Intestinal obstruction - symptoms and treatment
Correct diagnosis and physician tactics play a big role in the treatment of intestinal obstruction. Treatment involves:
- timeliness of infusion therapy;
- identifying the cause of the pathological process;
- choosing a compression relief method;
- determining the scope of surgical intervention;
- prevention of postoperative complications and patient rehabilitation.
Objectives and content of surgical intervention
Intestinal decompression (surgical removal of its compression) is divided into closed and open methods.
The closed method consists of inserting an 80-100 cm nasogastric tube with many side holes with a diameter of 0.3-0.4 cm - intestinal intubation. The duration of intestinal drainage is 2-5 days.
Open decompression methods include enterotomy, jejunostomy, and colonostomy.
Less effective methods of decompression are:
- intestinal intubation (70-80 cm below the Treitz ligament) through a microgastrostomy;
- end ileostomy - should be performed at a distance of 25-30 cm from the cecum;
- hanging enterostomy;
- cecostoma;
- transcecal retrograde intubation of the small intestine;
- contranatural anus.
If there is colonic obstruction of the left intestine, then Hartmann's operation . If the site of occlusion is located in the rectum, then the tactics change: extirpation of the rectum is performed and, if the intestine is long enough, a coloanal anastomosis is performed.
To correct fecal incontinence, anal ring plastic surgery is performed using the adductor magnus muscle of the thigh or a magnetic sphincter.
Performing surgical intervention in patients with acute insufficiency at a late stage and in conditions of developed peritonitis has its own characteristics. They are associated, first of all, with the need for thorough sanitation of the abdominal cavity during surgery.[16]
Treatment and observation of patients in the postoperative period is of great importance.[3][5] For this purpose the following is carried out:
- correction of hypohydration - introduction of polyionic solutions;
- restoration of water-electrolyte and colloid-osmotic functions;
- restoration of acid-base relationships.
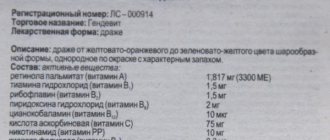
An important aspect in the treatment of acute infusion is infusion therapy . A patient with OKN is prescribed crystalloids, protein, glycosylated and colloidal drugs. Antibiotic therapy should also be carried out .
In the treatment of acute insufficiency, broad-spectrum antibiotics are used - third generation cephalosporins, fluoroquinolones, carbapinems and metronidazole. The duration of antibacterial treatment is 7-9 days.
All postoperative treatment tactics should be aimed at eliminating intoxication, restoring water-electrolyte balance and maintaining gastrointestinal motility. Patients are prescribed:
- sodium bicarbonate solution;
- 5% glucose solution;
- Ringer's solution.
In the absence of contraction of the intestinal walls, proserine derivatives or neuromidin are added. As an analgesic measure, a paraumbilical blockade is performed (if the initial cause was pancreatic pathology).[15]
In the postoperative period, a mandatory measure is to rinse the intestines with antiseptic solutions through a probe, which remains until intestinal motility is restored, gases begin to escape and the amount of discharge through the intestinal tube decreases.
Is it possible to cure intestinal obstruction without surgery?
Therapeutic methods for treating intestinal obstruction are usually ineffective and are not used, since lost time can lead to complications and death.
If a patient sees a doctor with intestinal obstruction that is just developing, and its cause is constipation or decreased intestinal tone, then cleansing siphon enemas (a solution of magnesium sulfate and magnesium sulfate) and laxatives are used. These methods are effective in treating constipation and developing intestinal obstruction.
It is important to understand that only a doctor can judge whether intestinal obstruction has formed after diagnosis. It is impossible to treat yourself, since the patient can suffer serious complications if intestinal obstruction has already formed and caused a persistent block of the intestinal lumen.
Physical exercise
In case of intestinal obstruction, physical exercise is strictly prohibited . The basic rule: “cold, hunger and peace” and contact a specialist.
Can I use a laxative?
Laxatives can be used only in case of developing intestinal obstruction and under the supervision of a doctor, since it is impossible to independently determine the stage of the disease.
Can I use an enema?
Enemas are effective if you consult a doctor before intestinal obstruction has formed, and this is confirmed by diagnostic methods. When the disease has developed, the use of enemas is dangerous and can lead to serious complications.
Classification
Intestinal obstruction is not an independent disease, but is a symptom as a result of which the passage of contents through the intestines is stopped and disrupted. According to the International Classification of Diseases, 10th revision (ICD-10), this condition is a complication of other diseases, which include the following nosologies: [7]
| Code | Nosology |
| K56 | Paralytic ileus and intestinal obstruction without hernia |
| K56.0 | Paralytic ileus |
| K56.1 | Intussusception |
| K56.2 | Volvulus |
| K56.3 | Ileus caused by gallstone |
| K56.4 | Another type of closure of the intestinal lumen |
| K56.5 | Intestinal adhesions [adhesions] with obstruction |
| K56.6 | Other and unspecified intestinal obstruction |
| K56.7 | Ileus unspecified |
In addition, intestinal obstruction can be classified according to the degree of passage disturbance, the level of obstruction, the clinical course, etiology and degree of compensation.
