Dentistry / Media about us / Dermatitis and the role of the Leptotrichia bacterium in their occurrence
Seborrheic and oral dermatitis are one of the pressing problems of dermatocosmetology.
Doctors note that the number of patients with these diseases, which manifest themselves as significant cosmetic defects of the skin in the form of oily sheen, peeling and rashes accompanied by itching, is constantly growing.
Why does dermatitis occur? How does he make himself known? And what to do to cope with this condition? The questions are answered by a dermatovenereologist (adult), dermatovenereologist (children), cosmetologist of the SCNT “NOVOSTOM” Natalya Vladimirovna Musayelova.
What, when, why and why
In recent years, the role of the bacterium Leptotrichia bucalis has been proven in the occurrence of seborrheic dermatitis.
Seborrheic dermatitis is based on chronic inflammation of the skin, associated with an increase in the quantity and change in the quality of sebum with localization in those areas of the scalp and torso where the sebaceous glands are developed - the scalp, eyebrows, eyelashes, naso-cheek folds, ears, behind-the-ear spaces, anterior area chest, interscapular and groin areas.
Damage to the skin of the scalp is observed in the form of dandruff, scales, crusts, thinning and thinning of hair, very often accompanied by itching and irritation. You can often see yellowish scaly crusts and hemorrhagic crusts formed as a result of scratching. Often the skin of the forehead, behind-the-ear areas, and ear canal areas is involved in the process.
Foci of redness and papules appear on the smooth skin of the face, back, and chest. Very often, the occurrence of these dermatitis can be traced to genetic predisposition, stress, gastrointestinal diseases, hormonal imbalances and the influence of external and climatic factors.
The leading role in the pathogenesis of seborrheic dermatitis of the scalp and dandruff is assigned to yeast-like fungi.
These fungi are a permanent component of the microflora of healthy skin in more than 90% of the population. They use the secretions of the sebaceous glands for their growth and development. The Malassezia futur variety is most often found on the scalp. Pityrosporum orbiculare - on the skin of the trunk and face. Stressful situations worsen the course of seborrheic and oral dermatitis due to changes in hormonal levels. In men 40-60 years old, seborrheic dermatitis is observed more often than in women, perhaps this is due to a decrease in the male hormone testosterone.
Thus, the above reasons lead to the spread and increase in the number of previously saprophytic microorganisms and the development of foci of inflammation with impaired immune skin response.
In recent years, there has been increasing interest in anaerobic microorganisms, namely bacteria of the genus Leptothrichia and Leptothrix.
One of the varieties is Leptotrichia bucalis, an inhabitant of the human oral cavity. Under microscopy, Leptotrichia look like straight or slightly curved rods with a diameter of 1.0 - 1.5 microns with pointed or rounded ends. With prolonged parasitism of leptotrichia on the mucous membranes of the oral cavity and genital organs, leptotrichosis infection leads to a general decrease in the resistance of the macroorganism, which is a trigger factor in the development of inflammatory reactions on the skin and mucous membranes
For diagnosis, scrapings from lesions are studied. The main criterion for diagnosing leptotrichosis lesions is the detection of the pathogen (10-15 bacteria in all fields of view) with the presence of inflammatory elements (leukocytes, histiocytes). Without the absence of inflammatory elements, bacterial carriage should be considered.
The tonsils, lateral and posterior parts of the pharynx, and tongue are mainly affected. Leptotrichosis is a pseudomycotic lesion of the oral mucosa. Objectively: a grayish-whitish coating appears on the mucous membrane of the oral cavity, tongue, and arches of the soft palate, turning into a light brown color, which cannot be easily removed with a spatula.
The diagnosis of the disease is made on the basis of characteristic clinical data and the microscopic picture of the specimen.
Microscopy in scrapings from the mucous membrane of the hard palate reveals spores and pseudomycelium of the genus Candida from the tongue of leptotrichia with elements of inflammation. Therefore, the correct interpretation of bacterioscopic preparations should be carried out, taking into account that the treatment of candidiasis and leptotrichosis is not the same.
Features of the pathogen
Leptothrix are gram-negative, filamentous bacteria that do not form spores and prefer an anaerobic environment with very little oxygen (such bacteria are called microaerophilic).
Their name comes from Latin words meaning “fine hair”. In a smear, leptothrix looks like long thin or thick rods, which are arranged in chains resembling hairs. The external resemblance to actinomycete fungi initially led to a classification error: for a long time leptothrix was classified as a fungus.
They are usually grouped under the general name of the genus Leptothrix species (spp.).
Some researchers attribute Leptothrix to a special variety of lactobacilli, modified under the influence of environmental conditions.
They noticed that some women who go to gynecologists with complaints of heavy discharge have bacteria in their smears that form long chains.
In women who do not have symptoms of infection, lactobacilli are grouped in chains ranging from 5 to 15 microns in length. In women with complaints of heavy discharge, the length of one chain can reach 40-75 microns.
Until now, in the medical literature, the names of bacteria leptothrix and leptotrichia are considered synonymous. This is due to the confusion and difficulty of cultivating them.
