Modern gynecology has a number of hormonal drugs that help in the treatment of uterine fibroids. One of them is “Buserelin”. Treatment of fibroids with Buserelin Long and other drugs based on buserelin acetate allows one to achieve good results in the initial stages of the disease, as well as as a component of preoperative preparation for removal of fibroids.
Please note: reviews of “Buserelin” for fibroids can be read on our website. In addition, you can ask our experts any questions you have about this product and receive detailed answers. However, do not forget that only your attending physician can prescribe treatment with this drug in accordance with diagnostic studies and your individual indications. You should not self-medicate with this drug, as it has a number of side effects that can cause serious harm to your health.
What is "Buserelin"?
“Buserelin” for the treatment of fibroids is a hormonal drug (antiandrogen, antigonadotropin, antiestrogen), which is produced in various forms:
- nasal spray;
- implants;
- lyophilisate for the preparation of suspension for injection;
- injection;
- drops.
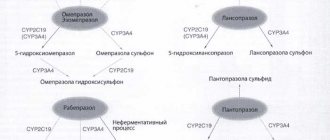
Its active ingredient is buserelin acetate - a substance from the groups of hormones of the hypothalamus and pituitary gland, antagonists and gonadotropins, as well as antitumor hormonal agents. The substance is able to bind to the receptors of pituitary cells and stimulate a short-term increase in the level of sex hormones in the blood plasma. Use of the drug for two weeks leads to a blockade of the gonadotropic function of the pituitary gland (the process resumes after stopping the drug) and, as a result, a decrease in the level of estradiol in the blood. As a result, this makes it possible to stop the development of myomatous nodes.
The role of buserelin in the treatment of common forms of prostate cancer (PCa).
The role of buserelin in the treatment of common forms of prostate cancer (PCa).
S.V. Mishugin, A.A. Drobyazko, A.A. Mordovin, A.A. Gritskevich, I.G. Rusakov.
Since 1941, following a study published by Huggins and Hodges demonstrating the dependence of prostatic cells on androgens, hormone therapy (HT) has been the mainstay of treatment for locally advanced and metastatic PCa [1]. The basis of any HT strategy is the principle of androgen blockade, which can be achieved by turning off the production of endogenous testosterone [2], as well as stopping the androgenic effect due to the competitive action of medicinal agents [3].
Currently, the main method of androgen deprivation is medical castration using LHRH agonists [4]. Today, preference is given to drug androgen deprivation rather than surgical castration. This is due to the psycho-emotional state of patients after surgery and many side effects, with an equal clinical effect, which is reflected in a number of studies. It is also possible to use intermittent hormone therapy regimens, which leads to regression of adverse reactions during temporary drug withdrawal [5,6].
One of the drugs of this group widely used in clinical practice is buserelin.
The drug buserelin is enclosed in microspheres with different resorption periods, the basis of which is a biosoluble copolymer of DL lactic and glycolic acids. Microspheres in the form of an aqueous suspension are injected deeply intramuscularly. After injection of the drug, a gradual release of the LHRH analogue from the surface of the microspheres begins, which during the first few days leads to stimulation of the synthesis of gonadotropins, and then to desensitization of the pituitary gland and blockade of the pituitary-gonadal axis. Subsequently, the microspheres, undergoing biodegradation in tissues, slowly release the LHRH analogue they contain, long-term maintaining the concentration of the drug in the blood necessary for desensitization of the pituitary gland [7,8,9].
From the beginning of December 2011 to December 2014, we observed 142 patients with prostate cancer aged 56 to 70 years who were treated with LHRH analogues. The average age of patients was 64.6 years.
