Why is this necessary?
If you have suffered deep vein thrombosis of the lower or upper extremities, your doctor will most likely prescribe you indirect anticoagulants.
The main drug in this group today, both here and abroad, is warfarin. In our country, another drug of this group is used quite widely - phenylin. Other coumarin drugs (acenocoumarol, marcumar, marivan) can be used. The recommendations given are mostly applicable to any anticoagulant. The purpose of this medication is to prevent blood clots from recurring, which could cause your condition to worsen or cause life-threatening complications. The risk of recurrence of thrombosis is quite high during the first year after the first episode of the disease, therefore, taking into account various factors, warfarin is prescribed for a period of 2 to 12 months. In rare cases, longer therapy is performed. Indirect anticoagulants have no effect on an already formed blood clot.
To determine the duration of treatment, special (including genetic) blood tests are sometimes required to identify an increased tendency to blood clots.
A very large number of patients around the world receive the treatment you have prescribed. It is used not only in phlebology, but also in such areas of medicine as vascular surgery. In addition to deep vein thrombosis, the basis for prescribing anticoagulant therapy is often previous heart attacks, cardiac arrhythmias, valve and peripheral vessel replacement, and much more.
Indications for use of Warfarin
The drug is used for the treatment and prevention of embolism and thrombosis of blood vessels. The following indications for the use of Warfarin are determined:
- venous thrombosis in acute form, as well as recurrent;
- pulmonary embolism;
- strokes , transient ischemic attacks ;
- prevention of thromboembolic complications in people who have had myocardial infarction ;
- secondary prevention of myocardial infarction ;
- prevention of thromboembolic complications in people with heart valve damage, atrial fibrillation, as well as in those who have undergone heart valve replacement;
- prevention of postoperative thrombosis .
How to monitor treatment
Carrying out antithrombotic (anticoagulant) therapy can save your life and health, but requires increased attention and mandatory compliance with the doctor’s recommendations. Warfarin is a drug that reduces the ability of blood to clot, so its excess can lead to hemorrhagic complications, i.e. to bleeding. To avoid complications, the required dose of warfarin is monitored using a blood test called INR (International Normalized Ratio). This may sometimes be referred to as INR in laboratory responses. During the entire period of taking warfarin, the INR should be in the range of 2.0 - 3.0. If the INR is less than 2.0, then blood clotting is not reduced and thrombotic complications are possible. If the INR is more than 4.0, hemorrhagic complications are very real. An increase in INR from 2.5 to 4.0 indicates the need to reduce the dose of the drug, but usually does not pose a direct threat. For some diseases, the required upper limit of INR is 4.0 - 4.4.
In the absence of the ability to determine INR, monitoring by prothrombin time (PT) is acceptable, but this method is much less reliable. No other blood tests are needed to calculate your warfarin dose. To identify the side effects of the drug, a general blood test, urine test and some biochemical tests are periodically prescribed.
Side effects of Warfarin
During treatment, the following side effects of Warfarin may occur:
- bleeding - often;
- increased sensitivity to Warfarin after prolonged treatment;
- abdominal pain, vomiting, diarrhea , anemia - uncommon;
- increased activity of liver enzymes, eosinophilia , urticaria , jaundice , eczema, necrosis , itching, rash, nephritis , urolithiasis , vasculitis , tubular necrosis - rarely.
Bleeding occurs in approximately 8% of patients receiving Warfarin. Of these cases, 1% are severe, requiring hospitalization, and another 0.25% are defined as fatal. The main risk factor for the development of intracranial hemorrhage is uncontrolled or untreated hypertension. Also, the likelihood of treatment with Warfarin increases in elderly people, with a history of gastrointestinal bleeding and strokes, with high intensity of concomitant anticoagulant and antiplatelet treatment, as well as in people with polymorphism of the CYP2C9 gene.
