Genferon
Genferon (recombinant human interferon alpha-2 + taurine_benzocaine) is a complex immunomodulatory drug with an antiviral effect. Interferons are biologically active proteins that are formed in the cell in response to the invasion of viruses, exposure to allergens or mutagens. Today, biotechnology is considered one of the most advanced technologies for obtaining interferon preparations. It does not involve the use of human blood as a raw material, which means there is no need to disinfect synthesized drugs. A Russian biotechnological company created the drug Genferon in the form of vaginal and rectal suppositories. This drug is widely in demand today in the complex treatment of infectious and inflammatory diseases of the urogenital tract, including infections caused by trichomonas, chlamydia, mycoplasmas, ureaplasmas, genital herpes, vaginal candidiasis, bacterial vulvovaginitis, genital warts. The key component of Genferon is interferon-alpha 2b, which has a complex antiviral, antimicrobial, cytostatic and immunomodulatory effect. It comes into play even before immune mechanisms are activated, acting as the first line of defense against invading pathogens. Interferon carries out its action indirectly through two enzymes synthesized with its participation, one of which cleaves viral RNA, the other suppresses the formation of new viral proteins.
The result is a decrease in the number of viral particles by several orders of magnitude. But interferon is valuable not only for its antiviral effect: it is also active against Staphylococcus aureus, Toxoplasma, Chlamydia, Legionella, Cryptococcus, and yeast. Another important component of Interferon is taurine. This amino acid has the ability to restore the structure of affected tissues, which is ensured by the presence of immunomodulatory, antioxidant, membrane-stabilizing and osmoregulatory properties. Taurine neutralizes the destructive effect of free radicals that are massively formed at the site of inflammation, which prevents further destruction of cell membranes and damage to cell DNA. The anti-inflammatory properties of taurine promote rapid epithelization and tissue repair in the inflammatory zone. This amino acid has the ability to potentiate immune reactions, activating the proliferation of cells that carry out the immune response. The third component of Genferon is the anesthetic benzocaine, whose task is to quickly eliminate discomfort (itching, burning, etc.) when administering a suppository. The combination of the neuromodulatory effect of taurine with the analgesic properties of benzocaine ensures that the quality of life of patients taking Genferon is maintained at a consistently high level.
The role of interferon therapy in the treatment of nonspecific vaginitis
According to numerous observations, Ureaplasma and Mycoplasma are the leading etiological agents of inflammatory diseases of the female genital area, which lead to severe reproductive dysfunction (cervicitis, endometritis, salpingo-oophoritis, choreoamnionitis, neonatal infections, etc.). The frequency of detection of these bacteria in women of reproductive age reaches 46-48%, and in the presence of a chronic inflammatory process in various parts of the reproductive system - up to 70%. Very often there is a joint detection of ureaplasmas, mycoplasmas and anaerobic microflora.
Table 1. Main clinical manifestations of nonspecific vaginitis
Table 2. Regimens for the use of antibacterial drugs
Figure 1. Comparative effectiveness of treatment of nonspecific vaginitis with study drugs
Mycoplasmas belong to the class Molecutes
family
Mycoplasmataceae
, genus
Mycoplasma
.
Ureaplasma
(representative -
Ureaplasma urealyticum
belongs to the same family - microorganisms capable of secreting the enzyme urease, which breaks down urea. These are small (mycoplasmas with a diameter of 3-5 microns, ureaplasmas - 10-30 microns) gram-negative microorganisms, characterized by significant polymorphism of microstructures and a variety of forms of reproduction, can be detected in the genitourinary organs, including in practically healthy women. Their structure is more similar to viruses; they are distinguished from bacteria by the absence of a rigid cell wall.
Ureaplasmosis is transmitted through sexual contact, and therefore many authors classify this disease as a sexually transmitted infection. Factors that enhance the potential pathogenicity of Ureaplasma
, are: disorders of immunological reactivity, hormonal imbalance, surgical interventions, as well as previous or concomitant diseases of inflammatory origin, pregnancy, childbirth, termination of pregnancy.
The main method of spread of Ureaplasma urealyticum
– along the length of the inner lining of the genitourinary tract. It is also impossible to exclude the possibility of lymphogenous and hematogenous spread.
