Pharmacological properties of the drug Naropin
Pharmacodynamics. Naropin contains ropivacaine, a pure enantiomer, which is an amide-type local anesthetic. Ropivacaine reversibly blocks the conduction of impulses along nerve fibers, suppressing the transport of sodium ions across the membranes of nerve cells. Similar effects are observed when the membranes of brain and myocardial cells are excited. Ropivacaine has an anesthetic and analgesic effect. When using the drug in high doses, surgical anesthesia is achieved, in low doses - sensory blockade (analgesia) and non-progressive motor blockade. The duration and intensity of blockade by ropivacaine is not potentiated when combined with epinephrine. Ropivacaine in vitro showed a less negative isotropic effect than levobupivacaine and bupivacaine. Determination of the effect on cardiac activity carried out in vivo in animal studies showed that ropivacaine has lower toxicity than bupivacaine. This difference was both qualitative and quantitative. The use of ropivacaine in standard doses causes less widening of the QRS than bipuvacaine, however, taking ropivacaine and levobupivacaine in high doses has a greater effect on the widening of the complex than bupivacaine at the same doses. Direct cardiovascular effects of local anesthetics include conduction slowing, negative inotropism, arrhythmia, and even cardiac arrest. After administration of ropivacaine, dogs receiving IV doses until the onset of signs of acute cardiovascular failure were more easily resuscitated than after administration of levobupivacaine and bupivacaine, despite higher free plasma concentrations. This indicates a wider margin of safety for the use of ropivacaine in the event of accidental IV injection or overdose. Pregnant sheep were not observed to be more susceptible to the systemic toxic effects of ropivacaine than non-pregnant sheep. After the use of ropivacaine in healthy volunteers receiving intravenous infusion, a significantly lower potential for toxicity from the central nervous system and the cardiovascular system was revealed than after the use of bupivacaine. CNS symptoms with these drugs are similar, but with bupivacaine they occur at lower doses and plasma concentrations, and also have a longer duration. Indirect cardiovascular effects (hypotension, bradycardia) may develop after epidural blockade, depending on the degree of concomitant sympathetic blockade. When a large amount of the drug enters the circulatory system, symptoms from the central nervous system and cardiovascular system quickly develop. Pharmacokinetics. The pKa value of ropivacaine is 8.1 and the partition coefficient is 141 (25 °C n-octanol/phosphate buffer at pH 7.4). Absorption. The concentration of ropivacaine in blood plasma depends on the administered dose, route of administration and perfusion at the injection site. Ropivacaine exhibits linear pharmacokinetics and peak plasma concentrations are dose proportional. Ropivacaine exhibits complete and biphasic absorption from the epidural space, with the elimination half-life of the two phases being approximately 14 minutes and 4 hours, respectively. Slow absorption is a factor that limits the rate of elimination of ropivacaine and explains why the half-life after epidural administration is longer than after IV administration. Distribution. Ropivacaine binds in blood plasma predominantly to acidic α1-glycoproteins, the unbound fraction is about 6%. The volume of distribution at steady state is 47 liters. An increase in total plasma concentrations of ropivacaine and hypocolylxylidine (PPX) with epidural infusion was observed, which was dependent on the postoperative increase in α1-acid glycoproteins. The increase in plasma concentrations of unbound, pharmacologically active ropivacaine was significantly less than the increase in total ropivacaine concentrations. The mean concentration of unbound PPX was approximately 7-9 times higher than the mean concentration of unbound ropivacaine after epidural infusion up to and including 72 hours. Metabolism. Ropivacaine is metabolized in the liver primarily by aromatic hydroxylation to hydroxyropivacaine by cytochrome P450 1A2 and by N-dealkylation to PPX by CYP 3A4. PPX is the active metabolite. The threshold for CNS toxicity in plasma concentrations of unbound PPX in rats was approximately 12 times higher than the threshold for unbound ropivacaine. PPX is a metabolite of minor significance after single doses, but is the major metabolite after continuous epidural infusion. Excretion. Metabolites are excreted in the urine. About 1% of a single dose of ropivacaine is excreted unchanged. The total plasma clearance of ropivacaine is approximately 440 ml/min, the clearance of unbound ropivacaine is 8 L/min, and the renal clearance is 1 ml/min. The half-life is 1.8 hours. The intermediate hepatic extraction coefficient is 0.4. Children. Based on research results, it has been established that in children aged 1 to 12 years, the pharmacokinetics of ropivacaine does not depend on age. In this group, the total plasma clearance of ropivacaine is 7.5 ml/min/kg, the plasma clearance of unbound ropivacaine is 0.15 l/min/kg. The volume of distribution at steady state is 2.4 l/kg, the unbound fraction of ropivacaine is 5%, and the half-life is 3 hours. Ropivacaine exhibits biphasic absorption in the caudal space. Clearance is related to body weight and is similar to clearance in adults.
Naropin, 5 pcs., 10 ml, 7.5 mg/ml, solution for injection
Naropin® should only be used by or under the supervision of specialists with sufficient experience in performing regional anesthesia.
Adults and children over 12 years old
:
In general, anesthesia for surgical interventions requires higher doses and more concentrated solutions of the drug than when using an anesthetic for pain relief. When using an anesthetic for pain relief, a dose of 2 mg/ml is usually recommended. For intra-articular administration, a dose of 7.5 mg/ml is recommended.
The doses indicated in Table 1 are considered sufficient to achieve a reliable blockade and are indicative when using the drug in adults, because There is individual variability in the speed of development of the blockade and its duration.
The data in Table 1 is an indicative guide to the dosage of the drug for the most commonly used blockades. When selecting the dose of the drug, it should be based on clinical experience taking into account the physical condition of the patient.
Table 1
Dosing recommendations for Naropin® for adults
| Types of anesthesia | Drug concentration, mg/ml | Volume of solution, ml | Dose, mg | Onset of action, min | Duration of action, h |
| Anesthesia for surgical interventions: | |||||
| Lumbar epidural anesthesia: | |||||
| Surgical interventions | 7,5 | 15–25 | 113–188 | 10–20 | 3–5 |
| 10 | 15–20 | 150–200 | 10–20 | 4–6 | |
| C-section | 7,5 | 15–20 | 113–150 | 10–20 | 3–5 |
| Epidural anesthesia at the thoracic level: | |||||
| Postoperative analgesic blockade and surgical interventions | 7,5 | 5–15 | 38–113 | 10–20 | — |
| Blockade of large nerve plexuses: | |||||
| For example, brachial plexus block | 7,5 | 10–40 | 75–300* | 10–25 | 6–10 |
| Conduction and infiltration anesthesia | 7,5 | 1–30 | 7,5–225 | 1–15 | 2–6 |
| Relief of acute pain syndrome: | |||||
| Epidural injection at the lumbar level: | |||||
| Bolus | 2 | 10–20 | 20–40 | 10–15 | 0,5–1,5 |
| Periodic administration (for example, for pain relief during labor) | 2 | 10–15 (minimum interval - 30 minutes) | 20–30 | ||
| Extended infusion for: | |||||
| - labor pain relief | 2 | 6–10 ml/h | 12–20 mg/h | — | — |
| - after surgical anesthesia | 2 | 6–14 ml/h | 12–28 mg/h | — | — |
| Peripheral nerve block: | |||||
| For example, femoral nerve block or interscalene block (extended infusions or repeated injections) | 2 | 5–10 ml/h | 10–20 mg/h | — | — |
| Epidural injection at the thoracic level: | |||||
| Extended infusion (eg, for postoperative pain relief) | 2 | 6–14 ml/h | 12–28 mg/h | — | — |
| Conductor blockade and infiltration anesthesia | 2 | 1–100 | 2–200 | 1–5 | 2–6 |
| Intra-articular injection | |||||
| Knee arthroscopy** | 7,5 | 20 | 150*** | — | 2–6 |
* The dose for major plexus block should be adjusted according to the site of administration and the patient's condition. Brachial plexus blocks using the interscalene and supraclavicular approaches may be associated with a high incidence of serious adverse reactions, regardless of the local anesthetic used.