, coumarin necrosis may occur as a side effect of warfarin therapy . As a rule, this phenomenon begins with the appearance of swelling and darkening of the skin of the buttocks or legs, less often such signs appear in other places. Later such lesions become necrotic. In approximately 90% of cases, this side effect develops in women. It is observed from the third to tenth day of taking the medicine. Its origin is associated with a deficiency of antithrombotic protein C or S. In case of congenital deficiency of these proteins, it is necessary to start taking Warfarin with small doses and simultaneously administer heparin . If such a complication develops, treatment should be stopped and heparin administered until the lesions heal.
In very rare cases, hand-foot syndrome . This complication develops in men who suffer from atherosclerosis . This complication is characterized by the development of purple, symmetrical skin lesions on the soles of the feet and on the toes, which are accompanied by burning pain. Symptoms disappear when the medication is stopped.
How to take the drug
Warfarin is available in 2.5 milligram tablets. Most often, the “starting” and “maintenance” doses of the drug are 5 milligrams (2 tablets) per day. In many cases, for more “fine” adjustments, you will change the dose of the medicine that you take not per day, but per week. This may require either dividing the tablet in half or taking different numbers of tablets on different days. To make it easier to monitor your treatment, you may be given a special account book, or you can keep a notebook with a treatment diary, where it is useful to note the doses of warfarin, INR level, and other laboratory data.
Warfarin is taken in the entire daily dose at one time, preferably at 17:00 - 19:00. Take the tablets with water. It is not recommended to take it with food, but can be taken on an empty stomach. Phenyline is usually taken in 2 doses.
Warfarin dose selection
The most difficult and responsible stage. “Loading” initial doses of warfarin (more than 5 mg) are not recommended.
Dose selection can be carried out both with and without the use of low molecular weight heparins (Fraxiparine, Clexane), both in the hospital and on an outpatient basis. The selection period on average takes from 1 to 2 weeks, but in some cases it increases to 2 months. At this time, you will need frequent INR determinations, up to 2 - 3 times a week or daily. Each time, after receiving the next test result, your doctor will determine a change in the dose of the medication and the date of the next test.
If in several tests in a row the INR remains in the range of 2.0 - 2.5, this means that the dose of warfarin has been adjusted. Further monitoring of treatment will be much easier.
Warfarin price, where to buy
Price Warfarin Nycomed – from 115 rubles. per pack 50 pcs. Packing of tablets 100 pcs. costs on average 180 rubles.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
- Online pharmacies in KazakhstanKazakhstan
ZdravCity
- Warfarin Nycomed tablets 2.5 mg 100 pcs. Takeda Pharma Sp.
z o.o. 155 rub. order - Warfarin Nycomed tablets 2.5 mg 50 pcs. Takeda Pharma Sp. z o.o.
105 rub. order
- Warfarin tablets 2.5 mg 100 pcs. OzonOzon LLC
125 rub. order
- Warfarin tablets 2.5 mg 50 pcs. Ozon LLC
73 rub. order
- Warfarin-OBL tablets 2.5 mg 100 pcs. JSC Obolenskoe farm. company
128 rub. order
Pharmacy Dialogue
- Warfarin Nycomed (2.5 mg tablet No. 100)Takeda
RUB 161 order
- Warfarin Nycomed (2.5 mg tablet No. 50)Takeda
97 RUR order
- Warfarin Nycomed (2.5 mg tablet No. 50)Nycomed
103 rub. order
- Warfarin (2.5 mg tablet No. 50) Ozon LLC
45 rub. order
- Warfarin (2.5 mg tablet No. 100)Canonpharma Production
103 rub. order
show more
Pharmacy24
- Warfarin-FS 2.5 mg N100 tablets Pharma Start TOV, Ukraine
78 UAH order - Warfarin-FS 3 mg No. 100 tablets Pharma Start TOV, Ukraine
91 UAH order
- Warfarin 2.5 mg No. 100 tablets Takeda Pharma A/S, Denmark/Takeda Pharma Sp.z.o.o., Poland
105 UAH order
PaniPharmacy
- WARFARIN tablets Warfarin tablets. 3mg No. 30 Finland, Orion
80 UAH order
- WARFARIN tablets Warfarin tablets 5 mg No. 100 Finland, Orion
185 UAH order
- WARFARIN tablets Warfarin Nycomed tablets 2.5 mg No. 100 Denmark, Takeda Pharma
110 UAH order
- WARFARIN tablets Warfarin tablets 3 mg No. 100 Ukraine, Pharma Start LLC
98 UAH order
- WARFARIN tablets Warfarin tablets. 3mg No. 100 Finland, Orion
190 UAH order
show more
Monitoring the dose of warfarin
If the dose of the drug is selected, less frequent monitoring is sufficient - first once every 2 weeks, then once a month. The frequency of additional studies is determined separately. The need for an extraordinary determination of the INR may arise in a number of cases, which we will discuss below. If in any doubt, ask your doctor for advice.
