, hemolytic anemia in patients with glucose-6-phosphate dehydrogenase deficiency.
From the musculoskeletal system: arthralgia.
Other: reversible alopecia, superinfection (usually caused by Pseudomonas aeruginosa or fungi), urine staining dark yellow or brown.
Contraindications
- hypersensitivity to nitrofurantoin or nitrofurans;
- severe renal dysfunction, renal failure, oliguria (creatine clearance less than 60 ml/min);
- children under 6 years of age;
- liver cirrhosis, chronic hepatitis;
— chronic heart failure (NYHA class III-IV);
- deficiency of glucose-6-phosphate dehydrogenase;
- acute porphyria.
- pregnancy and lactation due to possible hemolytic anemia in the fetus or newborn due to the immaturity of erythrocyte enzyme systems.
Drug interactions
The absorption of furadonin is increased when taken with food or with medications that cause delayed gastric emptying.
Magnesium trisilicate reduces the absorption of furadonin.
Probenecid and sulfinpyrazone reduce the renal excretion of furadonin.
Corboanhydrase inhibitors and agents that cause an alkaline reaction in urine reduce the antibacterial activity of furadonin.
Furadonin and antimicrobial agents from the fluoroquinolone group are antibacterial antagonists.
Furadonin can suppress intestinal flora, which leads to a decrease in estrogen absorption and the effectiveness of estrogen-containing contraceptives. Patients are recommended to use non-hormonal methods of contraception.
Furadonin may inactivate the oral typhoid vaccine.
Nitrofurantoin weakens the antibacterial effect of norfloxacin in the urinary tract; simultaneous use is not recommended.
special instructions
The drug should be discontinued at the first signs of peripheral neuropathy (paresthesia), because the development of this complication can be life-threatening.
It is necessary to stop treatment with furadonin if unexplained symptoms of impaired pulmonary function, liver function, hematological and neurological disorders occur.
If signs of lung damage appear, furadonin should be stopped immediately. Careful monitoring of pulmonary function is required in patients receiving long-term treatment with furadonin, especially in the elderly.
Careful monitoring of patients receiving long-term therapy with furadonin is necessary to identify signs of hepatitis development.
After taking furadonin, the urine may turn yellow or brown. Patients receiving furadonin may experience false-positive reactions when determining glucose in the urine.
Furadonin should be discontinued if signs of hemolysis appear in patients with suspected glucose-6-phosphate dehydrogenase deficiency.
Reactions from the gastrointestinal tract can be minimized when taking the drug with food, milk or by reducing the dose.
Pregnancy and lactation period. The use of furadonin during pregnancy is contraindicated. If it is necessary to use it during lactation, the child should be weaned from the breast for the entire period of treatment.
Use in pediatrics. Not recommended for use in children under 6 years of age.
Caution when prescribing should be observed in persons with diabetes mellitus, anemia, electrolyte disturbances, deficiency of B vitamins, because the neurotoxic effect of the drug may be enhanced.
Furadonin should not be used to treat diseases of the renal cortex (glomerulonephritis), purulent paranephritis, or prostatitis. Especially for the treatment of parenchymal infection of one non-functioning kidney. In cases of recurrent or severe infection, surgical causes must be excluded.
Influence on the ability to drive vehicles and work with moving mechanisms. Furadonin may cause dizziness and drowsiness. The patient should not drive a car or operate moving machinery while taking the medicine.
Overdose
Symptoms: when high doses are administered, dizziness, nausea, vomiting, and stomach irritation may occur.
Treatment: discontinuation of the drug, gastric lavage, taking large amounts of fluid to increase excretion of the drug in the urine, hemodialysis, symptomatic therapy.
There is no specific antidote.
Release form and packaging
10 tablets in a contoured cell-free package made of a combination of paper and cardboard material.
Contour cellless packages (without insertion into a pack), together with the appropriate number of instructions for medical use in the state and Russian languages, are placed in a cardboard box.
10 tablets per blister pack made of polyvinyl chloride film and flexible packaging based on aluminum foil for medicines.
2 blister packs together with instructions for medical use in the state and Russian languages are placed in a cardboard pack.
Storage conditions
Store in a dry place, protected from light, at a temperature not exceeding 25 ºС.
Keep out of the reach of children!
Shelf life
4 years
Do not use after expiration date.
Conditions for dispensing from pharmacies
On prescription
Manufacturer
Open Joint Stock Company "Borisov Medical Preparations Plant", Republic of Belarus, Minsk region, Borisov, st. Chapaeva, 64,
tel/fax +375 (177) 734043.