In the treatment of ureaplasmosis and mycoplasmosis, antibiotics are used that inhibit the synthesis of membrane and intracytoplasmic proteins. Due to the absence of a cell wall, these microorganisms are resistant to antibiotics that inhibit its synthesis, in particular, drugs of the penicillin group. For the purpose of immunocorrection, a wide range of immunomodulatory agents are used, aimed at both innate and adaptive immunity. Therapy should help normalize the vaginal microbiocenosis, as well as prevent relapses of the disease. In addition, important aspects are good tolerability of the drug and ease of use.
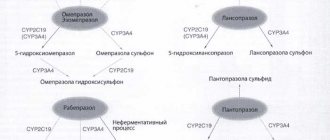
In recent years, interferon-a preparations, as well as inducers of endogenous interferons, have found widespread use in the combination therapy of nonspecific vaginitis.
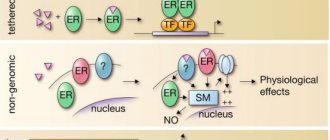
Interferon-a has antiviral, immunomodulatory and antiproliferative effects. The antiviral effect is mediated by the activation of a number of intracellular enzymes that have a direct inhibitory effect on viral replication. The immunomodulatory effect is manifested, first of all, by enhancing cell-mediated reactions of the immune system, which increases the effectiveness of the immune response against viruses, intracellular parasites and cells that have undergone tumor transformation. This is achieved by activating CD8
+
T
-killers,
NK
-cells, increased differentiation
of B
-lymphocytes and their production of antibodies, activation of the monocyte-macrophage system and phagocytosis, as well as increased expression of molecules of the major histocompatibility complex type I, which increases the likelihood of recognition of infected cells by cells of the immune system. Activation under the influence of interferon of leukocytes contained in all layers of the mucous membrane ensures their active participation in the elimination of pathological foci; in addition, due to the influence of interferon, the production of secretory immunoglobulin A is restored.
The widespread use of interferon preparations, primarily of genetic engineering origin, in healthcare practice both in our country and abroad is due to the fact that interferons are the most important link in the reactions of innate immunity in a wide variety of diseases. The use of interferon preparations is especially relevant for infectious and inflammatory diseases of the urogenital tract, in the pathogenesis of which viral-bacterial associations and secondary immunodeficiency, often expressed in the suppression of interferon-α production, play a significant role.
Experimental studies and experience in the practical use of interferon preparations have proven that their parenteral administration is not advisable for all diseases. Drugs intended for local use (ointments, suppositories, drops, etc.) are more effective for a number of nosological forms, as they are able to provide higher concentrations of the drug directly at the lesion site in the absence of side effects characteristic of parenteral administration of high doses of interferon. However, it should be noted that in the treatment of infectious and inflammatory diseases of the urogenital tract, not only the local effect of interferon is important, but also the general one, which makes it possible to achieve a systemic immunomodulatory and antiviral effect. Of particular importance in the treatment of urogenital infections is the accumulation of the drug in the pelvic organs, due to the fact that the spread of infection in these diseases is often ascending. Therefore, data on the pharmacokinetics of interferon preparations administered in the form of suppositories are of great practical interest.
The use of interferon drugs in complex therapy of patients with nonspecific vaginitis leads not only to an improvement in the clinical condition of patients, but also to the restoration of immune status. It should be noted that the changes in immune reactivity are reversible, the indicators of which are normalized after treatment, which is combined with the reverse development of clinical signs of the disease. Since topical application of interferons has fewer side effects than parenteral administration, the scope of their use is rapidly expanding. One of the drugs in this group is Genferon, which has found its use in the treatment of a wide range of infectious and inflammatory diseases of the urogenital tract, including genital herpes, human papillomavirus infection, ureaplasmosis, mycoplasmosis, chlamydia, recurrent vaginal candidiasis, bacterial vaginosis, etc.