** Cases of chondrolysis have been reported with postoperative extended intra-articular infusion of local anesthetics. Naropin® should not be used for prolonged intra-articular infusion.
*** If Naropin® was additionally used for other types of anesthesia, the maximum dose should not exceed 225 mg.
Standard guidelines should be used to understand the factors influencing the method of performing individual blocks and the requirements for specific patient groups.
To prevent the anesthetic from entering the vessel, an aspiration test must be performed before and during the administration of the drug. If the drug is intended to be used in a high dose, it is recommended to administer a test dose of 3–5 ml of lidocaine with epinephrine. Accidental intravascular injection is recognized by a temporary increase in heart rate, and accidental intrathecal injection is recognized by signs of spinal block. If toxic symptoms appear, you should immediately stop administering the drug.
Before and during the administration of Naropin® (which should be done slowly or by increasing sequential doses of the drug at a rate of 25-50 mg/min), the patient's vital signs should be carefully monitored and verbal contact should be maintained.
A single dose of ropivacaine up to 250 mg for epidural blockade for surgical intervention is usually well tolerated by patients.
When brachial plexus block is administered with 40 ml of Naropin® 7.5 mg/ml, maximum plasma concentrations of ropivacaine in some patients may reach values characterized by mild symptoms of CNS toxicity. Therefore, the use of a dose higher than 40 ml of Naropin® 7.5 mg/ml (300 mg ropivacaine) is not recommended.
When carrying out a long-term blockade by prolonged infusion or repeated bolus administration, the possibility of creating toxic concentrations of anesthetic in the blood and local nerve damage should be taken into account. The administration of ropivacaine over 24 hours at a dose of up to 800 mg in total during surgical interventions and for postoperative pain relief, as well as prolonged epidural infusion after surgery at a rate of up to 28 mg/h for 72 hours, is well tolerated by adult patients.
To relieve postoperative pain, the following regimen of drug use is recommended: if an epidural catheter was not installed during surgery, after its installation, an epidural blockade is performed with a bolus injection of the drug Naropin® (7.5 mg/ml). Analgesia is maintained by infusion of Naropin® (2 mg/ml). In most cases, for the management of moderate to severe postoperative pain, infusion at a rate of 6-14 ml/h (12-28 mg/h) provides adequate analgesia with minimal non-progressive motor blockade (a significant reduction in the need for opioid analgesics has been observed using this technique ).
For postoperative pain relief, Naropin® (2 mg/ml) can be administered continuously as an epidural infusion for 72 hours without or in combination with fentanyl (1–4 μg/ml). Naropin® 2 mg/ml (6–14 ml/h) provided adequate pain relief in most patients. The combination of Naropin® and fentanyl led to improved pain relief, while causing side effects typical of narcotic analgesics.
The use of Naropin® at concentrations above 7.5 mg/ml during cesarean section has not been studied.
table 2
Recommendations for dosing of Naropin® for children under 12 years of age
| Indicators | Drug concentration, mg/ml | Volume of solution, ml/kg | Dose, mg/kg |
| Relief of acute pain syndrome (pre- and postoperative): | |||
| Caudal epidural insertion: | |||
| Blockade in the area below ThXII in children weighing up to 25 kg | 2 | 1 | 2 |
| Extended epidural infusion in children weighing up to 25 kg | |||
| Age from 0 to 6 months | |||
| Bolus* | 2 | 0,5–1 | 1–2 |
| Infusion up to 72 hours | 2 | 0.1 ml/kg/h | 0.2 mg/kg/h |
| Age from 6 to 12 months | |||
| Bolus* | 2 | 0,5–1 | 1–2 |
| Infusion up to 72 hours | 2 | 0.2 ml/kg/h | 0.4 mg/kg/h |
| Age from 1 to 12 years inclusive | |||
| Bolus** | 2 | 1 | |
| Infusion up to 72 hours | 2 | 0.2 ml/kg/h | 0.4 mg/kg/h |
* Lower doses of the suggested range are recommended for thoracic epidural administration, while higher doses are recommended for lumbar or caudal epidural administration.
** Recommended for epidural administration at the lumbar level. It is reasonable to reduce the bolus dose for epidural analgesia at the thoracic level.
The doses indicated in Table 2 are a guide to the use of the drug in pediatric practice. At the same time, there is individual variability in the speed of development of the block and its duration.
In overweight children, a gradual reduction in the dose of the drug is often required; In this case, it is necessary to be guided by the patient’s ideal body weight. Specific guidelines should be consulted for background information on the factors that influence individual block techniques and the requirements for specific patient groups. The caudal epidural solution volume and epidural bolus volume should not exceed 25 mL for any patient.
To prevent inadvertent intravascular injection of anesthetic, careful aspiration testing should be performed before and during administration of the drug. During administration of the drug, it is necessary to carefully monitor the patient's vital functions. If toxic symptoms appear, you should immediately stop administering the drug.
A single dose of ropivacaine 2 mg/ml (at a rate of 2 mg/kg, solution volume 1 ml/kg) for postoperative caudal analgesia provides adequate pain relief below the ThXII level in most patients. Children over 4 years of age tolerate doses up to 3 mg/kg. The volume of epidural solution administered at the caudal level can be varied to achieve varying degrees of sensory block, as described in specialized guidelines.
Regardless of the type of anesthesia, bolus administration of the calculated dose of the drug is recommended.
The use of the drug in concentrations higher than 5 mg/ml, as well as the intrathecal use of Naropin® in children, have not been studied. The use of Naropin® in premature infants has not been studied.
Instructions for using the solution
The solution does not contain preservatives and is intended for single use only. Any amount of solution remaining in the container after use must be destroyed.
An unopened container of solution should not be autoclaved.
Unopened blister packs provide sterility to the outer surface of the container and are preferred for use in environments requiring sterility.
Indications for use of the drug Naropin
Anesthesia for surgical interventions:
- epidural anesthesia for surgical interventions, including caesarean section;
- nerve plexus blockade;
- peripheral nerve block and infiltration anesthesia.
Relief of acute pain:
- continuous epidural infusion or periodic bolus injections to relieve postoperative pain or labor pain;
- peripheral nerve block and infiltration anesthesia;
- intra-articular injections;
- Long-term blockade of peripheral nerves by infusion or periodic injections, for example to eliminate post-operative pain.
Relief of acute pain in children (during and after surgery):
- caudal block to relieve pain in newborns, infants and children up to 12 years of age inclusive;
- continuous epidural infusion in newborns, infants and children up to and including 12 years of age.
Use of the drug Naropin
Naropin is administered only by a doctor with experience in regional anesthesia or the administration is carried out under his supervision. To achieve adequate anesthesia, the drug should be used in the lowest doses. Adults and children over 12 years of age. Below are the recommended doses; dosage must be adjusted depending on the degree of blockade and the general condition of the patient. Anesthesia for surgical interventions requires the use of the drug in a high dose and a higher concentration than anesthesia for the purpose of relieving acute pain, which usually requires a concentration of 2 mg/ml. For intra-articular injections, a concentration of 7.5 mg/ml is recommended.