According to the degree of passage violation
- Full. The passage of intestinal contents is completely stopped.
- Partial. The passage of intestinal contents is partially preserved.
By level of obstruction
- High (if an obstruction occurs in the right parts of the colon).
- Low (obstruction occurs in the left colon or rectum).
According to the clinical course
- Spicy.
- Chronic.
According to the etiology of occurrence
- Tumor. The tumor can compress the intestines from the outside, in which case they speak of functional obstruction. If the tumor is inside the intestine, it is mechanical. When the tumor invades the nerve plexus, pseudo-obstruction may occur.
- Non-tumor. The cause may be a decrease in intestinal tone, constipation, fecal blockages, diverticulitis, infarction of the intestinal wall, hernias, adhesions, etc.
By degree of compensation
- Compensated. It occurs against the background of regular constipation with difficulty passing gas and stool retention.
- Subcompensated. The retention of gases and stool does not exceed 3 days.
- Decompensated. Retention of stool and gases exceeds 3 days, there are radiological signs of both small and large intestinal obstruction. [1,3,4]
Is stoma removal always necessary during surgery for intestinal obstruction?
In addition to creating a stoma, an alternative way to restore the passage of food through the intestines is to create an intestinal bypass anastomosis. Operations are named after the parts of the intestine connected, for example:
- An operation on the right side of the large intestine is called a bypass ileotransverse anastomosis.
- The imposition of an anastomosis between the initial part of the small intestine and the final part of the jejunum is called a bypass ileojejunostomy.
Each of these interventions can be temporary, performed to prepare the patient for subsequent stages, or final if radical surgery is not possible.
The main task solved during surgical treatment of acute intestinal obstruction is to save the patient’s life from the threat of breakthrough of intestinal contents into the peritoneal cavity with the development of acute peritonitis and death of the patient.[3,6]
Why is intestinal obstruction dangerous?
Intestinal obstruction leads to dehydration of the body, pronounced shifts in the water-electrolyte and acid-base balance of the body. It is based on a violation of food intake, its digestion and absorption, as well as the cessation of secretion of gastric and intestinal juices into the lumen of the gastrointestinal tract.
Since the tissues and cells of the body are sensitive to the slightest changes in the chemical constancy of the internal environment, such changes cause dysfunction of almost all organs and systems. Along with fluid and electrolytes, in case of intestinal failure, due to fasting, vomiting, and the formation of inflammatory exudate, a significant amount of proteins is lost (up to 300 g/day), especially albumin, which plays an important role in homeostasis. The presence of metastases in the liver, which inhibit the protein-synthetic function of the liver, further reduces the level of protein in the blood, reduces the oncotic pressure of the blood plasma, which causes the development of persistent edema.
The general intoxication of the body with the gradual development of intestinal obstruction is further worsened by the fact that in the contents of the afferent intestine, processes of decomposition and rotting begin, pathogenic microflora begins to multiply in the contents of the intestinal lumen, and toxic products accumulate. At the same time, physiological barriers that normally prevent the absorption of toxins from the intestines do not work and a significant part of toxic products enters the bloodstream, aggravating the general intoxication of the body. Necrosis (necrosis) begins to develop in the intestinal wall, the result of which is purulent peritonitis due to the spillage of intestinal contents into the peritoneal cavity. In this case, toxic products of tissue breakdown, microbial toxins, and severe metabolic changes can lead to sepsis and multiple organ failure and death of the patient. [5.11]
Signs of intestinal obstruction
An early and obligatory symptom of acute intestinal obstruction is abdominal pain. The pain can occur suddenly without any warning signs, be “cramping”, and usually it does not depend on food intake. At first, attacks of pain during acute intestinal obstruction are repeated at approximately equal intervals and are associated with the physiological wave-like movement of the intestine - peristalsis. After some time, abdominal pain may become constant.
With strangulation obstruction, the pain is immediately constant, with periods of intensification during a wave of peristalsis. In this case, the subsidence of pain should be regarded as an alarm signal, since it indicates the cessation of intestinal peristaltic activity and the occurrence of intestinal paresis (paralysis).
With paralytic intestinal obstruction, abdominal pain is often dull, bursting.
Symptoms vary depending on the height of the food obstruction - in the esophagus, stomach, duodenum or large intestine. Retention of stool, including its absence for several hours, and lack of passage of gases are early symptoms of low intestinal obstruction.