Before the start of treatment, all patients underwent an examination, which included a survey, examination, and determination of PSA levels in the blood serum (at least 7-10 days after transrectal/transurethral manipulations). To assess the local extent of the tumor process, a digital rectal examination was performed in all cases. To determine the location, size and extent of the primary tumor, all patients underwent TRUS of the prostate. After receiving the measurement data, the prostate volume was calculated using software. In order to identify regional and distant metastases, transabdominal ultrasound of the abdominal organs, retroperitoneum and pelvis, chest radiography, and bone scanning were performed in all cases. To clarify the extent of the primary tumor and the condition of the pelvic lymph nodes, patients underwent CT or MRI of the pelvis. Also, all patients underwent clinical and laboratory tests (analyses of the general, biochemical composition of the blood, its coagulation system, general urine analysis and bacteriological examination of urine (as indicated), electrocardiography). To verify the diagnosis, all patients underwent transrectal biopsy of the prostate gland under ultrasound guidance.
75 had locally advanced PCa, 67 had generalized PCa (Table 1). The patients are divided into two groups.
In the first group (n=55), patients received therapy with the drug Buserelin-depot, in the second (n=87) - one of the other LHRH analogues (goserelin, leuprorelin, triptorelin). The period of drug treatment was at least 6 months.
Table 1. Distribution of patients by disease stage
| Disease stage | Buserelin (n=55) | Other LHRH analogues (n=87) |
| T2N1Mo | 7 | 12 |
| TZNoMo | 26 | 44 |
| T3NoM1 | 10 | 15 |
| T3N1M1 | 5 | 9 |
| T4N1M1 | 7 | 7 |
| Total | 55 | 87 |
At the time of inclusion in the study, 137 (96.5%) of 142 men had complaints. The main symptoms of the disease were urinary disorders (77.6% of cases in the group of patients receiving Buserelin and 66.7% in the group receiving other LHRH analogues), pain of various locations caused by the primary tumor (5.5% of cases in the first group and 13.8% in second), bone metastases (30.9% of patients from the first group and 35.6% from the second), as well as impaired outflow of urine from the collecting system (23.6% of patients from the first group and 17.2% from the second) (Table 2 ).
Table 2. Complaints of 142 patients with advanced prostate cancer.
| Complaint | Number of patients | |
| those receiving Buserelin (n-55) | receiving other LHRH analogues (n-87) | |
| Dysuria | 41 (77,6%) | 58 (66,7%) |
| Nocturia | 13 (23,6%) | 15 (17,2%) |
| Hematuria | 2 (3,6%) | 2 (2,3%) |
| Urinary retention | 18 (32,8%) | 16 (18,4%) |
| Pelvic pain | 5 (5,5%) | 12 (13,8%) |
| Bone pain | 18 (30,9%) | 31 (35,6%) |
| Pain in the lumbar region | 4 (7,5%) | 4 (4,6%) |
| Weakness | 30 (54,5%) | 38 (43,7%) |
The purpose of the study was to evaluate the effectiveness of the drug Buserelin-depot at a dose of 3.75 mg, with a dosage frequency of 1 time in 28 days, by studying the dynamics of testosterone, PSA levels, and prostate volume; to determine the effect of the drug on the activity status of patients and the level of pain and compare it with a group of patients treated with other LHRH analogues, and monitor side effects.
Patients of group 2 received one of the LHRH analogues also once every 28 days. In addition to hormone therapy, patients with bone metastases were treated with other specialized treatment methods: palliative distant therapy for bone metastases, treatment with zoledronic acid.
During histological verification of the diagnosis, moderately and poorly differentiated forms of prostate cancer predominated (Table 3).
Table 3. Histological types of tumors
| Histological tumor type | Buserelin (n=55) | Other LHRH analogues (n=87) | |||
| abs | % | abs | % | ||
| Gleason 2-4 | 7 | 12,7 | 11 | 12,6 | |
| Gleason 5-6 | 15 | 27,3 | 24 | 27,6 | |
| Gleason 7 | 24 | 43,6 | 35 | 40,2 | |
| Gleason 8-10 | 9 | 16,4 | 17 | 19,6 | |
| Total | 55 | 100 | 87 | 100 | |
For patients in both groups, before the start of treatment, PSA and testosterone levels were determined, activity status was assessed according to the Karnofsky scale, pain status according to the WHO scale, and prostate volume was measured using TRUS.
Subsequently, all patients underwent PSA and testosterone monitoring every 4 weeks; after 3 months, a control determination of prostate volume was performed; upon completion of treatment, the activity status and pain status of the patients were re-determined.