Registration Certificate Holder
Open Joint Stock Company "Borisov Medical Preparations Plant", Republic of Belarus
Name, address and contact details (telephone, fax, e-mail) of the organization in the territory of the Republic of Kazakhstan responsible for post-registration monitoring of the safety of the medicinal product
Republic of Kazakhstan, 050004, Almaty, Abylay Khan Avenue, 30, MedPharmInterService LLP, tel. 87013066011, 87714140258.
Side effects
After taking the pills you may experience:
- vomiting, dizziness , nausea, headaches;
- arthralgia , asthenia , myalgia , nystagmus , anaphylactic shock ;
- lupus-like syndrome , chills and skin rashes, eosinophilia ;
- drowsiness , cough, pain in the chest, broncho-obstructive syndrome , fever , interstitial changes in the lung tissue;
- hepatitis , pancreatitis , cholestatic syndrome , pseudomembranous enterocolitis , diarrhea ;
- peripheral neuropathy , abdominal pain.
With long-term treatment with the drug, the likelihood of developing malignant kidney tumors .
Nitrofurantoin, its derivatives and metabolites have a toxic effect on the lungs. One patient out of 5000 after completing a single course of the drug develops: shortness of breath , cough, fever , eosinophilia , myalgia and bronchospasm . Long-term treatment with the drug can lead to lobar infiltration , pleural exudation , vasculitis , alveolar exudation , interstitial inflammation .
In 1 in 20,000 patients, taking this substance causes pulmonary fibrosis and other irreversible toxic damage to lung tissue. If therapy is repeated, the risk of developing this type of damage increases significantly.
Allergic reactions that are observed during treatment with the drug disappear on their own after cessation of therapy.
Side effects of the drug Nitrofurantoin
Eosinophilic infiltrate in the lungs, fever, chills, cough, chest pain, shortness of breath, eosinophilia, nausea, vomiting, anorexia, rarely - hepatitis, cholestatic jaundice, abdominal pain, diarrhea, peripheral neuropathy, nystagmus, dizziness, asthenia, headache , drowsiness, exfoliative dermatitis and erythema multiforme, reversible alopecia, lupus-like syndrome, angioedema, maculopapular rash, erythema, eczema, urticaria, pruritus, anaphylactic reactions, sialadenitis, pancreatitis, gout, myalgia, drug fever, agranulocytosis, leukopenia, granulocytopenia, hemolytic anemia, thrombocytopenia, anemia caused by glucose-6-phosphate dehydrogenase deficiency, megaloblastic anemia and eosinophilia. When the course of treatment is stopped, blood counts return to normal. There are reports of rare cases of aplastic anemia.
Nitrofurantoin, instructions for use (Method and dosage)
Tablets are prescribed orally. The medicine must be taken with plenty of liquid.
Nitrofurantoin, instructions for use
Patients are prescribed from 50 to 150 mg of the drug in 3-4 doses per day. The course of treatment ranges from 5 days to one week.
The maximum single dosage for an adult is 0.3 grams of the drug. You can take up to 0.6 mg of medication per day.
Children are prescribed 5-8 mg of the substance per kg of weight. The daily dosage is divided into 4 doses.
If necessary, treatment can be continued for up to 10 days, provided that the sterility of the urine is monitored.
If there is a need for long-term maintenance treatment with the drug, it is better to use the minimum dosage. When carrying out therapy for 3 months or more, the optimal amount of Nitrofurantoin that the patient can take per day is 1.5 mg per kg of weight.
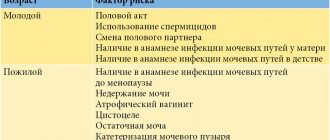
The use of nitrofurans for urinary tract infections
Despite almost 60 years of experience in medical practice, nitrofurans remain one of the most active antibacterial drugs against pathogens of uncomplicated lower urinary tract infection (LUTI): cystitis, urethritis. The high natural activity of nitrofurantoin and furazidin against both E.coli and gram-positive pathogens, in particular Enterococcus faecalis and S.saprophyticus, forces them to remain in the formulary of drugs for the treatment of urinary infections.