Drug concentration (mg/ml) | Dose | Dose | Onset of action (min) | Duration of action (hours) | |
| Anesthesia for surgical interventions | |||||
| Lumbar epidural injection for surgery | 7,5 10 | 15–25 ml 15–20 ml | 113–188 mg 150–200 mg | 10–20 10–20 | 3–5 4–6 |
| Lumbar epidural injection for caesarean section | 7,5 | 15–20 ml | 113–150 mg | 10–20 | 3–5 |
| Thoracic epidural injection for postoperative analgesic block | 7,5 | 5–15 ml depending on injection level | 38–113 mg | 10–20 | – |
| Peripheral nerve block and infiltration anesthesia | |||||
| Brachial plexus block | 7,5 | 30–40 ml | 225–300 mg1 | 10–25 | 6–10 |
| Small and medium nerve block and infiltration anesthesia | 7,5 | 1–30 ml | 7.5–225 mg | 1–15 | 2–6 |
| Relief of acute pain | |||||
| Lumbar epidural injection | |||||
| Bolus | 2 | 10–20 ml | 20–40 mg | 10–15 | 0,5–1,5 |
| Periodic injections (extra doses), for example for pain relief during childbirth | 2 | 10–15 ml at intervals of at least 30 minutes | 20–30 mg | – | – |
| Lumbar epidural insertion at the lumbar level | |||||
| Long-term infusion, for example for post-operative or labor pain relief | 2 | 6–14 ml/h | 12–28 mg/h | – | – |
| Thoracic epidural insertion | |||||
| Long-term infusion, for example for post-operative pain relief | 2 | 6–14 ml/h | 12–28 mg/h | – | – |
| Peripheral nerve block and infiltration anesthesia | 2 | 1–100 ml | 2–200 mg | 1–5 | 2–6 |
| Intra-articular injection (for example, for knee arthroscopy) | 7,5 | 20 ml | 150 mg2 | – | 2–6 |
| Peripheral nerve blocks (femoral or interscalene blocks) Continuous infusion or intermittent injections (eg for post-operative pain relief) | 2 | 5–10 ml/h | 10–20 mg/h | – | – |
The doses given in the table are those required to provide clinically acceptable blockade and should be considered as recommended for adults.
There is considerable individual variation regarding the time of onset and duration of effect. 1The dose for plexus block should be adjusted depending on the site of administration and the patient's condition. With interscalene and supraclavicular brachial plexus blocks, an increased incidence of severe adverse reactions may be observed, regardless of the local anesthetic used. 2When administering an additional dose of ropivacaine by any other technique to the same patient, the total dose limit should not exceed 225 mg. It is important to take special care to prevent accidental intravascular injections. Careful aspiration testing is recommended before and during injection of the total dose. The total dose should be administered slowly at a rate of 25-50 mg/min or in separate doses, constantly monitoring the patient's condition. When administering high-dose epidural injections, it is recommended to administer a test dose of 3–5 ml of xylocaine epinephrine. Accidental intravascular administration may cause, for example, a transient increase in heart rate, and accidental intrathecal administration may cause spinal block. If symptoms of intoxication occur, administration of the drug should be stopped immediately. When blocking the brachial plexus by administering 40 ml of Naropin at a concentration of 7.5 mg/ml, the maximum concentration of ropivacaine in the blood plasma in some patients may approach the level at which mild symptoms of toxic effects on the central nervous system were described. Therefore, it is not recommended to use doses exceeding 40 ml of Naropin with a concentration of 7.5 mg/ml (300 mg of ropivacaine). When administering a continuous infusion or repeated bolus injections, the risk of toxic plasma concentrations or local nerve damage should be considered. Total doses of ropivacaine up to 800 mg inclusive, administered over 24 hours, were well tolerated by adult patients during anesthesia for surgical interventions and for the relief of postoperative pain. Good tolerability was observed in adults with continuous epidural infusions, which were carried out after surgery for 72 hours at an infusion rate of up to 28 mg/h. Relief of postoperative pain: the blockade is carried out before surgery by administering Naropin 10 or 7.5 mg/ml or after surgery by epidural bolus administration of Naropin 7.5 mg/ml. Analgesia is maintained with an epidural infusion of Naropin 2 mg/ml. Clinical studies have demonstrated that infusion rates of 6–14 mL (12–28 mg/h) provide satisfactory anesthesia for moderate to severe postoperative pain, with most cases showing only mild and nonprogressive motor block. This technique can significantly reduce the need for additional use of opioid analgesics. Clinical studies were also conducted in which epidural infusion of Naropin alone or Naropin in combination with fentanyl (1–4 μg/ml) for 72 hours was used for postoperative pain relief. When using Naropin 2 mg/ml (6–14 mg/h) was observed effective pain relief in most patients. The combination of Naropin and fentanyl provided better pain relief, but caused opioid side effects. For caesarean sections, epidural ropivacaine 7.5 mg/ml or spinal administration was not performed. When performing long-term peripheral nerve blockade by continuous infusion or repeated injections, the risk of toxic plasma drug concentrations or local damage must be taken into account. In clinical studies, femoral nerve block before surgery was achieved by administering 300 mg of Naropin at a concentration of 7.5 mg/ml, and an interscalene block with 225 mg of Naropin at a concentration of 7.5 mg/ml. Analgesia was then maintained by administering Naropin 2 mg/ml. The infusion rate or periodic injections of 10–20 mg/h over 48 hours provided sufficient analgesia and good tolerability. Children under 12 years of age
Concentration | Volume | Dose | |
| Relief of acute pain before and after surgery | |||
| Single caudal block in children under 12 years of age For distribution below the T12 level Children weighing up to 25 kg inclusive | 2 mg/ml | 1 ml/kg | 2 mg/kg |
| Continuous epidural infusion in children weighing up to 25 kg inclusive | |||
| 0–6 months Bolus Infusion up to 72 hours | 2 mg/ml 2 mg/ml | 0.5–1 ml/kg 0.1 mg/kg/h | 1–2 mg/kg 0.2 mg/kg/h |
| 6–12 months Bolus Infusion up to 72 hours | 2 mg/ml 2 mg/ml | 0.5–1 ml/kg 0.2 mg/kg/h | 1–2 mg/kg 0.4 mg/kg/h |
| 1 year–12 years Bolus Infusion up to 72 hours | 2 mg/ml 2 mg/ml | 1 ml/kg 0.2 mg/kg/h | 2 mg/kg 0.4 mg/kg/h |
a) For thoracic epidural blocks, doses at the lower end of the dosing range are recommended, while for lumbar or caudal epidural blocks, the upper end of the dosing range is recommended. b) Recommended for lumbar epidural blocks.
When used in children, the doses given in the table should be considered as recommended. The dose should be selected individually. Overweight children often require a gradual dose reduction, which is calculated based on proper body weight. Specific Dosing Recommendations The volume of caudal epidural injection is adjusted until the spread of sensory blockade is controlled. There is experience with the safe use of doses up to 3 mg/kg inclusive. Experience with caudal blocks in children weighing 25 kg is limited. When using a calculated dose, it is recommended to fractionate the total dose.
Instructions for use NAROPIN® 200 mg/100 ml
The drug is used for epidural, infiltration and conduction anesthesia. Naropin should only be used by or under the supervision of specialists with sufficient experience in performing regional anesthesia.
Naropin is administered slowly or by increasing sequentially administered doses of the drug at a rate of 25-50 mg/min.
To prevent the anesthetic from entering the vessel, an aspiration test must be performed. If you intend to use the drug in a high dose, it is recommended to administer a test dose - 3-5 ml of lidocaine with epinephrine. Accidental intravascular injection is recognized by a temporary increase in heart rate, and accidental intrathecal injection is recognized by signs of spinal block. In general, higher doses and more concentrated solutions of the drug are required for anesthesia during surgical procedures (for example, with epidural administration). For pain relief (for example, epidural administration to relieve pain), lower doses and concentrations of the drug are recommended. The table provided is a rough guide to the dosage of the drug for the most commonly used blockades. When selecting the dose of the drug, it should be based on clinical experience taking into account the physical status of the patient.
| Drug concentration (mg/ml) | Volume of solution (ml) | Dose (mg) | Onset of action (min) | Duration of action (hours) | |
| Relief of acute pain syndrome: | |||||
| Epidural injection at the lumbar level: | |||||
| Bolus | 2.0 | 10-20 | 20-40 | 10-15 | 0.5-1.5 |
| Periodic administration (for example, for pain relief during labor) | 2.0 | 10-15 (minimum interval - 30 minutes) | 20-30 | — | — |
| Extended infusion for - labor pain relief - post-operative pain relief | 2.0 2.0 | 6-10 ml/h 6-14 ml/h | 12-20 mg/h 12-28 mg/h | — — | — — |
| Epidural injection at the thoracic level: | |||||
| Extended infusion (eg, for postoperative pain relief) | 2.0 | 6-14 ml/h | 12-28 mg/h | — | — |
| Conductive blockade and infiltration | 2.0 | 1-100 | 2-200 | 1-5 | 2-6 |
The doses indicated in the table are considered sufficient to achieve a reliable blockade and are indicative when using the drug in adults, since there is individual variability in the rate of development of the block and its duration. Standard guidelines should be used to understand the factors influencing the method of performing individual blocks and the requirements for specific patient groups.