Genferon is a combination drug, the effect of which is due to the medicinal properties of the components (IFN-a 2b
, taurine, anesthesin), included in its composition. The effects of interferon-a described above are potentiated by the action of taurine, which has regenerative, reparative, membrane-protective, antioxidant and anti-inflammatory properties. Anestezin is a local anesthetic that prevents pain. This combination of components seems to be very rational for the treatment of infectious and inflammatory diseases of the urogenital tract, as well as disorders of the vaginal microbiocenosis.
The purpose of our study was to comparatively study the clinical effectiveness of the drug Genferon, which is used in the complex therapy of patients with nonspecific vaginitis. Treatment was recommended for those patients who, when tested for the presence of Ureaplasma urealyticum
and
M.genitalis,
a high titer of the pathogen was detected (>104 CFU/ml). Recovery was assessed according to generally accepted standards of care. The criteria were: elimination of clinical manifestations of the disease and elimination of the infectious agent.
Materials and methods
A survey of 60 women aged 18-36 years with ureaplasma and mycoplasma infections was carried out.
Group I - 20 patients received antibacterial therapy and vaginal suppositories Kipferon, group II - 20 patients - were prescribed Viferon at a dose of 1,000,000 IU 2 times a day rectally in combination with antibacterial therapy, in group III 20 patients received antibacterial therapy and Genferon suppositories dose of 500,000 IU 2 times a day vaginally. The course of treatment was 10 days in all groups (Table 1).
Tetracyclines, macrolides, and ofloxacins were used to treat ureaplasma and mycoplasma infections. The scheme for the use of antibacterial drugs is presented in Table 2.
After a course of antibiotic therapy (after 7-10 days), in order to restore the vaginal microbiocenosis, it was recommended to carry out therapy with eubiotics (Acilact, Bifidumbacterin) for 7 days.
Control of cure was carried out 10 days after the end of therapy (cultural examination of the discharge) and further, during 3 menstrual cycles (sampling was carried out after the end of menstruation in 1-2 days).
Most patients had concomitant inflammatory diseases of the vagina. For bacterial vaginosis, ornidazole 500 mg 2 times a day for 3 days was prescribed, for vaginal candidiasis - Flucostat 150 mg 2 times with an interval of 7 days. Throughout the treatment, patients used barrier contraception methods. During the entire treatment and subsequent monitoring, the use of immunomodulatory drugs other than those studied was not recommended. The distribution of patients into groups was carried out randomly using the random sampling method. During the study, a physical examination, PCR diagnostics, bacteriological examination, microscopy of Gram-stained smears, cytological examination of Papanicolaou-stained smears, and colposcopy were carried out.
Criteria for cure of ureaplasma and mycoplasma infections: negative result of bacteriological examination during 3 menstrual cycles, absence of local inflammatory phenomena.
Studies for the presence of the pathogen were carried out using Mycoplasma duo
(BIO-RAD
, France), which make it possible to determine the concentration of the pathogen in the test material. The detection of a pathogen in the test material in more than 104 CFU/ml indicated the presence of a pronounced infectious process. A cytological examination was carried out, and the condition of the vaginal flora was assessed. The material was collected using cytobrushes and Volkmann spoons.
Baseline characteristics of patients
An analysis of the anamnesis of 60 patients with diagnosed ureaplasma and mycoplasma infections showed that young patients aged 18-36 years old, most of them with a burdened obstetric and gynecological history, consulted a doctor with complaints. Of the previous genital tract infections, the most common were: ureaplasmosis - 30%, chlamydia - 14%, HPV - 7%, CMV, HSV and candidiasis were previously encountered in 3% of patients. 29 (48.3%) of the examined patients had a history of chronic inflammatory diseases confirmed during the study. Chronic salpingoophoritis and chronic cystitis predominated; 40% of patients were referred for consultation to a urologist. Cervical ectopia was detected in 10 patients (34.5%). An assessment of the symptoms of the diseases showed that frequent complaints were discharge from the genital tract of varying intensity, burning and itching in the vagina and vulva, and nagging pain in the lower abdomen.
When examining for the presence of Ureaplasma
and
Mycoplasma,
a high titer of the pathogen (>104 CFU/ml) was detected in 100% of those examined.
Fungi of the genus Candida
were detected in 20% of patients, bacterial vaginosis in 13.3% (8 patients).
results
The results of the control bacteriological study demonstrated the high effectiveness of the treatment.