Currently, there are portable devices for self-determination of INR (similar to systems for monitoring blood sugar levels in patients with diabetes), but their cost is very high and, in most cases of deep vein thrombosis, purchasing them is impractical.
What may affect treatment
- Any concomitant diseases (including “colds” or exacerbation of chronic diseases)
- The use of drugs that affect the blood coagulation system. This is especially true for a large class of drugs that includes aspirin. It also includes many drugs prescribed as anti-inflammatory and painkillers (diclofenac, ibuprofen, ketoprofen, etc.). As a mild analgesic during treatment with warfarin, it is better to use paracetamol in normal dosages. In any case, the need for a new medication and the duration of its use must be agreed with the attending physician. When warfarin and aspirin are prescribed simultaneously, the INR is maintained in the range of 2.0 - 2.5.
- The use of drugs that affect the absorption, excretion and metabolism of warfarin. Most often, it is necessary to take into account the prescription of broad-spectrum antibiotics and oral antidiabetic agents. However, taking any new medicine may change how warfarin works. If concomitant treatment is necessary, additional INR analysis is usually prescribed at the beginning and end of therapy.
- Diet changes.
Warfarin acts on blood clotting through vitamin K, which is found in varying amounts in food.
There is no need to avoid foods high in vitamin K! Nutrition should be complete. You just need to make sure that there is no significant change in their proportion in the diet, for example, depending on the season. If you significantly increase your intake of foods rich in vitamin K while on a stable dose of warfarin, this may greatly weaken its effect and lead to thromboembolic complications.
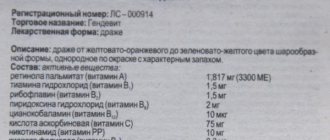
The maximum amount of vitamin K (3000 - 6000 mcg/kg) is found in dark green leafy vegetables and herbs (spinach, parsley, green cabbage), and in green tea up to 7000 mcg/kg; intermediate amounts (1000 - 2000 mcg/kg) - in plants with paler leaves (white cabbage, lettuce, broccoli, Brussels sprouts). A significant amount of the vitamin is found in legumes, mayonnaise (due to vegetable oils), and green tea. Fats and oils contain varying amounts of vitamin K (300 - 1000 mcg/kg), more of it in soybean, rapeseed, and olive oils. The content of vitamin K in dairy, meat, bakery products, mushrooms, vegetables and fruits, black tea, coffee is low (no more than 100 mcg/kg). Regular consumption of berries and cranberry juice may increase the effect of warfarin.
Small doses of alcohol with normal liver function do not affect anticoagulant therapy, but alcohol consumption must be treated with caution.
Taking multivitamins that contain vitamin K may reduce the effect of warfarin.
Frequently asked questions about warfarin treatment
1. Why is warfarin prescribed?
Warfarin is an anticoagulant - a drug that reduces blood clotting (the ability to form blood clots). Warfarin is prescribed in cases where the risk of unwanted blood clots is particularly high. The most common indications for prescribing warfarin: artificial heart valve, atrial fibrillation (the so-called “atrial fibrillation”), deep vein thrombosis, pulmonary embolism, sometimes after a heart attack, stroke, with thrombophilia (a disease in which blood clotting is increased and constantly appears). blood clots).