All patients had PSA above normal before treatment. The average PSA value in the first group was 107.3 ng/ml, in the second - 97.5 ng/ml. After the start of treatment, most patients had positive PSA dynamics, characterized by a sharp decrease in the first 2 months of treatment, after which gradual regression and stabilization of indicators occurred.
During therapy with Buserelin-depot in patients with prostate cancer, a consistent decrease in average PSA values was revealed from 107.3 ng/ml to 37.8 ng/ml after 2 months, to 27.9 ng/ml after 4 months, to 3.3 ng /ml after 6 months. In the group of patients treated with other LHRH analogues, there was also a regression of the average PSA value: from 97.5 ng/ml to 24.05 ng/ml after 2 months, to 12.35 ng/ml after 4 months, to 3. 1 ng/ml after 6 months.
The dynamics of prostate volume correlated with a decrease in PSA levels. During therapy with Buserelin-depot in patients with prostate cancer, a decrease in the volume of the prostate gland was noted from 55.9 to 39.8 cm3 by 6 months of treatment (-28.8%). The average volume of the prostate gland in patients of group 2 was 63.9 cm3. After 6 months of treatment, the volume of the gland decreased by 33.2% (42.7 cm3). The registered change in the volume of the prostate gland during treatment became a prerequisite for reducing the symptoms of urinary disorders in the vast majority of patients in the study groups.
The average testosterone level in patients of the first group before treatment was 17.7 ng/ml, in the second group the average value was 14.21 ng/ml.
During the therapy, a decrease in testosterone levels to post-castration values was achieved in patients of both groups within a month after the start of hormone therapy. In the first group: from initial 17.7 to 2.12 ng/ml after 2 months and 0.41 ng/ml after 4 months of treatment. In the second group, after 2 months there was a decrease in the average testosterone level from 14.21 to 1.53 ng/ml and to 0.39 ng/ml after 4 months of treatment. After 4 months of treatment, no further significant changes in testosterone levels were observed.
The treatment provided was intermittent. Considering the positive results of 6 months of therapy in the buserelin group and the other LHRH agonists group, further use of the drugs was discontinued with subsequent dynamic monitoring of PSA and testosterone levels.
The dynamics of testosterone levels were monitored in the first and second groups of patients after discontinuation of treatment with LHRH analogues. When analyzing the data obtained, it turned out that an increase in testosterone levels above castration values when using buserelin occurs 1 month after completion of treatment, and in the second group of patients, where other LHRH analogues were used, this was noted after 1.8 months. Further observation showed that the time to restore initial testosterone levels occurred in the buserelin group after 2.4 months, and when using other LHRH analogues after 3.2 months.
In 822 patients before treatment, the activity status on the Karnofsky scale was 80-100%, in 35 – 60-70% and in 25 patients – 50-60% when assessing both groups. It should be noted that patients with generalized forms of prostate cancer had a lower status index. Upon completion of HT, a change in activity status in a positive direction occurred in 5 (9%) patients of group 1 and in 8 (9.2%) in the group of patients receiving therapy with LHRH agonists (Table 4).
Table 4. Activity status of patients in groups before and after treatment
| Activity status according to Karnovsky, % | Buserelin (n=55) | Other LHRH analogues (n=87) | |||||||
| before treatment | after treatment | before treatment | after treatment | ||||||
| abs | % | abs | % | abs | % | abs | % | ||
| 80-100 | 31 | 56,4 | 35 | 63,6 | 51 | 58,6 | 55 | 63,2 | |
| 60-70 | 15 | 27,3 | 12 | 21.8 | 20 | 23 | 20 | 23 | |
| 50-60 | 9 | 16,4 | 8 | 14,5 | 16 | 18,4 | 12 | 13,8 | |
Before the prescription of hormonal therapy, 66 patients (46.5%) had pain syndrome. 76 patients did not require pain relief. 22 (15.5%) patients took non-narcotic analgesics irregularly, 16 (11.3%) patients required inconsistent use of narcotic analgesics to reduce pain, and 28 (19.7%) patients constantly took non-narcotic analgesics. After 6 months of drug use, the number of patients who did not require analgesics in both groups increased by 5.8%. At the same time, none of the patients was able to completely abandon the use of analgesic drugs (Table 5).