Attention! In the new classifications, these are two different genera - Leptothrix and Leptotrichia! Be careful, bacteria cause completely different diseases!
Treatment of dermatitis
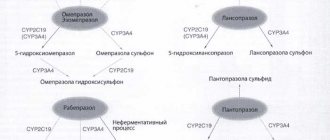
Based on the results of microscopic examinations and studies of the immune status, the clinical picture of patients with seborrheic, oral dermatitis and leptotrichosis, it is necessary to use complex therapy .
To treat mucous membranes, bacteriophages (staphylococcal, complex) and antiseptic solutions (Betadine and Miramistin) are used by application to the tongue or for rinsing the mouth, as well as antimycotic (Orungal, Lamisil) and antiparasitic (Trichopol, Dekaris) therapy orally.
To treat skin inflammation, antibacterial (Metrogyl) and antifungal (Nizoral, Triderm, Akriderm GK, etc.) drugs are used in combination.
Source
What symptoms may be observed?
Lactobacilli begin to predominate in the vaginal microflora after puberty. But why Leptothrix infection occurs is not known exactly.
There is an opinion that bacteria often appear after self-diagnosis and improper treatment of candidiasis. Anti-thrush medications are readily available, and women often skip gynecological appointments.
Leptothrix is often combined with the following pathogens:
- 1Trichomonas.
- 2Gardnerellas.
- 3 Candida.
- 4Chlamydia.
Manifestations of infection are nonspecific; in Western literature it is sometimes called the term “lactobacillosis.” It is not sexually transmitted and does not cause any symptoms in men.
The most common symptoms women experience are:
- 1 Copious, white or clear vaginal discharge without an unpleasant odor or lumps, sometimes resembling water.
- 2Itching and burning in the vagina and vulva area.
- 3The acidity of the vaginal environment remains normal.
- 4Sometimes a woman complains of discomfort and burning when urinating.
- 5During examination, the doctor, as a rule, does not see redness of the vaginal walls and swelling - obvious signs of inflammation.
Complaints often appear in the second phase of the cycle, when menstruation approaches. There is evidence that high concentrations of hydrogen peroxide and lactic acid in the vagina lead to damage to epithelial cells and nerve endings, which can cause the development of vulvodynia.
During pregnancy, the detection of leptothrix is also accompanied by copious liquid discharge, which constantly wets the underwear.
Leptotrichosis, that is, an infection caused by leptotrichia , is characterized by slightly different symptoms:
- 1Increase in the amount of vaginal discharge, change in color (gray, white-gray).
- 2The appearance of an unpleasant odor, typical of bakvaginosis.
- 3Shift of acidity to the alkaline side.
- 4Pain during sexual intercourse (dyspareunia).
- 5Itching and burning in the vagina.
One of the types of leptotrichia - Leptothrix amnionii - can cause the following complications:
- 1Premature termination of pregnancy.
- 2Choriamnionitis.
- 3Low fetal weight at birth.
- 4Postpartum sepsis in immunosuppressed women in labor.
- 5Infection of a newborn.
Identification of this pathogen is extremely rare.
Treatment regimens for leptothrix during pregnancy and beyond
When treating vaginal symptoms of pathology, standard regimens are used to combat bacteria. In the acute phase of the disease, topical antifungal drugs (vaginal suppositories and tablets) are used:
- "Gyno-travogen" (iconazole nitrate) - vaginal suppositories (0.6 g), 1 time per day;
- "Clotrimazole" - tablets (0.1–0.2 g), cream (1–2%);
- "Miconazole", "Gynodactarin" - suppositories (0.1 g);
- "Econazole", "Ginopevaril" - suppositories (0.15 g).
To get rid of bacteria throughout the body, systemic drugs are used, they guarantee relief from vaginal symptoms:
- “Orungal” - take a course of capsules (0.1 g) for 3 days;
- "Ketoconazole" - tablets (0.2 g) 5 days;
- "Diflucan" - capsules (0.05–0.15 g).
Antifungal antibiotics are also used:
- “Pimafucin” - a course of tablets, designed to be taken 4 times a day, 1 piece, 7-12 days;
- "Amphoglucamine" - tablets, 2 times a day, 1 piece, 10-14 days;
- “Nystatin” - tablets (500 thousand units) 4 times a day, course - 2 weeks;
- Clindamycin is an antibiotic for oral administration, the dosage depends on the severity of the disease.
Broad-spectrum antimicrobial and combination drugs:
- metronidazole - tablets for oral administration, 500 mg 2 times a day for a week;
- Terzhinan - vaginal tablets, course on average 10 days.
Vaginal antiseptics:
- "Hexicon" (chlorhexidine);
- "Betadine" (povidone-iodine).
1-2 times a day for a week.
After treatment with any vaginal antimicrobial drugs, the amount of beneficial flora and lactobacilli in the vagina decreases; you can simply wait until everything returns to normal on its own or use drugs to restore the microflora:
- "Lactozhinal";
- "Acilact";
- "Lactonorm";
- "Vagilak";
- "Gynoflor" and the like.