To relieve postoperative pain, the following regimen of drug use is recommended:
- if the epidural catheter was not installed during surgery, then after its installation an epidural blockade with Naropin (7.5 mg/ml) is performed. Analgesia is maintained by infusion of Naropin (2 mg/ml). In most cases, for the management of moderate to severe postoperative pain, infusion at a rate of 6-14 ml/hour (12-28 mg/hour) provides adequate analgesia with minimal non-progressive motor blockade (a significant reduction in the need for opioid analgesics was observed with this technique).
For postoperative pain relief, Naropin (2 mg/ml) can be administered continuously as an epidural infusion for 72 hours without or mixed with fentanyl (1-4 μg/ml). The use of Naropin in concentrations above 7.5 mg/ml during cesarean section has not been studied.
Instructions for using the solution
The solution does not contain preservatives and is intended for single use only. Any amount of solution remaining in the container after use must be destroyed.
An unopened container of solution should not be autoclaved.
Unopened blister packs provide a sterile exterior of the infusion container and are preferred for use in environments requiring sterility.
Due to the lack of sufficient clinical observations, it is not recommended to use Naropin in children under 12 years of age.
Side effects of the drug Naropin
In clinical studies, a large number of symptoms were reported that represented the physiological effects of the blockade and the clinical situation. Physiological effects of nerve blocks can occur with all types of local anesthetics and include hypotension and bradycardia during epidural and intrathecal anesthesia, as well as events caused directly by spinal puncture (spinal hematoma, headache after dural puncture, meningitis and epidural abscess). Side effects (occur with all types of blockades). Very common (1/10) General: nausea. From the circulatory system: hypotension***. Common (1/100) General: fever, chills, back pain. From the circulatory system: bradycardia*, tachycardia, hypertension. From the side of the central nervous system: paresthesia, dizziness, headache*. From the gastrointestinal tract: vomiting****. From the genitourinary system: urinary retention*. Sometimes (1/1000) General: hypothermia*. From the circulatory system: syncope*. From the central nervous system: anxiety, symptoms of intoxication from the central nervous system (convulsions, grand mal seizure, slight dizziness, perioral paresthesia, numbness of the tongue, hyperacusis, tinnitus, blurred vision, dysarthria, muscle twitching, tremor)**, hypoesthesia*. From the respiratory system: shortness of breath*. Rarely (≤1/1000) General: allergic reactions, in severe cases - anaphylactic shock. From the circulatory system: cardiac arrest, arrhythmias. *Reactions are more likely to occur after spinal anesthesia. **Symptoms occur due to accidental intravascular injection, overdose or rapid absorption. ***Hypotension is rare in children (1/100). ****Vomiting occurs very often in children (1/10). Adverse reactions are grouped by class. The following adverse reactions include complications associated with the anesthesia technique, regardless of the type of local anesthetic used. Neurological complications Neuropathies and spinal cord dysfunction (anterior spinal artery syndrome, arachnoiditis, cauda equina syndrome) have been associated with spinal and epidural anesthesia. Total spinal block Total spinal block occurs when an epidural dose is inadvertently administered intrathecally or when a very high spinal dose is administered. Systemic overdose and accidental intravascular injection can cause serious side effects.
Special instructions for the use of the drug Naropin
Before starting treatment, it is necessary to conduct an individual sensitivity test. The procedure for using regional anesthetics should always be carried out in the presence of prepared equipment for carrying out emergency resuscitation measures. Before the blockade is performed, intravenous catheters are installed in the patient. The physician administering the block must take appropriate precautions to avoid intravascular injections and must be appropriately trained and familiar with the patient's diagnosis and management of side effects, systemic toxicity, and other complications. Large peripheral nerve blocks may require the use of large volumes of local anesthetic in highly vascularized areas that often conceal large vessels where there is a high risk of intravascular injection and/or systemic absorption, which can result in high plasma drug concentrations. Certain procedures with local anesthetics, such as injections into the head and neck areas, may be associated with a high incidence of severe adverse reactions. The blockade should be carried out with caution if patients have II-III degree AV blockade. Elderly persons and patients with progressive liver disease, severe renal impairment or poor general condition should be closely monitored. Patients taking class III antiarrhythmic drugs (eg amiodarone) should also be monitored. In addition, the need for ECG monitoring in such patients should be considered due to the possibility of additive cardiac effects. There are reports of cases of cardiac arrest during the use of Naropin for epidural anesthesia or peripheral nerve blockade, especially after accidental intravascular administration in elderly patients and with concomitant cardiac disease. Ropivacaine is metabolized in the liver. Clinical and pharmacokinetic studies have not been conducted in patients with severe liver disease. There is no need to change the dose for patients with impaired renal function if the drug is used for a single dose or short-term treatment. Acidosis and decreased plasma protein concentrations, which are often observed in patients with chronic renal failure, may increase the risk of systemic toxicity. This risk is also taken into account in malnourished patients and in those treated for hypovolemic shock. Epidural and spinal anesthesia can lead to hypotension and bradycardia. The risk of these effects can be reduced by IV fluids or injection of a vasopressor, such as ephedrine 5–10 mg IV, repeated if necessary. When administering Naropin intra-articularly, caution should be exercised if there is a suspicion of recent extensive intra-articular trauma or if there are large open surfaces in the joint formed during surgery, as this may accelerate absorption and lead to an increase in the concentration of the drug in the blood plasma. Long-term use of ropivacaine should be avoided in patients treated with CYP1A2 inhibitors such as fluvoxamine and enoxacin. In case of overdose or accidental intravascular injection, symptoms of intoxication from the central nervous system (convulsions, impaired consciousness) and/or cardiovascular system (arrhythmias, decreased blood pressure, myocardial depression) may occur. Impact on the ability to drive vehicles or operate other machinery. In addition to the immediate anesthetic effect, ropivacaine has a slight temporary effect on motor activity and coordination of movements. During pregnancy and breastfeeding. Clinical experience in pregnant women is limited. Experimental data obtained from animal studies do not indicate an increased risk of adverse effects on the fetus. It is not known whether ropivacaine passes into breast milk. Children. See INDICATIONS and USAGE.
Naropin
Before anesthesia, it is necessary to assess the general and physical condition of the patient to select the optimal dose of the drug.
For adults, the recommended doses for the most common blockades are given in the table. In general, anesthesia for surgical procedures (eg, epidural administration) requires higher doses of the drug and more concentrated solutions; for pain relief (for example, epidural administration to relieve acute pain), it is recommended to use lower doses and concentrations of the drug.
Anesthesia for surgical interventions
| Drug concentration (mg/ml) | Volume of solution (ml) | Dose (mg) | Onset of action (min) | Duration of action (hours) |
| Lumbar epidural anesthesia: | ||||
| surgical interventions | ||||
| 7.5 | 15-25 | 113-188 | 10-20 | 3-5 |
| 10 | 15-20 | 150-200 | 10-20 | 4-6 |
| C-section | ||||
| 7.5 | 15-20 | 113-150 | 10-20 | 3-5 |
| Epidural anesthesia at the thoracic level: | ||||
| for example, postoperative analgesic blockade | ||||
| 7.5 | 5-15 | 38-113 | 10-20 | — |
| Blockade of large nerve plexuses: | ||||
| for example, brachial plexus block | ||||
| 7.5 | 10-40 | 75-300 | 10-25 | 6-10 |
| Conduction and infiltration anesthesia: | ||||
| 7.5 | 1-30 | 7.5-225 | 1-15 | 2-6 |
Relief of acute pain syndrome
| Drug concentration (mg/ml) | Volume of solution (ml) | Dose (mg) | Onset of action (min) | Duration of action (hours) |
| Epidural injection at the lumbar level: | ||||
| bolus injection | ||||
| 2.0 | 10-20 | 20-40 | 10-15 | 0.5-1.5 |
| repeated administration (for example, for pain relief during labor), minimum interval - 30 minutes | ||||
| 2.0 | 10-15 | 20-30 | — | — |
| extended infusion for labor pain relief | ||||
| 2.0 | 6-10 ml/h | 12-20 mg/h | — | — |
| extended infusion for postoperative pain relief | ||||
| 2.0 | 6-14 ml/h | 12-28 mg/h | — | — |
| Epidural injection at the thoracic level: | ||||
| extended infusion (eg, for postoperative pain relief) | ||||
| 2.0 | 6-14 ml/h | 12-28 mg/h | — | — |
| Conductive blockade and infiltration: | ||||
| 2.0 | 1-100 | 2-200 | 1-5 | 2-6 |
The doses indicated in the table are considered sufficient to perform a reliable blockade in adults, however, the table data is indicative (since there is individual variability in the rate of development of the block and its duration).