Table 1. Structure of pathogens of uncomplicated UTIs in Russia
Table 2. Frequency of isolation of resistant E. coli strains in patients with outpatient UTIs in Russia to oral antibiotics, %
Table 3. Pathogens of uncomplicated and complicated urinary tract infections in outpatients in Moscow
Table 4. Antibiotic susceptibility of E. coli strains isolated from patients with uncomplicated UTIs in Moscow (2)
Table 5. Bacteriological characteristics of 1990 isolates (NAUTICA)
Table 6. E. coli susceptibility data from the ARESC study (2006)
Table 7. Comparison of toxicity and side effects of nitrofurans
Table 8. Antibacterial activity in vitro MIC, µg/ml
Table 9. Pharmacokinetic data of furagin and furamag
Figure 1. Concentration of drugs in urine (single dose of 100 mg of the drug)
Figure 2. Total urinary excretion of drugs (single dose of 100 mg of drug)
Table 10. Characteristics of patients treated with Furamag
Table 11. Microbial spectrum of pathogens
Recently, interest in them has been increasing due to the low level of resistant strains of urinary pathogens, while there has been an increase in the resistance of E. coli
to trimethoprim/sulfamethoxazole (TMP/SMX), ampicillin, amoxicillin, protected beta-lactams, quinolones.
Practicing physicians should be familiar with data on the resistance of pathogens in a particular region and take them into account when making decisions about prescribing empirical therapy for UTI, since pathogen resistance to the drug used increases the risk of treatment failure.
Over the past 9 years, the Research Institute of Antimicrobial Chemotherapy (Smolensk) and the Department of Clinical Pharmacology of the Smolensk State Medical Academy, in collaboration with leading urological clinics of the Russian Federation, have been conducting a series of studies using uniform UTIAP codes, which are aimed at studying the spectrum of pathogens and monitoring the antibiotic resistance of the main uropathogens.
A total of three studies were conducted: UTIAP-1 (1998), UTIAP-2 (2002) and UTIAP-3 (2005). (1) (Table 1 and 2).
Antibiotics and antimicrobial drugs, the level of resistance to which exceeds 20% - ampicillin and co-trimoxazole according to the criteria adopted by international communities (IDSA, EAU, AUA), cannot be considered as means of empirical choice for the treatment of outpatient UTIs. Antibiotics with high microbiological activity against the main pathogens of outpatient uncomplicated UTIs (primarily E. coli
), – fluoroquinolones (ciprofloxacin, norfloxacin), cephalosporins II-III (cefuroxime, ceftibuten), nitrofurantoin.
Not all of the listed antimicrobial drugs, despite their high microbiological activity, have the same clinical significance for the treatment of uncomplicated UTIs. In addition to the level of resistance in the region, it is necessary to take into account such characteristics as safety and tolerability, pharmacokinetic profile, and the effectiveness of the drug proven in clinical trials.
II-III generation cephalosporins (cefuroxime and ceftibuten) have
high activity against E. coli At the same time, b-lactams are generally less effective in the treatment of UTIs compared to fluoroquinolones, since their administration achieves lower concentrations in urine. This is why b-lactam antibiotics cannot be used to treat UTIs in short courses (3-5 days). The third group includes drugs with an intermediate level of resistance - primitive quinolones and amoxicillin/clavulanate. The resistance of uropathogenic E. coli
to early (“primitive”) quinolones, nalidixic and pipemidic acids in Russia is relatively low (8.9%), but is 2 times higher than the level of resistance to fluorinated quinolones – norfloxacin, ciprofloxacin, levofloxacin. Early quinolones must be taken at least 4 times a day to create sufficient concentrations in the urine, which sharply reduces patient compliance with these uroseptics. Comparative clinical trials conducted in patients with uncomplicated UTIs revealed a significantly higher microbiological effect and better tolerability of fluoroquinolones (norfloxacin) compared with earlier quinolones (nalidixic acid). Considering the threat of increasing antibiotic resistance in general and to UTI pathogens in particular, it is necessary to take into account the property of early quinolones to induce the development of resistance not only to the early quinolones themselves, but also to fluoroquinolones (1).
According to studies of antibiotic resistance in pathogens of urinary infections in outpatients in Moscow (UTIAP studies from 1998 to 2005), the main causative agents of outpatient UTIs are representatives of the family Enterobacteriaceae
, which were isolated in 86% of cases.
The most common uropathogen is E. coli
, which was found in 90% of patients.
Other pathogens were much less common. In 16% of cases, other representatives of the family Enterobacteriaceae were isolated: Klebsiella spp., P.mirabilis
and
Enterobacter spp.
, while gram-positive microorganisms –
Staphylococcus spp., Enterocccus spp.
and
S.agalactiae
– in 10.% of cases.
Table 3 presents the causative agents of uncomplicated (NIUT) and complicated (CIUT) urinary tract infections in outpatients at different time intervals in Moscow (2).
In complicated lower urinary tract infections, E. coli
(53% and 80.9%) and the proportion of such pathogens as
P.aeruginosa
(4.5% and 0%) and
E.faecalis
(9.1% and 4.2%) is significantly increasing.