For the treatment of pregnant women, it is permissible to use only a local type of therapy - suppositories, vaginal balls, creams, etc. Other drugs can harm not only the health of the mother, but also the unborn child.
The pathology is usually asymptomatic and the detection of leptothrix bacteria in a smear (if there are no signs of an inflammatory process) is not at all a reason for immediate treatment, since it is also detected in healthy people. This is an opportunistic microorganism. The only exceptions are expectant mothers and a certain subspecies of bacteria.
If you need to undergo treatment for dysplasia, “cauterize the erosion”, and leptothrix is detected in the smear, while the number of leukocytes is normal, there are no inflammatory manifestations - this is not a reason to postpone the procedure.
Back to contents
This is also interesting
- Tank culture from the cervical canal for flora and sensitivity to antibiotics
- What does coccobacillary flora mean, does it need to be treated and how?
- Streptococcus agalactiae in a smear from the vagina, urethra and cervical canal - what to do if detected
Reviews and comments
- Mikhail 41 years old:
March 27, 2022 at 4:44 pmHello. A year ago I saw a dermatologist about seborrheic dermatitis and cheilitis. I was treated with antifungal tablets for 1 month. Symptoms appeared after some time and appeared again. The dermatologist looked at the root of the tongue and said that it was covered with a yellowish-brown coating, then she prescribed a smear from the root of the tongue. They found leptotrichia. She prescribed metronidazole. Now about a year has passed. The tongue is yellowish-brown again, the drool is yellow. The immune system is weak, stress. A year ago I donated blood: lymphocytosis, neutropenia. The hematologist-oncologist said that he didn’t see anything wrong. That there were signs of an infectious inflammatory process. And to re-donate the blood in a month. But he didn’t send it. 2 months ago I took ampicillin for 7 days because of acute respiratory viral infection. I am taking antipsychotics. Now my tongue is yellowish-brown again. I have stomatitis. Tell me how to get rid of leptothyrichia posta
Answer
Diagnostic methods
In gynecology, the first stage of diagnosis is a speculum examination and bimanual examination. During the examination, the doctor will not notice any changes in the vagina or cervix.
Two-handed examination in the absence of inflammation in the appendages and uterus is painless. The acidity of the vaginal environment is within normal limits.
- Leptothrix is detected in a simple smear on the flora. Its characteristic feature is its arrangement in the form of long thin chains according to the dot-dash principle.
- A modern diagnostic method is the Femoflor analysis. It is distinguished by the speed of obtaining results, as well as the ability to detect different representatives of normal flora and count their number.
The normal value is 104. If this indicator is exceeded, dysbiosis or nonspecific vaginitis is diagnosed.
Differential diagnosis is carried out with vaginal candidiasis and bacterial vaginosis. Each of these pathologies has characteristic symptoms that make it easy to distinguish them from each other.
Leptothrix in a smear during pregnancy: diagnosis and consequences
It is worth noting a bacterium from the same family - Leptotrichia amnionii. French scientists managed to isolate it from the amniotic fluid of women who gave birth prematurely. The bacterium caused chorioamnionitis - inflammation of the membranes. The result of this was premature rupture of amniotic fluid and termination of pregnancy.
But the negative impact on the fetus did not stop there. In addition to prematurity and all the problems associated with it, bacteremia was recorded in infants, the presence of the same infectious pathogens in the blood as in the amniotic fluid (water).
Apparently, the bacterium has this effect due to a physiologically determined decrease in the mother’s immunity during pregnancy.
Only the attending physician, a gynecologist who is managing the pregnancy, can confirm or refute the diagnosis. Expectant mothers undergo flora smears at least twice during pregnancy. And if the analysis turns out to have a lot of leukocytes, a competent doctor will prescribe another, additional test - vaginal culture . It is also called cultural research. It takes about a week to complete. Task: to identify which specific microorganisms caused the inflammatory process and which antibiotics they are sensitive to, that is, to prescribe the most effective drug.
It is in the culture that Leptothrix is detected. It must be treated necessarily in the presence of symptoms and (or) in case of confirmation of its subtype - amnionii, even a small amount of which can lead to fetal death.
The PCR test, which is also taken by expectant mothers, helps to identify hidden sexually transmitted infections. They often occur in parallel with leptotrichosis and are dangerous for the fetus.
Back to contents
Clinical picture: symptoms and signs
Affecting the mucous membranes of the vagina and cervix, the pathology manifests itself as a gray coating on the walls, and vaginal discharge also becomes gray. And in addition, redness, itching and burning, which intensify during sex. The female body does not show any other reactions. At least in the “non-pregnant” state and with normal immunity.
If a woman has concomitant inflammatory diseases of the pelvic organs, for example, endometritis, parametritis, salpingitis, then broader symptoms are possible. This is an increase in temperature to 39-40 degrees, headache and muscle pain, dehydration. General intoxication of the body occurs. Such symptoms appear mainly in expectant mothers when leptothrix enters their blood. The same bacterium provokes severe abdominal pain in them. The amniotic membranes are also affected. A child becomes infected with the bacteria in utero .
Back to contents