Table 5. Dynamics of pain status of patients in groups according to the WHO scale.
| Pain gradation (WHO), points | Buserelin (n=55) | Other LHRH analogues (n=87) | |||||||
| before treatment | after treatment | before treatment | after treatment | ||||||
| abs | % | abs | % | abs | % | abs | % | ||
| 0-no analgesics required | 32 | 58 | 33 | 60 | 44 | 50,6 | 46 | 52,9 | |
| 1-sometimes non-narcotic | 7 | 12,7 | 8 | 14,5 | 15 | 17,2 | 16 | 18,4 | |
| 2-regularly non-narcotic | 11 | 20 | 12 | 21,8 | 17 | 19,5 | 18 | 20,7 | |
| 3-sometimes narcotic | 5 | 9,3 | 2 | 3,7 | 11 | 12,7 | 7 | 8 | |
| 4-regularly narcotic | — | — | — | — | — | — | — | — | |
When using Buserelin-depot, the vast majority of patients complained of hot flashes and sweating, which was also noted by patients treated with other LHRH agonists. There were no cases of urinary retention, muscle weakness in the lower extremities, edema or lymphostasis. It should be noted that most side effects are completely reversible after discontinuation of the drugs.
Experience with the use of Beserelin Depot has shown that it is highly effective for the treatment of hormone-dependent prostate cancer. The use of Buserelin-depot leads to a decrease in PSA levels, ensures a stable decrease in serum testosterone levels to the post-castration level, a decrease in the volume of the prostate gland and a decrease in symptoms of urinary disorders in the absence of serious side problems. A number of patients showed an increase in activity status, as well as a decrease in the need and dose of analgesics.
An earlier restoration of the initial testosterone level was noted after completion of the course of Buserelin-depot compared to other LHRH analogues, which reduces the severity of side effects of HT and improves the quality of life of patients.
Buserelin depot can be recommended for use as independent therapy or in combination with other hormonal drugs in patients with prostate cancer.
Bibliography
- Huggins C., Hodges CV Studies on prostatic cancer. II The effect of castration, estrogen and androgen injections on serum. Cancer Res 1944;1:293–297.
- Oefelein MG, Feng A, Scolieri MJ, et al. Reassessment of the definition of castrate levels of testosterone: implications for clinical decision making. Urology 2000;56:1021-4.
- Evans CP, Fleshner N, Fitzpatrick JM, et al. An evidence-base approach to understanding the pharmacological class effect in the management of prostatic diseases. BJU Int 2005;95:742-9.
- Seidenfeld J., Samson DJ, Hasselblad V. et al. Single-therapy androgen suppression in men with advanced prostate cancer: a systematic review and meta-analysis. Annals of Internal Medicine, 2000, v. 132, issue 7, p. 566-577.
- Anderson J, Abrahamsson PA, Crawford D, et al. Management of advanced prostate cancer: can we improve on androgen deprivation therapy. BJU Int 2008;101:1497-1501.
- Heidenreich A, Pfister D, Ohlamann CH, et al. Androgen deprivation for advanced prostate cancer. Urologe 2008;47:270-83.
- Klioze SS, Miller MF, Spiro TP. A randomized, comparative study of buserelin with DES/ orchiectomy in the treatment of stage D2 prostatic cancer patients. Am J Clin Oncol 1988;11(Suppl 2):S17-S182
- Huben RP, Murphy GP. A comparison of diethylstilbestrol or orchiectomy with buserelin and with methotrexate plus diethylbestrol or orchiectomy in newly diagnosed patients with clinical stage D2 cancer of the prostate. Cancer 1988; 62:1881-7.
- Bruun E, Frimodt-Moller C. The effect of buserelin versus conventional antiandrogenic treatment in patients with T2-4NXM1 prostatic cancer. A prospective, randomized multicentre phase III trial. The “Danish Buserelin Study Group”. Scand J Urol Nephrol 1996;30:291-7.