In the UTIAP studies, the proportion of uncomplicated UTIs was 37.6% and the proportion of complicated UTIs was 38.8%. (2)
One of the most common complicating factors is urolithiasis and, as a consequence, the presence of stones in the kidneys or urinary tract - 48.5%. Other common complicating factors were: diabetes mellitus - 24.2%, conditions after operations were much less common - 3.%, bladder outlet obstruction - 6.1%, etc.
E.coli resistance data
, as the most common causative agent of urinary infection, are of the greatest interest and are the basis for further use in practical guidelines on recommendations for the selection of drugs for empirical treatment of uncomplicated urinary tract infection.
Data on the sensitivity study of the main causative agent of NIMP Escherichia coli are presented in Table 4.
The data obtained demonstrate different levels of E.coli
to beta-lactam antibiotics.
Noteworthy is the high frequency of isolation of E. coli
to ampicillin (28.6-43.75%)1.
E. coli
is highly resistant to ampicillin has not changed over time; moreover, there is an increasing trend. The high level of strains resistant to co-trimoxazole does not allow it to be recommended for empirical treatment of NSTI in Moscow, and data on E. coli resistance to nitroxaline (93.4% of resistant strains) even made it possible to exclude it from UTIAP studies in 2004-2005.
Sidorenko S.V. et al. (3) in a study of 375 strains that cause urinary infections in Moscow, also confirms the priority of Escherichia coli among all pathogens of urinary tract infections. Further, significantly lagging behind in importance, follow Klebsiella spp, Proteus spp, Enterobacter
, from gram-positive -
Enterococcus faecalis
. E. coli strains were highly sensitive to nitrofurans - 88%, in particular to nitrofurantoin. Efficacy criteria for furazidine and furazidine potassium salt have not currently been developed. However, the geometric mean MIC values of these compounds are significantly lower than those of nitrofurantoin, which indicates their greater antibacterial activity.
The data obtained during the study do not differ significantly from data from other studies on the resistance of urinary pathogens. Among gram-negative pathogens, the number of strains sensitive to co-trimoxazole was noted in 47-75%.
At the same time, the growth of quinolone-resistant strains is noteworthy. Thus, sensitivity to nalidixic acid among enterobacteriaceae was noted in 70.8-79%, and to ciprofloxacin - in 82.3-85.7%, respectively (3). This, of course, is due to the fact that the study involved not only patients with uncomplicated but also complicated urinary tract infections, and men with bacterial prostatitis.
Of interest are the data from the North American Urinary Tract Infection Collaborative Alliance-NAUTICA to determine the sensitivity of outpatient UTI pathogens (uncomplicated and complicated) to commonly used antibacterial drugs, isolated in different regions of the USA and Canada. The study was conducted at 41 medical centers (30 in the United States and 11 in Canada). During the period from April 2003 to June 2004 inclusive, each Center submitted up to 50 pathogens. Of interest is the study of the influence of age and gender on the resistance of pathogens. In the case of ampicillin, resistance was higher in people under the age of 14 years inclusive, and resistance to TMP/SMX was lowest in women aged 15 to 50 years, while no statistically significant differences were found in both cases. Resistance to fluoroquinolones (ciprofloxacin and levofloxacin) increased with age and was higher in men than women, being highest in men aged 65 years and older (p
The most highly resistant E. coli
(n=1142) was to ampicillin (37.7%), followed by TMP/SMX (21.3%), ciprofloxacin (5.5%), levofloxacin (5.1%) and nitrofurantoin (1.1% ). Resistance to all antibiotics was higher in the United States compared to Canada. So for ampicillin these figures were 39.3% and 33%, TMP/SMX - 22.6% and 17.7%, ciprofloxacin - 6.8% and 1.1%, levofloxacin - 6.4% and 0.7 % and nitrofurantoin – 1.4% and 0%, respectively (p
The results of the present study show that the frequency of resistance to ampicillin among all isolates was 45.9%, and to TMP/SMX - 20.4%. These data are consistent with previous studies showing that resistance to ampicillin and TMP/SMX continues to increase in North America. Overall resistance to nitrofurantoin occurred in 14.3% of isolates. This figure is quite high and probably reflects the fact that only 57.5% of the isolates were E. coli
and a significant part of the isolated microorganisms were enterobacteria such as
Klebsiella spp.
and
Proteus spp.
, relatively resistant to the action of nitrofurantoin.
Obviously, urine collection was carried out not only in women with uncomplicated cystitis and urethritis, but also in postmenopausal women, and in patients of both sexes with asymptomatic bacteriuria (complicated UTI). At the same time, these data have great practical value, since they reflect real clinical practice. Among E. coli,
the incidence of resistance to nitrofurantoin was 1.1%. Data on resistance to ciprofloxacin (9.7%) and levofloxacin (8.1%) are consistent with those obtained previously. These results indicate that such drugs should be prescribed judiciously to prevent the rise of drug resistance (4).