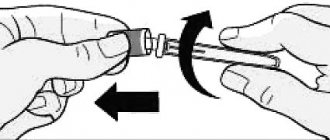
Before and during administration of the drug (which should be done slowly or by increasing sequentially administered doses at a rate of 25-50 mg/min), a careful aspiration test should be performed to prevent the solution from entering the vessel. Accidental intravascular administration is recognized by an increase in heart rate, and accidental intrathecal administration by signs of spinal block. If symptoms of intoxication appear, you should immediately stop administering the drug. For epidural blockade during surgery, a single dose of ropivacaine up to 250 mg is usually well tolerated.
When performing prolonged blockade by prolonged infusion or repeated bolus administration, the possibility of creating toxic concentrations of anesthetic in the blood and local nerve damage should be considered.
A total dose of 800 mg of ropivacaine given over 24 hours, as well as a continuous epidural infusion at a rate of 28 mg/hour for 72 hours, was found to be well tolerated by adults.
To relieve postoperative pain, the following regimen for using the drug is recommended: if an epidural catheter was not installed during surgery, then after its installation, an epidural blockade with Naropin (7.5 mg/ml) is performed. Analgesia is maintained by infusion of Naropin (2 mg/ml). Infusion at a rate of 6-14 ml/h (12-28 mg/h) provides adequate analgesia with mild and non-progressive motor blockade. This technique can significantly reduce the need for opioid analgesics. Clinical studies have shown that for postoperative pain relief, epidural infusion of Naropin (2 mg/ml) without fentanyl or in a mixture with it (1-4 μg/ml) can be carried out continuously for 72 hours. In the latter case, the appearance of effects associated with with stimulation of opioid receptors.
The use of Naropin in concentrations above 7.5 mg/ml during cesarean section is not documented.
Overdose
Symptoms: Accidental intravascular administration of an anesthetic can cause symptoms of intoxication that appear immediately or over a delayed period.
The entry of excess amounts of the drug into the systemic bloodstream has a depressing effect on the central nervous system and myocardium (reduces excitability and automaticity, impairs conductivity).
Neurological manifestations are discrete. First, visual and hearing disturbances, dysarthria, increased muscle tone, and muscle twitching appear. As intoxication progresses, loss of consciousness and attacks of convulsions lasting from several seconds to several minutes are possible, which is accompanied by the rapid development of hypoxia and hypercapnia and respiratory failure, even stopping in severe cases. Respiratory and metabolic acidosis potentiate the toxic effects of the anesthetic.
Subsequently, due to the redistribution of the anesthetic from the central nervous system and its subsequent metabolism and excretion, functional restoration occurs, which can occur quite quickly, unless the drug was administered in a high dose.
Cardiovascular dysfunction in the form of arterial hypotension and arrhythmia usually follows the initial manifestations of neurological disorders, unless the patient is under general anesthesia or has not been premedicated with benzodiazepines or barbiturates.
Treatment: when the first signs of systemic intoxication appear, the drug should be stopped immediately. During seizures, adequate oxygen supply should be maintained using a bag or mask. If after 15-20 seconds the convulsions do not stop, anticonvulsants should be used (IV 100-120 mg of thiopental or 5-10 mg of diazepam; after intubation and the start of mechanical ventilation, suxamethonium can be administered). If the activity of the cardiovascular system is suppressed (arterial hypotension, bradycardia), it is necessary to administer ephedrine intravenously at a dose of 5-10 mg, if necessary, repeat the administration after 2-3 minutes. In the event of cardiac arrest, standard resuscitation measures should be carried out. It is necessary to maintain optimal blood gas composition while simultaneously correcting acidosis.
Drug interactions Naropin
Ropivacaine is used with caution in combination with drugs similar in composition to local anesthetics, namely class IB antiarrhythmic drugs, since their toxic effects are additive. Specific studies of interactions between local anesthetics and class III antiarrhythmic drugs (for example, amiodarone) have not been conducted, however, in this case, caution should be exercised during simultaneous use. In healthy volunteers, the clearance of ropivacaine was reduced by up to 77% when administered concomitantly with fluvoxamine, a potent competitive inhibitor of P450 1A2. CYP 1A2 is involved in the formation of hydroxyropivacaine, the main metabolite. Thus, the simultaneous use of potent CYP1A2 inhibitors, such as fluvoxamine and enoxacin, with Naropin may cause a metabolic interaction, which leads to an increase in the concentration of ropivacaine in the blood plasma.
Naropin overdose, symptoms and treatment
Toxicity Seizures may occur following accidental intravascular injections during plexus or other peripheral blocks. When administered spinally, the potential for systemic toxicity is low. Intrathecal use of the drug in high doses can lead to total spinal blockade. Symptoms Systemic toxic reactions mainly affect the central nervous system and cardiovascular system. Such reactions are caused by high blood concentrations of local anesthetics, which may be due to accidental intravascular injection, overdose, or extremely rapid absorption from highly vascularized sites. CNS symptoms are similar for all amide local anesthetics, whereas cardiac symptoms are more dependent on the drug, both quantitatively and qualitatively. Accidental intravascular injections of local anesthetics can cause immediate (seconds to minutes) systemic toxic reactions. In case of overdose, systemic toxicity appears later (15–60 minutes after injection) due to a slow increase in the concentration of local anesthetic in the blood plasma. On the part of the central nervous system, manifestations of toxicity develop gradually, with increasing severity of symptoms and reactions. The first symptoms usually appear in the form of mild dizziness, perioral paresthesia, numbness of the tongue, hyperacusis, tinnitus and blurred vision. Dysarthria, muscle cramps and/or tremors are serious symptoms that occur before the onset of generalized seizures. These signs should not be mistaken for neurotic behavior. After this, loss of consciousness and a grand mal seizure may occur, which last from a few seconds to several minutes. During seizures, oxygen deficiency and hypercapnia quickly develop due to increased muscle activity and insufficient gas exchange in the lungs. In severe cases, respiratory arrest may also occur. Acidosis enhances the toxic effects of local anesthetics. Recovery depends on the metabolism of the local anesthetic and its distribution beyond the CNS. This happens quickly unless a very large amount of the drug is administered. Cardiovascular effects are a more serious concern and are usually preceded by signs of CNS toxicity unless general anesthesia is administered or the patient is placed under deep sedation with agents such as benzodiazipines or barbiturates. As a result of high systemic concentrations of local anesthetics, the development of arterial hypotension, bradycardia, artymia, and cardiac arrest is possible. In children, it may be difficult to detect early signs of local anesthetic toxicity when performing blocks during general anesthesia. Treatment If signs of acute systemic toxicity occur, the use of local anesthetics should be discontinued immediately. Treatment should be aimed at quickly stopping seizures and maintaining oxygenation and circulation. Oxygen should be provided and, if necessary, mechanical ventilation should be performed. If the convulsions do not stop spontaneously after 15–20 s, the patient is given intravenous sodium thiopental 1–3 mg/kg or intravenous diazepam 0.1 mg/kg. Administration of a muscle relaxant (for example, suxamethonium 1 mg/kg) quickly stops seizures, but requires intubation and mechanical ventilation. When blood pressure decreases/bradycardia, vasopressor agents, such as ephedrine 5–10 mg, are administered intravenously (the administration can be repeated after 2–3 minutes). In case of asystole, cardiac massage should be performed. It is necessary to maintain optimal levels of oxygenation, ventilation and circulation while correcting acidosis. When treating symptoms of toxicity in children, doses that are appropriate for their age and body weight should be used. Total spinal block Symptoms: a rare adverse reaction to spinal anesthesia is widespread or total spinal block, which leads to depression of cardiovascular activity and respiration. Depression of cardiovascular function is caused by extensive sympathetic blockade, which can lead to hypotension, bradycardia, or cardiac arrest. Respiratory depression may be caused by blockage of the innervation of the respiratory muscles, including the diaphragm. Treatment: if signs of extensive or total spinal blockade occur, the use of the drug should be stopped immediately. Treatment should be aimed at maintaining oxygenation and circulation. Oxygen supply should be provided and, if necessary, mechanical ventilation should be performed. When blood pressure decreases and bradycardia, vasopressors, such as ephedrine 5-10 mg, are administered intravenously (the administration can be repeated after 2-3 minutes). In case of asystole, perform cardiac massage. It is also important to correct acidosis.