Contraindications:
- Allergic reaction to buserelin acetate or additional substances;
- Pregnancy and lactation;
- Kidney failure;
- Depression;
- Diabetes mellitus along with two or more complications.
Side effects of Buserelin
It is worth noting that “Buserelin” for fibroids and other diseases has a number of side effects:
- From the gastrointestinal tract: thirst, nausea and vomiting, weight gain or loss;
- From the central nervous system: headaches and dizziness, insomnia, constant feeling of weakness and fatigue, depression, anxiety;
- From the cardiovascular system: strong heartbeats, increased blood pressure;
- From the senses: visual impairment, hearing impairment, tinnitus;
- From the endocrine system: hot flashes, severe sweating, decreased libido, pain in the lower abdomen;
- Allergic reactions of varying intensity.
The effect of "Buserelin" on the female body
The effect of “Buserelin” for uterine fibroids depends on the type of myomatous nodes and the individual characteristics of the patient’s body. It is worth noting that reviews of taking this drug are not always positive, since it causes a number of side effects. At the same time, it is worth noting that when using Buserelin in the form of a nasal spray. Negative manifestations were practically not noticed. Numerous studies show that after therapy with Buserelin, many women develop early menopause. The drug has found wide use in the postoperative period to eliminate the risk of fibroid recurrence.
In what cases is Mirena prescribed for adenomyosis?
Adenomyosis is a gynecological pathology in which the endometrium grows into the muscular layer of the uterus. The progression of the disease is accompanied by pathological symptoms, disruption of the reproductive system, and the inability to conceive and bear a child. Mirena for uterine adenomyosis helps stop the uncontrolled growth of the endometrium and relieve unpleasant symptoms.
The intrauterine device is installed only according to doctor's indications. The drug is recommended in the following cases:
Progressive internal adenomyosis, manifested by a pronounced clinical picture. A woman is worried about severe pain in the lower abdomen, heavy, prolonged menstrual bleeding, and discomfort during sexual intercourse.
- Uterine leimioma.
- Endometrial hyperplasia.
- Menstrual irregularities.
- Extensive damage by foci of adenomyosis of the myometrium.
- Heavy uterine bleeding, contributing to the development of iron deficiency anemia.
An intrauterine device is installed in women who have already given birth to a child. In exceptional situations, the drug is also used for nulliparous women, but in this case there is a high risk of prolapse of the system from the uterus. Before installation, the doctor sanitizes the vagina and cervix to make sure there are no active inflammatory processes. It is worth noting that after implantation, a woman will not be able to get pregnant for 5 years; this fact is also taken into account by the doctor before prescribing the drug.
Mode of application
Side effects can be minimized and positive results can be achieved from taking Buserelin by strictly following the dosage and dosage regimen recommended by your doctor. They directly depend on the form of release of the drug. Thus, a nasal spray is usually used three times a day at equal intervals at a rate of 0.9 mg per day. During treatment, oral contraceptives cannot be used, so it is recommended to replace them with other methods of contraception. Intramuscular injections of Buserelin are given every 28 days, starting 5 days before the start of the cycle. If the product is used as preoperative preparation, then injections are given within three months. As for conservative therapy, its course lasts six months.
Disadvantages of the IUD
Like any other medication, the Mirena therapeutic system has its drawbacks, among which the most significant are:
- Installation and removal is carried out only by a doctor.
- Not suitable for women who are planning pregnancy in the near future.
- Has an abortifacient effect. The IUD does not always suppress ovulation, so conceiving a child is possible. But the pregnancy is terminated not yet in the early stages, since the implantation process is disrupted and a miscarriage occurs.
- Long adaptation period. In the first 3 to 6 months after IUD implantation, you may experience intermenstrual bleeding, which is normal.
- When installing an IUD, the risk of infection entering the uterine body increases.
- It is rare, but it happens that the drug leads to the progression of an aseptic inflammatory process in the reproductive organ.