2. How does warfarin work?
Warfarin blocks part of vitamin K, from which prothrombin is synthesized in the liver, a substance necessary for the formation of blood clots. Vitamin K enters the body with food from green vegetables, and is also produced by bacteria living in the human intestines. Warfarin “neutralizes” part of vitamin K and the liver does not receive enough “building material” to create prothrombin. Warfarin does not dissolve existing blood clots.
3. How quickly does warfarin start and stop working after taking it?
Since warfarin interferes with the creation of new prothrombin without neutralizing the one already formed, its effect does not appear immediately. The effect of warfarin can be seen only in 3-5 days (when the previously created prothrombin is destroyed). It also takes 3-5-7 days for the liver to produce a sufficient amount of prothrombin after stopping warfarin, and blood clotting returns to normal.
4. Is warfarin dangerous? Will I have any side effects?
Warfarin is a serious drug. Failure to follow the rules for taking it can lead to serious complications. At the same time, when prescribing it, the doctor weighed the possible risks of warfarin and the risks without it, and came to the conclusion that there would be more benefit from warfarin than danger. In general, following the rules for taking warfarin and regularly monitoring blood clotting, in most cases, allows you to avoid serious complications.
5. When should you take warfarin?
The main condition is that warfarin must be taken every day, without skipping. Therefore, determine the time for taking warfarin for yourself when you will not forget to take it! In addition, you should always take warfarin at the same time and on an empty stomach. Food affects the absorption of warfarin, so it is better not to combine them. It is best to take warfarin once a day in the evening.
6. How long will I have to take warfarin?
This depends on the reason you were prescribed warfarin. For example, after installation of an artificial mechanical heart valve or with thrombophilia, warfarin will have to be taken for life. After some other heart surgeries or deep vein thrombosis, warfarin is usually prescribed for six months to a year.
7. What should I do if I forget to take warfarin?
Don't forget to take your next dose :). Under no circumstances take a double dose at your next dose! Just wait until your next dose and take your regular dose for that day.
8. I don't remember if I took warfarin. What should I do?
Nothing. If you skip one dose, there will be less harm than if you take a double dose. And in order to prevent this situation from happening again, use a pill bottle or put warfarin and other medications aside for the day in a separate box/jar. This way you will always know what you have already drunk and what you haven’t yet.
9. Should I somehow monitor the progress of warfarin treatment?
Yes, monitoring the progress of treatment is the basis of all basics. If you are not going to control your blood clotting, it is best not to start warfarin therapy at all. Treatment with warfarin is a constant balancing act between the risk of thrombosis and the risk of bleeding. And without regular tests it is impossible to maintain this balance.
About INR
10. What is INR?
INR (international normalized ratio) is one of the indicators of the blood coagulation system. It is sometimes referred to as “INR” in analyses. It is by this indicator that the effectiveness of warfarin treatment is determined.
11. What is the “target INR range”?
The normal INR for humans is about 1 (0.8 – 1.3). The purpose of prescribing warfarin is to reduce blood clotting to a level where the risk of thrombosis is significantly reduced, but the risk of bleeding is not yet too high. For different conditions, this balance point is between certain INR numbers. For example, with a mechanical heart valve, it is recommended to keep the INR between 2.5 and 3.5. These numbers are called the “target INR range”. This range may be different for different conditions.
12. How often should I check my INR?
At the stage of selecting the dose of warfarin, INR should be monitored every 3-5 days, after reaching the target range - once every 5-7 days, after receiving 3 consecutive tests in the target range, you can switch to measuring once every two weeks. In general, it is necessary to measure INR at least once a month, and preferably once a week or two. It is also necessary to check the INR if you change the dose of warfarin, change your diet, add new medications and other situations that could affect blood clotting. Remember that changes in INR levels will only be noticeable after 3-5-7 days.