A new local anesthetic ropivacaine (naropin) in the practice of an anesthesiologist at a multidisciplinary hospital
Koptsov Sergey Vladimirovich (E-mail)
Alexander Hospital (St. Petersburg)
The desire to use fewer drugs that have the maximum necessary properties is the ideal that every anesthesiologist strives for in his practice. The main requirements for drugs are their therapeutic breadth, reliability, predictability and safety. The desire to find a “golden” mean applies equally to local anesthetics, the interest in which has grown extraordinary over the past 10 years. This phenomenon is caused by the revival of regional analgesia methods, their more significant introduction into surgical practice, and the mastery of these methods by the majority of anesthesiologists. Demand creates supply, and now, new generations of these representatives are appearing in the group of amide local anesthetics, the latest of which is ropivacaine (naropin - AstraZeneca). But let's go back to basics. What are local anesthetics? The most complete definition of these drugs is given by V.M. Vinogradov (1985): “Substances that selectively block the excitability of sensory endings and the conduction of impulses in nerve trunks at the site of direct use, and in high concentrations, a general sensory block at the site of administration.” In 1879, the Russian scientist V.K. Anrep, and in 1884, the Englishman Koller, discovered and described the local anesthetic effect of Erythroxylon coca; which served as an impetus for the subsequent synthesis of a large number of drugs related to local anesthetics. Based on the chemical structure, two main groups can be distinguished:
1. Esters of aromatic acids, where the ester link is located between the aromatic end of the molecule and the intermediate chain.
These include: novocaine, dicaine, tetracaine, etc.
2. Amides, the amine link of which is located between the aromatic end and the intermediate chain. These include lidocaine, xylocaine, bupivacaine, ropivacaine, etc.
The main difference between ester- and amide-containing compounds lies in the different metabolic pathways and their allergenic potential, as well as their chemical stability. Esters are destroyed by pseudocholinesterase to para-aminobenzoic acid, which can cause allergic reactions, and amides are destroyed by liver enzymes, without the formation of acid. Esters are not stable enough in solution compared to amides. The chemical structure largely determines the analgesic properties of the drug. So, if you increase the molecular weight, lengthen the intermediate chain, or include an additional carbon atom in the aromatic or amine part, you can enhance the drug’s own anesthetic capabilities (Takman, 1975). The aromatic part of the product determines the degree of its lipophilicity, and the amine part determines its hydrophilicity. The greater the degree of lipophilicity and the better the binding to proteins, the longer the effect of the drug. The timing of the onset of pain relief is directly dependent on the amount of the uncharged form of the drug (Ritchie et al., 1965). Thus, 35% of lidocaine is in unionized form, and bupivacaine is only 15%, therefore, the rate of development of the effect of lidocaine is 2 times higher (Bridenbaugh, 1975).
Three concepts are used to characterize local anesthetics:
- relative toxicity,
- relative strength of action,
- anesthetic index (Pashchuk A.Yu., 1987).
Relative toxicity is the ratio of the minimum lethal dose (MLD) of novocaine to the MLD of the new drug.
Relative potency is the ratio of the minimum effective dose (MAD) of novocaine to the MDA of the new drug.
The ratio of the potency of a drug to its relative toxicity is called the anesthetic index of the drug.
.
Based on these basic criteria, it is possible to characterize the local anesthetics most often used in anesthesiological practice.
Lidocaine.
- Strength of action – 4.
- Toxicity – 1.4.
- Anesthetic index – 3.
- The hidden period is 5-8 minutes.
- Duration – 3.5 hours.
Trimekain.
- Strength of action – 2-3
- Toxicity – 1.4.
- Anesthetic index – 2.
- The hidden period is 7-9 minutes.
- Duration – 2.5 hours.
Bupivacaine.
- Action power – 16
- Toxicity – 8.
- Anesthetic index – 2.
- The hidden period is 7-9 minutes.
- Duration – 8-12 hours.
Ropivacaine.
- Action power – 20
- Toxicity – 7.
- Anesthetic index – 3.
- The hidden period is 7-9 minutes.
- Duration – 8-12 hours.
Material and methods.
At the Alexandrovskaya Multidisciplinary Hospital of St. Petersburg, comprehensive clinical studies of a new local anesthetic, ropivacaine (naropine), were conducted in 62 surgical patients over 3 months in 2001. The mean age was 56.6±6.4 years, the percentage of men and women was 56% and 44%.
The group included 37 trauma patients, 13 gynecological patients, 6 general surgical patients, 6 urological patients. The trauma surgery group included:
- 17 metal osteosynthesis of lower extremity bones (thigh, tibia, patella, ankle, foot).
- 9 metal osteosynthesis of the bones of the upper limb (humerus, forearm bones, clavicle).
- 6 simultaneous osteosynthesis of the bones of the upper and lower extremities.
- 5 hip replacements (including 2 total).
Gynecological operations include:
- 8 extirpations of the uterus with appendages.
- 3 plastic surgery of the vaginal walls.
- 2 ectopic pregnancies.
General surgical operations include:
- 3 resections of 2/3 of the stomach.
- 1 removal of varicose veins of the lower extremities.
- 1 herniotomy (groin).
- 1 appendectomy.
Urological operations include:
- 3 transvesical adenomectomies.
- 3 transurethral adenomectomies.
14 operations were performed on an emergency basis.
The patients were divided into 4 groups, depending on the method of anesthesia:
The first group included patients who underwent epidural blockade as a component of general anesthesia using the endotracheal technique.
The second group included patients in whom epidural analgesia was an anesthetic aid.
The third group included patients who underwent conduction blockade as a component of anesthesia.
The fourth group included patients in whom conduction analgesia was used as an independent technique.
All groups were divided into subgroups depending on the urgency of the surgical intervention. For anesthesia during surgery, 7.5% and 10% naropin were used, for postoperative pain relief - 2%, 7.5% and 10% naropin. In all cases, adrenaline was added to the anesthetic (at a ratio of 1 drop per 10 ml of solution). The control group included 60 surgical patients who received the local anesthetic bupivacaine (Marcaine) as an element of anesthesia. The studied groups of patients (control and main) were similar in age and gender. There were no significant (p<0.05) differences in these characteristics in the compared groups. They were also not found based on the concomitant pathology and profile of surgical patients. The control group also had four subgroups, similar to the main one. For analgesia during surgery and for postoperative pain relief, 0.5% marcaine with adrenaline was used. The following indicators were used to characterize patients:
- Physical condition of the patient (classification developed by the American Association of Anesthesiologists (ASA).
- Condition of the cardiovascular system. Systolic and diastolic blood pressure, pulse, and ECG were determined.