The latest international epidemiological study of antibiotic resistance in uncomplicated urinary tract infections (ARESC) was completed in 2006. 10 countries took part in the study, including Russia. Cystitis pathogens from 61 medical centers were studied, 10 centers from Russia. Among the causative agents of uncomplicated urinary tract infection are E.coli
isolated in 76.3%,
S.saprophyticus
– 3.6%,
Klebsiella pneumonia
– 3.5%,
Proteus mirabilis
– 3.1%,
Enterococcus faecalis
– 3%, other species of the
Enterobacteriaceae
account for 6.4%, other representatives of gram-positive flora – 3.7% (Table 6).
Thus, it is clear that the percentage of E. coli strains resistant to nitrofurantoin in all studies is less than 5%. Sensitivity of gram-positive flora, in particular Enterococcus faecalis
and
S.saprophyticus
, the etiological significance of which has recently been increasing, is approaching 100%. This circumstance could not go unnoticed, which fueled our interest in nitrofuran drugs in general, and in furamag in particular.
History of
nitrofurans
The history of clinical use of nitrofurans or 5-nitrofuran derivatives begins from 1943-1947. after the discovery by M.
Dodd
and
W. Stilman
(5).
Nitrofuran preparations are classical synthetic chemotherapeutic agents with a broad antimicrobial spectrum of action. It is extremely important that nitrofuran drugs are not general enzymatic poisons, but exhibit a strictly selective effect on certain enzymatic systems. Such a long presence of nitrofuran drugs in the first-line list for the treatment of urinary infections is due to the fact that they have a unique antimicrobial mechanism of action on pathogenic microflora - an effect on cellular respiration (6).
Today, the most popular nitrofurans used in urology for chemotherapy of infectious diseases are:
- Nitrofurantoin (Furadonin) was first synthesized in the USA in 1952.
- Furazidin (Furagin) is an original drug created at the Institute of Organic Synthesis of the Academy of Sciences of Latvia in 1954.
- Furamaga capsules 50 mg - an original medicinal composition of furagin soluble with magnesium carbonate as the main one was developed by O.N. Akifev, G.M. Grinberg, M.Ya. Paberzoy, A.P. Gilev and the chief urologist of the USSR A.Ya. Pytel in 1986-87. Antimicrobial activity of nitrofurans
The antimicrobial spectrum of action of nitrofurans includes microorganisms that cause both urological and intestinal infections. These include gram-negative microorganisms: E.coli, Shigella spp, Salmonella spp, Proteus spp, Klebsiella spp, Aerobacter aerogenes
and gram-positive aerobic bacteria:
Staphylococcus spp, S.pyogenes, E.faecalis, Corynebacterium spp,
pathogenic fungi -
candida albicans, Microsporum spp
, some protozoa:
Trichomonas vaginalis, Lamblia intestinalis, Entamaeba hystolytica.
(7).
Speaking about the general characteristics of nitrofuran drugs in terms of the degree of activity “in vitro” in terms of MIC and bactericidal concentrations, it should be noted that they, of course, are inferior to fluoroquinolones and broad-spectrum antibiotics. There is a difference in the degree of activity of individual nitrofurans.
The mechanism of action of nitrofurans consists of several factors (6, 7, 8).
Acting as hydrogen acceptors, they enter into competitive relationships with natural hydrogen acceptors in the chain of oxidative processes. Nitrofurans, being restored in the culture medium, distract electrons (hydrogen) from their normal metabolic pathway, thereby inhibiting cellular respiration and preventing the formation of energy necessary for the growth and reproduction of microbial cells. The drugs undergo intracellular transformation, the process of restoration of the nitro group occurs under the influence of bacterial flavoproteins. As a result, metabolites of nitrofurans are formed, which have a cytotoxic effect. The drugs inhibit the biosynthesis of microbial DNA and, to a lesser extent, RNA. The mechanism of action of nitrofurans has not been fully studied, but it is specific only for drugs of this group. This is why nitrofurans are active against most bacteria that are resistant to antimicrobials of other classes of chemicals (7). Biological fluids (blood, serum, urine, cerebrospinal fluid), as well as novocaine, do not reduce the antibacterial activity of nitrofurans. Antagonists of nitrofurans are B vitamins and quinolones.