13. What does it mean if my INR is BELOW the target range? What to do about it?
This means that the dose of warfarin is insufficient and there is a risk of thrombosis. In order to return to the range, you need to either reduce the amount of vitamin K in food or increase the dose of warfarin. It's better to start with the first one. If the INR has dropped below 1.6 (for a target range of 2.0-3.0) or 2.0 (for a target range of 2.5-3.5), you may need to temporarily add heparin or Clexane (ask your doctor!) .
14. What does it mean if my INR is ABOVE the target range? What to do about it?
This means that the dose of warfarin is excessive and the risk of bleeding is increased. It is necessary to either increase the intake of vitamin K from food or reduce the dose of warfarin. If the INR is no more than 4.0-4.5, then it is better to start with the first option. And only if the INR does not decline within a week, then reduce the dose of warfarin.
15. I can't seem to stay within my target range. Is it even possible?!
Maybe! It just takes time to learn how to regulate blood clotting. For this:
A. Monitor your INR regularly
b. Stick to a diet (see below)
V. To more accurately select the dose of warfarin, use combinations of tablets with different warfarin contents (2.5, 3 and 5 mg are available in Ukraine) and their parts.
d. Use an alternating regimen for taking warfarin: one dose one day, another - another, the third - the same as the first, etc. In this way, you can select the average daily dose more accurately.
d. Don't forget about the interactions of warfarin with medications, herbs, vitamins and foods!
e. Change the dose of warfarin very carefully, by 10-20% at a time and allow time for changes to appear (5-7 days).
16. For several tests in a row, my INR has been in the target range. Does this mean that the warfarin dose has been adjusted and I can stop checking my INR?
No, it doesn't mean that. INR monitoring is necessary while you are taking warfarin because clotting can vary significantly depending on external factors (food, medications, stress, etc.). Even if the indicator is stable, it is necessary to monitor the INR once a week or two and in no case less than once a month!
17. In what situations do I need an unscheduled INR check?
If there is reason to suspect or predict an exit from the target range. For example, if unmotivated large bruises appeared on the body, nosebleeds or other bleeding appeared. An unscheduled INR measurement is also necessary if your diet has changed radically or you have added/removed some medication that can affect the INR.
About lifestyle
18. Can I combine warfarin with other medications?
You can, but your warfarin dose may need to be adjusted. There is a whole list of drugs that enhance the effect of warfarin and no less those that weaken its effect. Always pay attention to the “drug interactions” section in the medication annotations and if warfarin is indicated there, be sure to check the INR 5 days after starting the drug and possibly change the warfarin dose. Don't forget to check your INR and return to your original warfarin dose after you finish taking the new drug.
19. I periodically take herbs/vitamins/dietary supplements. Could this have any effect on warfarin?
Maybe! Many vitamins (eg vitamin C, vitamin E) affect the action of warfarin. Many multivitamins contain small amounts of vitamin K, which means they significantly reduce the effect of warfarin. When choosing multivitamins, pay attention to this; take those that do not contain vitamin K. The same applies to many herbs and dietary supplements. Before taking them, think carefully about whether the expected benefit from taking them is so great as to risk “shaking” the INR. And if you still decide to take herbs/vitamins/dietary supplements, be sure to check your INR 5-7 days after they start and after they end.
20. Do I have to follow any special diet while taking warfarin?
Yes, there are certain dietary rules for people taking warfarin. They consist in the fact that there should be a stable content of vitamin K in food every day. It can be high or low, it doesn’t matter, the main thing is that it is approximately the same every day! Green vegetables and green tea contain the most vitamin K.
21. Should I change my lifestyle if I take warfarin?
Sometimes yes. To avoid dangerous bleeding, you should avoid activities and entertainment that involve an increased risk of injury (contact sports, working with cutting objects, or with a high risk of falling, even from your own height).
22. I want to go on a trip/hiking. Will warfarin therapy interfere with this?
Basically no. Just remember to take an adequate supply of warfarin with you and check your INR before leaving. Don't forget about your diet - when traveling, food often differs significantly from usual, and this can affect the INR. It is better to avoid long (more than 2 weeks) trips unless there is an opportunity to check the INR (with a portable device or at the nearest hospital). Also, always have a card/piece of paper with you indicating that you are taking warfarin and for what indications.