Non-invasive monitoring of vital functions during surgery was carried out using a cardiac monitor from the South Korean company BIOSYS using the following parameters: electrocardiography, measurement of systolic and diastolic blood pressure, plethysmogram, blood oxygen saturation. A universal monitor from the German company Hewlett Packard, which measures the following parameters: electrocardiography, measurement of systolic and diastolic blood pressure, plethysmogram, blood oxygen saturation, respiratory rate and pattern, tissue perfusion, body temperature. To assess analgesia, a verbal twelve-point rating scale was used, where 0 means no pain and 12 means intolerable pain. Regional anesthesia was carried out by high blockade of the main nerve trunks: for the lower leg - the sciatic and femoral nerves, for the thigh - blockade of the obturator and lateral cutaneous nerves is added to the above using the “three in one” technique (Winnie APet al., 1973). To perform a lumbar plexus block using the “3-in-1” method, it is necessary to apply pressure to the thigh area below the injection site while injecting the solution to the femoral nerve. This technique ensures that the local anesthetic solution spreads predominantly proximally along the femoral canal, which is necessary for blocking the obturator and lateral cutaneous nerves. To carry out a blockade of the brachial plexus, a supraclavicular approach according to Kulenkampff is used (Kulenkampff D., Persky A., 1928), or axillary (Pashchuk A.P., 1987). Electrical stimulation techniques are used to identify the nerve. For this purpose, the “KORDELEKTRO” pacemaker, manufactured in Kaunas, Republic of Lithuania, is used, which is a generator of rectangular stimulating pulses. Epidural blockade was performed at different levels, depending on the location of the operation. All patients underwent catheterization of the epidural space for subsequent administration of anesthetic. To carry out general anesthesia using the endotracheal technique, multicomponent, balanced anesthesia using muscle relaxants was used, where regional anesthesia was one of the components of the technique. All patients in the control and main groups were assigned to ASA classes 2–4.
Duration of action
The duration of analgesia was determined using a verbal self-assessment rating scale in the postoperative period. The use of narcotic analgesics (fentanyl) and α2-adrenergic agonists (clonidine) did not significantly (p<0.05) affect the effect of anesthetics. Table 1, 2 presents data on the duration of action of anesthetics in the control and main groups.
Table 1. Duration of analgesia in patients in the control group (marcaine) (M ± m, n = 100).
| Group | Duration of analgesia (hours). |
| 1 Group | 8,3± 1,2 |
| 2 Group | 7,5± 0,5 |
| 3 Group | 12,2± 1,4 |
| 4 Group | 11,3± 1,1 |
The duration of analgesia in patients where regional anesthesia acted as a component of anesthesia was significantly (p<0.05) longer than with a monocomponent technique, apparently due to the use of additional amounts of narcotic analgesics and ataractics.
Table 2. Duration of analgesia in patients of the main group (naropin) (M ± m, n = 110).
| Group | Duration of analgesia (hours). |
| 1 Group | 12,3± 0,5* |
| 2 Group | 10,5± 1,4* |
| 3 Group | 26,5± 1,5* |
| 4 Group | 22,3± 1,5* |
*- differences with the control group are significant (p<0.05).
There was a significant (p<0.05) difference in the duration of analgesic activity between the main and control groups. The greatest difference is observed in subgroups 3 and 4, where conduction anesthesia was performed. Just as in the control group, there was an increase in the duration of analgesia in cases of using regional anesthesia as a component of anesthesia. The duration of analgesia significantly (p<0.05) increased when using more concentrated solutions of local anesthetic. When using 7.5% naropin with adrenaline for conduction analgesia, the duration of action was 16 - 18 hours, the effectiveness was 4 - 5 points (according to a verbal 12-point self-assessment rating scale), when using 10% naropin with adrenaline - the duration of the blockade was - 19 - 34 hours, efficiency – 1 – 2 points (our data); when carrying out epidural anesthesia using 7.5% naropin with adrenaline - duration - 8 - 10 hours, when using 10% ropivacaine - 9 - 12 hours. Pain in most patients increased gradually and reached a maximum intensity not exceeding 6 points, which corresponded to the definition of pain as “moderate”. To prolong analgesia, a local anesthetic was injected into the epidural space through a catheter in fractions and drops. Most often (75%) bolus administration of the drug was used due to the simplicity of the technique and the possibility of training the patient himself. The disadvantage of this method was the appearance of tachyphylaxis already with the second or third injection. When administered by drip during the first two days at a rate of 20 mg/hour, analgesia was adequate and corresponded to 2–3 points (on the self-assessment scale). When performing a single conduction blockade, 76% of patients had no pain at all, which was obviously due to the fact that alteration and swelling during trauma operations decreased within 24–32 hours after the intervention.
Onset of action.
The timing of the onset of sensory and motor blockade is an integral characteristic of any local anesthetic. This indicator depends on the pKa value. This value is equal to the pH value, provided that the ionized and non-ionized forms of the local anesthetic are present in equal quantities. Diffusion of the anesthetic through the nerve sheath and membrane is determined by the uncharged form of the drug. For both marcaine and naropin, the pKa is 8.1, which corresponds to 15% of the non-ionized form, the average time for the onset of sensory blockade was: for epidural anesthesia - 14.5 ± 3.4 minutes; for conduction blockade – 24.3 ± 7.3 minutes. No significant (p<0.05) difference in the time of onset of sensory blockade was found between the control and main groups. The time of onset of analgesia during conduction blockade is largely determined by the accuracy of the local anesthetic entering the perineural space. To accurately identify the nervous structure, we used the method of electrical stimulation. Electrical stimulation was carried out with a current intensity of 0.5–2.5 mA and a duration of 0.5–1.5 mS. If muscle contractions appeared at 0.5 mA and 0.5 mC, the probability of direct contact of the needle with the nerve is almost 100%. In these cases, the time for the onset of sensory blockade decreased by 2 times.
The time of onset of motor blockade and its duration in patients of the control group were respectively:
- for epidural anesthesia: 25.5±7.3 minutes; 6.4± 1.3 hours;
- for conduction blockade: 45.5±8.3 minutes; 8.4± 1.2 hours.
In patients of the main group, motor blockade directly depended on the concentration of local anesthetic. Thus, using 2% naropin, no motor block was obtained. 7.5% naropin applied epidurally caused muscle relaxation after 23.3 ± 4.5 minutes, and the duration was 6.3 ± 1.2 hours; conductive use contributed to motor block after 45.2 ± 6.4 min. with a duration of 7.5 ± 1.5 hours. 10% naropin when used epidurally 18.3 ± 7.3 min. and 8.3± 1.1 hours; with conduction blockade – 32.2±5.3 min. and 12.2±2.3 hours. A similar phenomenon has found practical application in certain operations, for example, total hip arthroplasty using bone cement for both the acetabulum and the “leg,” which lasted 3.5 hours using 10% naropin with adrenaline, was accompanied by pronounced muscle relaxation, facilitating any movements in the joint. Extirpations of the uterus and appendages for rapidly growing fibroids, with nodes lasting more than 15 weeks, were carried out using both 7.5% and 10% naropin. Relaxation when using 7.5% naropin in 6 (85%) cases was not sufficient; it was necessary to additionally administer muscle relaxants (Arduan) and, therefore, switch to the endotracheal technique. The use of 10% naropin caused severe myoplegia and did not require additional use of muscle relaxants. During gastrectomy, all manipulations were performed on the upper floors of the abdominal cavity, even using 10% naropin, relaxation was not complete, in addition, using a local anesthetic at high levels of the spinal cord - there was a high probability of hemodynamic and respiratory disorders, so we used naropin only as anesthesia component.
Level of anesthesia.