Resistance to nitrofurans is cross-linked only within this class of substances. Bacterial strains resistant to beta-lactams, aminoglycosides, zloramphenicol, fluoroquinolones, tetracyclines, and sulfonamides remain sensitive to nitrofurans. It is necessary to study the biochemical mechanisms of resistance in the development of drug resistance of bacteria to nitrofurans. However, the problem of drug resistance to nitrofurans is not of clinical significance, since despite the long-term use in medical (since the 1950s) and veterinary practice (since 1994) and the current isolation of pathogen strains sensitive to nitrofurans, further successful use can be predicted some drugs in this group.
Tolerability ,
adverse reactions , contraindications for use
Nitrofurans have a narrow therapeutic range and are used in low therapeutic doses. Recommended doses must be strictly followed. Exceeding dosages is associated with a significant risk of adverse reactions. Nitrofurantoin is more toxic than furazidin (Furagin) and Furamag (Table 7). Nitrofurans cause the same unwanted side effects as other drugs. From the gastrointestinal tract there may be pain and nausea, discomfort, rarely - loss of appetite, and even less often - diarrhea and vomiting. On the part of the liver, a transient increase in transaminases is possible. Allergic reactions to nitrofurans can manifest themselves in the form of skin rash and itching, arthralgia and myalgia, eosinophilia, and fever. Rare adverse reactions specific to nitrofurans and requiring special attention from a physician include:
- reactions from the respiratory system (acute pneumonitis - pain in the chest, cough, difficulty breathing, increased body temperature) are more common in elderly patients and are usually reversible after cessation of treatment (7). In urological practice, pneumonitis has been described only in elderly patients, most often men in nursing homes, who received nitrofurantoin for a long time - 12 months (9);
- reactions from the nervous system in the form of dizziness, drowsiness and fatigue, headache, polyneuropathy, muscle weakness;
- hematological reactions: granulocytopenia, leukopenia, anemia, decreased platelet aggregation, very rarely - hemolytic anemia (7).
The risk of undesirable side reactions increases with renal and liver failure, when combined with drugs that depress hematopoiesis in patients with glucose-6-phosphate dehydrogenase deficiency. Nitrofurans should not be prescribed to children in the first month of life due to the high risk of developing hemolytic anemia due to insufficient age-related development of enzyme systems.
Nitrofurantoin
The activity of nitrofurantoin is enzyme-dependent and unique among antimicrobials due to its multiple mechanisms of action. The drug interferes with bacterial enzyme systems, including DNA and RNA synthesis, carbohydrate metabolism and other metabolic enzyme proteins (10).
Nitrofurantoin is a weak acid and is excreted in the kidneys by glomerular filtration and tubular secretion, reaching high concentrations in urine that depend in part on urine pH. Because it is a weak acid, the presence of acidic urine increases the amount of drug reabsorbed from the renal tubules; conversely, when urine is alkaline, drug reabsorption is reduced and large amounts of drug are then excreted, resulting in large concentrations in urine (10). After taking soda, due to the formation of a water-soluble sodium salt, the excretion of the drug in the urine increases. It is quickly metabolized in body tissues. As a result, low concentrations of the drug remain in the blood serum relative to urine, and urine may turn brown. Therapeutic concentrations are achieved only in urine. Taking the drug with food increases bioactivity by 40% and increases the duration of therapeutic concentration in urine. Communication with blood proteins is average – 60%. Biotransformation: 2/3 of the drug is quickly metabolized and inactivated in most body tissues, including the liver. The half-life in patients with normal renal function is 20 minutes to 1 hour and approximately half of the drug is excreted in the active unchanged form. Patients with renal impairment (creatinine clearance less than 50 mL/min) should avoid nitrofurantoin to prevent crystalluria and possible adverse drug accumulation reactions. During hemodialysis, the drug is eliminated (11).
There are two different forms of nitrofurantoin: macrocrystalline dosing 4 times daily and a modified monohydrate macrocrystalline form that allows dosing 2 times daily (12). The macrocrystalline form provides delayed release and a slight reduction in bioactivity from the gastrointestinal tract, while the modified monohydrate form delays gastric absorption due to its unique gel matrix and allows for a longer dosing interval (10).
Furazidin
Furagin is a weak acid and, due to the presence of active hydrogen in the molecule, is capable of forming salts (6). Replacing a hydrogen atom with a potassium atom results in the production of the potassium salt of furagin - solafur. However, in the presence of carbon dioxide and water vapor, or in the presence of hydrochloric acid in the stomach, a reverse reaction occurs, as a result of which furagin is formed from solafur.
An experiment on mice showed that intense absorption of the drug occurs in the distal small intestine; furagin is transported by passive diffusion (13).