23. I want to get pregnant and have a baby. Would warfarin interfere with this?
Unfortunately it will interfere. Warfarin is extremely harmful to the baby, so if you are planning a pregnancy, discuss with your doctor the possibility of replacing warfarin with heparin during pregnancy.
24. Should I tell doctors that I am taking warfarin?
Yes, it is necessary, since many manipulations cannot be carried out with warfarin or require special training or support. Be prepared for the fact that doctors in some specialties may not know what warfarin is and what risks it carries, so it is better to have the instructions for the drug with you.
25. I am about to have an operation or other medical procedure. What to do with warfarin?
It all depends on how traumatic the manipulation is. For any operation, warfarin will have to be temporarily removed, perhaps replaced with heparin for a while. The same applies to such manipulations as gastroscopy, bronchoscopy, etc. Tooth extraction may require a dose reduction or discontinuation of warfarin. Other dental manipulations can be carried out without changing the dose of warfarin, but you should be prepared for prolonged bleeding from the gums, etc.
26. In what situations should I consult a doctor immediately?
a. If you have had an injury to the abdomen, chest, or head. Even if you feel well, but the blow can be described as severe, it is better to go to the hospital and make sure that there is no internal bleeding.
b. If you notice blood in your sputum, stool, urine, or if you are vomiting blood. You should also consult a doctor if you have nosebleeds that do not stop within 10-15 minutes.
c. If you have numerous large bruises on your body.
d. If you suddenly have headaches, weakness in one half of the body, blurred vision, speech impairment, abdominal pain, etc.
In each of these cases, be sure to tell your doctor that you are taking warfarin and your latest INR value.
27. Can I combine warfarin with alcohol?
You can, but it is not advisable to do so. Alcohol, by affecting the liver, enhances the effect of warfarin. In addition, even small doses of alcohol impair coordination and increase the risk of accidental injury, which can be life-threatening in a person taking warfarin.
TO MAKE AN APPOINTMENT WITH A SPECIALIST AT OUR MEDICAL CENTER, PLEASE CLICK HERE
It is important
Always tell any health care professional you see that you are taking anticoagulants. It is advisable to carry your “account” book or treatment diary with you.
Most dental procedures (except tooth extraction) can be performed without changing your treatment regimen. When removing a tooth, it is usually sufficient to use a tampon with a local hemostatic agent (aminocaproic acid, thrombin sponge).
If you have problems with blood pressure, you need to regularly monitor it and maintain it at a level not higher than 130/80 mmHg.
Warfarin and pregnancy
During pregnancy, taking warfarin is contraindicated. In the event of pregnancy, indirect anticoagulants are immediately discontinued; if further prevention of thrombosis is necessary, heparins are usually used. Therefore, if you suspect pregnancy, refrain from taking the drug until you consult your doctor.
It is possible to use warfarin during breastfeeding. Warfarin is excreted in breast milk in extremely small quantities and does not affect the baby's blood clotting processes, but for complete safety it is recommended to refrain from breastfeeding during the first three days of the mother's treatment with the drug.
Contraindications
Before taking medications, you need to take into account the contraindications that are indicated in the instructions for the drug:
- manifestation of high sensitivity to the components of the product or suspicion of hypersensitivity;
- acute bleeding;
- severe liver and kidney diseases;
- the first trimester of pregnancy and the last 4 weeks of gestation;
- acute DIC syndrome;
- thrombocytopenia;
- lack of proteins C and S;
- varicose veins of the digestive tract;
- aneurysm ;
- increased risk of bleeding, including hemorrhagic disorders ;
- stomach and duodenal ulcers;
- severe wounds, including post-operative wounds;
- lumbar puncture;
- bacterial endocarditis;
- hypertension malignant;
- intracranial hemorrhage;
- hemorrhagic stroke.