When mechanical compression, paresis or narrowing is located in the area of the upper intestines, mainly at the onset of the disease, with partial patency of the intestinal tube, under the influence of therapeutic measures, the patient may have a bowel movement due to bowel movement located below the obstacle. Nausea and vomiting are often observed sometimes repeated, indomitable, increasing with increasing intoxication.
Sometimes there is bloody discharge from the anus.
Upon careful examination, you can notice significant bloating and pronounced asymmetry of the abdomen, peristalsis of the intestines visible to the eye, which then gradually fades away - “noise at the beginning, silence at the end.”
General intoxication, weakness, loss of appetite, apathy - these symptoms are observed in most patients with gradual progression of intestinal obstruction from partial to complete. [1,2]
What needs to be done to save a person with intestinal obstruction?
The development of intestinal obstruction is an indication for urgent hospitalization in a surgical hospital, where the following is immediately performed:
- abdominal radiography,
- ultrasound examination of the abdominal organs
- irrigography is an x-ray examination with a contrast barium suspension introduced into the intestines using an enema.
In our clinic, we often use liquid contrast to better contour the bowel and to prevent barium from entering the peritoneal cavity during subsequent surgery. If the diagnosis is confirmed and/or severe clinical symptoms of peritonitis are present, emergency surgery is performed after very short preoperative preparation.
In the absence of symptoms of peritoneal irritation (peritonitis), conservative therapy is carried out for some time (up to a day) under the supervision of a surgeon:
- rehydration,
- administration of protein solutions, electrolytes,
- administration of antibiotics,
- release of the upper parts of the digestive tract by tube gastric lavage,
- intestinal lavage,
- pain relief, etc.
If there is no effect from conservative treatment, it is necessary to perform surgery as planned. If it is possible to remove the cause of obstruction, a diagnostic laparotomy with intestinal resection is performed. During the operation, an inspection of the abdominal cavity is required to clarify the cause of the development of acute intestinal obstruction and determine the total scope of the operation. [2]
If adhesions, volvulus, loop nodes, or invaginations are detected during an audit of the abdominal organs, they are eliminated. If possible, cytoreductive surgery is performed to remove the primary tumor focus that caused the development of acute intestinal obstruction.
According to existing rules, removal of the intestine in case of obstruction should be carried out at a certain distance above and below the site of obstruction (obstruction). If the diameter of the connected segments is not significantly different, an “end to end” anastomosis is performed; if there is a significant difference in the diameters of the adducting and efferent sections of the anastomosis, a “side to side” anastomosis is performed. In our clinic, we use both classic hand-suturing techniques for the formation of anostoses, and modern stitching devices such as staplers.
In case of severe general condition of the patient or the impossibility of forming a primary anastomosis for other reasons, for example, due to an advanced tumor process, the formation of a “tumor shell”, a large extent of the section of resected intestine, accumulation of a large volume of fluid in the abdominal cavity (ascites), on the anterior abdominal A hole is formed in the wall - a colostomy, into which the adducting and efferent segments of the intestine are brought out - a “double-barrel stoma”.
Depending on the section of the intestine from which the colostomy is formed, this surgical intervention has a different name:
- ileostomy - when removing the small intestine,
- cecostoma - blind,
- ascendo-, descendo- and transversostomy - respectively, ascending, transverse and descending sections of the transverse colon,
- with sigmostomy - from the sigmoid colon.
During surgery on the sigmoid colon, called the “Hartmann operation,” the efferent segment of the colon is always sutured tightly and immersed in the abdominal cavity. [2.12]
Why does acute intestinal obstruction develop?
Among the factors predisposing to mechanical intestinal obstruction, the most common are:
- Adhesive process in the abdominal cavity (as a consequence of the interaction between the tumor and surrounding tissues, and as a complication after operations to remove the primary tumor focus).
- Individual features of the intestinal structure (dolichosigma, mobile cecum, additional pockets and folds of the peritoneum),
- Hernias of the anterior abdominal wall and internal hernias.
Mechanical (obstructive) intestinal obstruction can also occur due to compression of the intestine by an external tumor or narrowing of the intestinal lumen as a result of inflammation. It is important to know that mechanical intestinal obstruction can develop not only with intestinal tumors, but also with cancers of other locations, for example, kidney cancer, liver cancer, bladder cancer, and uterine cancer.
Paralytic ileus can be the result of trauma, peritonitis, or significant metabolic disorders, such as low potassium levels in the blood. In cancer patients, paralytic intestinal obstruction may be caused by decompensation of liver and kidney function, impaired carbohydrate metabolism in the presence of concomitant diseases such as diabetes mellitus and a number of other conditions.
Spastic intestinal obstruction develops with lesions of the brain or spinal cord, poisoning with salts of heavy metals (for example, lead) and some other conditions. [9,10]