Studies on drug excretion (50 mg tablets) showed that when taking the drug before meals, the maximum concentration of furagin was reached after 6 hours and amounted to 20.06 + 5.33 mcg/ml. Similar indicators when taking the drug after meals were 2 hours and 22.6 + 2.27 mcg/ml, respectively. Moreover, when taking the drug on an empty stomach in the first 4 hours after using the drug, its concentration in the urine was on average 2 times lower than when taking furagin tablets after meals (14).
Furamag
It was found that the combined release of solafur with magnesium carbonate makes it possible to reduce the pyrophoricity of solafur and significantly increase the bioavailability of the drug when administered orally. At the Institute of Organic Synthesis of the Academy of Sciences of Latvia, based on the potassium salt of furagin in combination with basic magnesium carbonate in a 1:1 ratio, it was possible to develop an optimized dosage form of furazidin for oral use under the trade name “Furamag”. Basic magnesium carbonate prevents the conversion of the potassium salt of furazidin in the acidic environment of the stomach into furagin and ensures more complete absorption of the drug in the small intestine in the form of a highly soluble potassium salt. The bioavailability of furazidin contained in furamage is 2.5-3 times higher than the bioavailability of furagin. The higher degree of bioavailability of furazidin in the form of furamag allows one to obtain a therapeutic effect in lower doses. When Furamag is administered orally, the potassium salt of furazidine is rapidly absorbed and excreted by the kidneys through tubular secretion and glomerular filtration. In urine, high concentrations of the potassium salt of furazidin are achieved, exceeding bacteriostatic levels by more than 50 times (Table 8).
The maximum concentration in the urine of the potassium salt of furazidine is determined 3-4 hours after oral administration. When using Furamag, higher concentrations of the drug are achieved in the blood than other nitrofurans. This is the basis for more detailed studies of the possible systemic effects of the drug (7). When studying the pharmacokinetics of Furamag and Furagin, the bioavailability of Furamag is on average 2.5 times higher (15) (Table 9).
Data from comparative studies of Furagin 50 mg tablets and Furamag 50 mg capsules, performed on 19 volunteers, are shown in Figures 1 and 2. As can be seen from the presented results, Furamag creates a concentration of the drug in urine almost 6 times higher than that for Furagin tablets. Moreover, the bioavailability of Furamag is approximately 2.5-3 times higher than that of Furagin 50 mg tablets at the same administration doses (16).
Clinical
use
Clinical use of furamag for urological diseases has shown their high clinical and bacteriological effectiveness. Back in 1982, in the treatment of cystitis, pyelitis, urethritis, prostatitis, epididymitis in 63 patients, a dose of 50 mg 3 times a day for 7-10 days showed good efficacy and tolerability of the drugs (17). In a study of 355 strains of urinary infection pathogens, sensitive strains of E. coli, Staphylococcus spp., E.
Faecalis
.
Proteus spp., K. Pneumonia, P.aeruginosa
were resistant at the Kharkov Medical Academy of Postgraduate Education when studying the clinical effectiveness of Furamag for UTI in women and men (96 patients) in monotherapy 50 mg 3 times a day for 7 -10 days. The drug was highly effective in the treatment of urethritis in men, and in women - chronic cystitis or endocervicitis. The drug was weakly effective in the treatment of chronic epididymitis, which is understandable, because tissue concentrations of nitrofurans are extremely low. Of the adverse reactions, the authors noted discomfort and nausea in 4.87% of patients who did not require discontinuation of the drug (19).
According to a multicenter, prospective, open-label, controlled comparative study of the clinical and bacteriological effectiveness of the drug Furamag in the treatment of 105 patients with acute uncomplicated cystitis in Moscow (20), recovery was achieved in 92.6% and 96%, 5 and 7-day courses of treatment, respectively. Side effects in the form of nausea were recorded in 4.8% of cases. Only 2 patients stopped treatment due to adverse reactions.
Bacteriological effectiveness ( E. coli, Staphylococcus saprophyticus, Enterococcus faecalis
) was noted in 94% and 97%, respectively.
In 2007, the Research Institute of Urology of Rosmedtechnologies conducted an open clinical post-marketing study of the drug Furamag for the treatment of infectious and inflammatory urological diseases. The study included adult patients, of both sexes, with bacteriologically proven nonspecific urinary tract infection (UTI) and sensitivity to furazidine. Based on these criteria, 40 patients were included in the study. The drug was prescribed orally, after meals, with plenty of liquid, 50–100 mg 3 times a day. The course of treatment is 5-7-10 days; if necessary, the course was repeated. The different dosage regimens are due to the fact that we selected patients strictly according to the sensitivity of microorganisms to furagin, not only with acute cystitis, but also with persistent, recurrent urinary tract infection.