In the group of patients in whose complex treatment Genferon was used, a higher frequency of elimination of the infectious agent was achieved than with the use of other immunotropic drugs. A positive result was obtained in 18 patients (90%) in the “antibacterial drug + Genferon” group. Re-detection of the pathogen after treatment with antibacterial drugs in combination with Genferon was observed in 2 patients (10%). However, these patients did not have any clinical manifestations of the disease. A bacteriological examination for the presence of ureaplasmas and mycoplasmas revealed a low titer of the pathogen (4 CFU/ml), which indicated the carriage of these pathogens and the absence of an infectious process. These patients were not given a second course of treatment for nonspecific vaginitis; it was recommended that bacteriological examination be carried out during three menstrual cycles. However, no growth of pathogens was detected - the titer remained low.
At the same time, when using antibacterial therapy and Viferon, a positive result was observed in 75% of patients, and when using antibacterial therapy and Kipferon - in 80% of patients (Figure 1).
Discussion
Despite the availability of a wide range of antibacterial and immunomodulatory drugs, the problem of recurrent urogenital infections of bacterial etiology is still relevant. Patients diagnosed with nonspecific vaginitis are regular visitors not only to the gynecologist’s office, but also to the urologist.
Analysis of the results of this study indicates that complex therapy of ureaplasma and mycoplasma infections using the drug Genferon is most effective. The use of antibacterial therapy in combination with Genferon allowed achieving a positive result in 90% of patients.
The use of the drug Genferon in combination with antibacterial therapy is well tolerated by patients, does not cause local or systemic reactions, reduces pain, promotes the elimination of the pathogen, and reduces the frequency of disease relapses.
The results of the study allow us to formulate the following recommendations for the use of the drug Genferon in the treatment of nonspecific vaginitis: the appointment of an antibacterial drug after determining sensitivity during a cultural study and the parallel administration of Genferon at a dose of 500,000 IU 2 times a day vaginally for 10 days. After a course of antibiotic therapy to restore the vaginal microbiocenosis, prescribe eubiotics for 7-10 days.
Genferon® (Genferon)
GENFERON® is a combination drug, the effect of which is determined by the components included in its composition. Has local and systemic effects.
The composition of the drug Genferon® includes recombinant human interferon alpha-2b, produced by a strain of the bacterium Escherichia coli, into which the human interferon alpha-2b gene was introduced using genetic engineering methods.
Interferon alpha-2b has antiviral, immunomodulatory, antiproliferative and antibacterial effects. The antiviral effect is mediated by the activation of a number of intracellular enzymes that inhibit viral replication. The immunomodulatory effect is manifested, first of all, by enhancing cell-mediated reactions of the immune system, which increases the effectiveness of the immune response against viruses, intracellular parasites and cells that have undergone tumor transformation. This is achieved through the activation of CD8+ T killer cells, NK cells (natural killer cells), increased differentiation of B lymphocytes and their production of antibodies, activation of the monocyte-macrophage system and phagocytosis, as well as increased expression of molecules of the major histocompatibility complex type I, which increases the likelihood recognition of infected cells by cells of the immune system. Activation under the influence of interferon of leukocytes contained in all layers of the mucous membrane ensures their active participation in the elimination of pathological foci; in addition, due to the influence of interferon, restoration of the production of secretory immunoglobulin A is achieved. The antibacterial effect is mediated by reactions of the immune system, enhanced under the influence of interferon.
Taurine helps normalize metabolic processes and tissue regeneration, has membrane-stabilizing and immunomodulatory effects. Being a strong antioxidant, taurine directly interacts with reactive oxygen species, the excessive accumulation of which contributes to the development of pathological processes. Taurine helps maintain the biological activity of interferon, enhancing the therapeutic effect of the drug.
Benzocaine (anesthetic) is a local anesthetic. Reduces the permeability of the cell membrane to sodium ions, displaces calcium ions from receptors located on the inner surface of the membrane, and blocks the conduction of nerve impulses. Prevents the occurrence of pain impulses at the endings of sensory nerves and their conduction along nerve fibers. It has an exclusively local effect, without being absorbed into the systemic circulation.