The distribution of the anesthetic during its epidural use is largely determined by its concentration and baricity. The use of 0.5% marcaine led to significant (p<0.05) analgesia from the injection site 3–5 dermatoses above and 4–6 below. The use of 2% naropin at a dose of 2 mg/kg led to a significant (p<0.05) spread of analgesia from the injection site to 4–7 dermatomes above and 4–6 below. The use of 7.5% naropin at the same dosage significantly (p<0.05) caused analgesia in 2–4 dermatomes above and 5–7 below. The use of 10% naropin at the same dosage led to a significant (p<0.05) spread of analgesia to 1–2 dermatomes above and 6–8 below. The speed of spread of the anesthetic was influenced by the position of the body during epidural puncture; if the patient was on his side, the drug was distributed in all directions more evenly than in a sitting position, when the time for the onset of the effect (for operations in the lower half of the body) was reduced by 45%.
Dosage.
The dosage of local anesthetic affects the effects obtained from the block. As the concentration of naropin increases, a faster, longer-lasting and deeper blockade occurs. At the same time, the degree of motor blockade increases. Our data show that it is the dosage of the drug, and not the volume, that plays the leading role in determining the anesthetic effect. The volume of the drug may affect the area of distribution of anesthesia. The only use of small concentrations and a larger volume (according to our data) is possible when performing a lumbar plexus block using the “3 in 1” technique, since a large volume is “pushed” proximally through the inguinal canal in the direction of the lumbar plexus. Complete lumbar block occurs after administration of at least 30 ml of 2% naropin.
Tachyphylaxis.
Long-term use of local anesthetics is often accompanied by a decrease in sensitivity to the drugs, weakening and cessation of their action. The combination of these effects is described by the concept of tachyphylaxis (Renck et al., 1976). This phenomenon is not predictable both in terms of the time of its appearance after the onset of anesthesia and the rate of its regression in each individual patient. The occurrence and rate of increase of tachyphylaxis are not related to the gender, weight and body surface area of the patient, or to the location and duration of the operation (Mogensen et al., 1988). An explanation for this phenomenon has not yet been found. All patients in the control and main groups, where epidural anesthesia was used, received postoperative administration of local anesthetics for prolonged analgesia. In the control group, 65%, and in the main group, 78% of patients developed tachyphylaxis to the local anesthetic after a single injection. When using concentrated solutions of naropin during surgery, repeated administrations of less concentrated solutions of the drug or other local anesthetics of the amide group led to a sharp decrease in analgesia up to its complete absence. The dynamics of the duration of analgesia with subsequent administration of marcaine and naropin are presented in Table 3.
Table 3. Dynamics of the duration of pain relief in patients of the control and study groups (M ± m)
| A drug | Duration of analgesia (hours). | ||
| 1st introduction | 2nd introduction | 3rd introduction | |
| 0.5% marcaine | 3,4± 0,4 | 2,3± 0,4 | 1,5± 0,2 |
| 2% naropin | 2,3± 0,4 | 1,1± 0,2 | 1,0± 0,1 |
| 7.5% naropin | 4,5± 0,3 | 2,3± 0,3 | 1,2± 0,2 |
| 10% naropin | 5,3± 1,1 | 3,1± 0,4 | 1,4± 0,5 |
The table data shows that by the 3rd injection the duration of analgesia becomes approximately the same in all cases. The concentration of the anesthetic determines the duration of analgesia only after the first administration of the drug, then a decrease in sensitivity occurs to a certain threshold value. The use of adrenaline did not significantly (p<0.05) affect the degree of tachyphylaxis. The use of narcotic analgesics significantly (p<0.05) reduced the percentage of cases of insensitivity to anesthetics.
Toxicity.
General toxic reactions most often occur in the central nervous system, cardiovascular system and respiration, as well as the function of the pelvic organs. When using 0.5% marcaine, hemodynamic disturbances were observed in 20% of cases in the form of hypotension by 35–40% of the initial value. Such changes are especially typical for patients who underwent emergency operations, elderly patients, as well as when using a2-adrenergic agonists (clonidine). The use of 2% naropin did not significantly (p<0.05) affect hemodynamics; the use of 7.5% and 10% naropin caused a slight decrease (mainly in systolic blood pressure) in hemodynamics by 20% compared to baseline. The urgency of surgery did not significantly (p<0.05) affect the cardiovascular system. As in the control group, a significant change in hemodynamics occurred with the use of clonidine. In one patient, when using 10% naropin during extirpation of the uterus and appendages (the patient corresponded to group 2), there was a rhythm disturbance in the form of atrial bigeminy for 35 minutes at the initial stages of the operation, which did not manifest itself hemodynamically and stopped on its own. Epidural analgesia in both the control and main groups at a level below Th12 was not accompanied by respiratory disorders. A higher use of epidural blockade occurred against the background of the use of mechanical ventilation, so it was not possible to identify reliable breathing disorders. Oxygen saturation in both the main and control groups was within the physiological norm. No CNS disorders were found in both groups. No dysuric or other dysfunctions of the pelvic organs were detected. No allergic or other manifestations of hypersensitivity were identified in both groups.
Recommended areas for further clinical research.
- To determine the possibility of using mixtures of naropin with lidocaine to reduce the latent period while maintaining the duration and adequacy of analgesia.
- To clarify the selectivity of the action of naropin at various concentrations and the possibility of regulating and controlling these effects.
- To determine the effect of orthostatic tests on the location and duration of analgesia when using different concentrations of naropin.
- Determine the factors influencing the decrease in sensitivity to naropin and ways to overcome tachyphylaxis.
- Try naropin for subdural use.
conclusions
During a clinical trial of the local anesthetic naropin, conclusions and practical recommendations were formulated:
- The local anesthetic of the amide group of the latest generation, ropivacaine (naropin), best corresponds to the concept of an “ideal” drug, due to its therapeutic breadth of action, duration, effectiveness, low toxicity, and safety.
- Its most effective use is for trauma surgeries on the extremities, when, once applied during conduction blockade, it is able to provide long-term adequate analgesia for a period of more than 18 hours.
- The epidural use of naropin during trauma operations on the area below the knee, when quality pain relief could only be provided by a subdural (intrathecal) blockade, made it possible to carry out such surgical interventions.
- The use of naropin in the anesthesia complex using the endotracheal technique made it possible to reduce the total consumption of drugs.
- Using naropin in urological and gynecological practice, it is possible to implement a monocomponent epidural blockade technique.
- The combination of naropin with narcotic analgesics helps reduce the incidence of tachyphylaxis and more effective pain relief.
- The most effective use of the analgesic properties of naropin in the postoperative period is the use of a drip method of administering the drug into the epidural space at a rate of 20 mg/hour.
- Naropin is recommended for use in both planned and emergency operations, especially in cases of combined injuries, even without the use of catheterization of the perineural space.
Literature _
- Vinogradov.V.M. Pharmacology (general, specific and clinical basics). – 1985. – L. – VmedA. – 516s.
- Pashchuk A.Yu. Regional anesthesia. - M.: Medicine, 1987.-160 p.
- Bridenbaugh PQ Intercostal nerve blockade for the evaluation of local anaesthetic agents // Br. J. Anaesth. – 1975. – V.47. - No. 306. – P.183-201.
- Kulenkampff D., Persky A. Brachil plexus anaesthesia // Ann.Surg., 1928. - No. 87. – P.883-891.
- Mogensen T., Hjorts NC, Bigler D. Unpredictability of regression of analgesia during the continuous postoperative extradural infusion of bupivacaine // Br. J. Anaesth. – 1988. – V.60. - No. 515. – P.621-627.
- Renck H., Edstrom H., Kinnberger B., Brandt G. Thoracic epidural analgesia. Prolongation in the early postoperative period by continuous injection of 1% bupivacaine // Acta Anesth. Scand. – 1976. – V.20. - No. 47. – P.69-74.
- Ritchi JM, Ritchi B., Greengard P. The active structure of local anesthetics // J.Pharmacol Exp.Ther. – 1965. – V.150. - No. 152. – P.128-131.
- Takman BH The chemistry of local anesthetic agents: classification of blocking agents // Br. J. Anaesth. – 1975. – V.47. - No. 183. – P.85-95.
- Winnie AP, Ramamurthy S., Durrani Z. The inguinal paravascular technic of lumbal plexus anesthesia: the “3-in-1” block //Anesthes., Analg. - 1973. - No. 52. — P.989-996.