The age of the patients was from 18 to 79 years, the average age was 37.58 years, of which: 5 men and 35 women. The average duration of the disease before treatment was 1.12 years.
The distribution of patients by diagnosis is presented in Table 10.
In all patients included in the study, the growth of microorganisms sensitive to furazidine was determined in urine cultures before treatment (Table 11).
After treatment, 35 patients achieved complete eradication of pathogens, i.e. an excellent result. In four patients, a decrease in the microbial number of microorganisms was noted, in particular: in a patient with chronic bacterial prostatitis and with a mixed urinary infection: E. coli + Enterococcus faecalis
106 before treatment, after a 10-day course of treatment with Furamag, a decrease in the microbial titer of enterococcus to 104 and eradication of Escherichia coli was noted, which, of course, can be regarded as a positive result of treatment.
In women with persistent infection, recurrent cystitis, after 5 days of treatment, clinical improvement was noted and a decrease in the microbial number of Enterococcus faecalis by 2 Lg
from 104 to 102. Eradication of one of the pathogens in a patient with a mixed infection and a decrease in the microbial titer in the second pathogen (
E.coli + Enterococcus faecalis
from 108 to
E.coli
at 102;
E.coli+ Staph.spp.
104 to
Staph.spp.
102 after treatment). The results of treatment of these 4 patients were assessed as good, because a microbial titer of 102 CFU/ml is a clinically insignificant titer.
In only one patient, the treatment results were assessed as unsatisfactory: in a woman with a chronic urinary tract infection due to urolithiasis (microlith in the right kidney) and cystitis, a change in pathogen occurred during 5 days of treatment with Furamag: Staphylococcus epidermidis
10 in 4 degrees, after treatment –
Streptococcus adalactae
10 in 4 degrees, although
Streptococcus adalactae
is a normal vaginal microflora (control urine cultures were carried out after 2-3 weeks of the so-called “cleansing period”, i.e. patients did not take any anti-inflammatory therapy).
Good and excellent bacteriological effectiveness of Furamag in the treatment of UTIs was demonstrated in 39 patients, which amounted to 97.5%; in 1 patient (2.5%) there was no bacteriological effect. Good clinical efficacy was observed in 35 patients (87%).
Only one patient noted dizziness while taking Furamag; after treatment, the dizziness stopped. The remaining patients did not report any undesirable side effects during therapy with Furamag. No allergic reactions associated with taking the drug were observed in patients. Thus, drug tolerability was excellent in 39 patients (97.5%).
Such good treatment results are explained by careful selection of patients for treatment with Furamag. As can be seen from the tables, we mainly selected patients with colibacillary and enterococcal infections, who are most sensitive to Furamag. Considering the growth and significance of enterococcal urinary tract infections in recent years, as well as the increasing resistance of urinary pathogens to many antibiotics, there has been a renaissance of nitrofurans, the effectiveness and safety of which have been tested by time.
Nitrofurans will be in the arsenal of doctors for a long time for the treatment of uncomplicated and complicated urinary tract infections, in the treatment of asymptomatic bacteriuria in pregnant women, as well as as a prophylaxis for recurrent urinary infections and sanitation of the urinary tract before urological operations, remote stone crushing, endoscopic operations and other urological operations .
Interaction
The combination of taking drugs that block tubular secretion ( sulfinpyrazone, probenecid ) and Nitrofurantoin leads to a decrease in the effectiveness and concentration of the latter in the urine, and an increase in its toxicity.
The effectiveness of the drug is reduced by nalidixic acid and magnesium trisilicate antacids .
The medicine cannot be combined with fluoroquinolone and its derivatives.
special instructions
In patients with anemia , electrolyte B vitamin deficiency, peripheral neuropathy increases .
The substance is ineffective in the treatment of diseases of the renal cortex, prostatitis , and purulent paranephritis .
Nitrofurantoin should not be combined with drugs that have an inactive effect on kidney function.
Reviews of Nitrofurantoin
- “... The doctor prescribed tablets for cystitis. During treatment with the drug I felt very bad. He, of course, helped me, after the first pill I felt improvements, but I can no longer endure the constant headache, stomach pain and nausea. Next time, if I get sick, I will never take this medicine”;
- “...I have chronic pyelonephritis. Sometimes I take these tablets in combination with others during exacerbations. The medicine helps quickly and for sure. However, the pills are so bitter, they constantly make me sick. On the plus side, they are quite inexpensive”;
- “... I take this antimicrobial agent if I get cystitis. I tried everything. In the end I settled on these pills. I didn’t notice any side symptoms.”