Neuromidin is a special drug that is neither a muscle relaxant, nor an analgesic, nor an anti-inflammatory drug. It is not included in any international or domestic protocol for the treatment of acute back pain, and even more so when the pain is caused by discogenic complications of osteochondrosis (protrusions and hernias). The cost of Neuromidin is quite high, exceeding 1000 rubles. Let's figure it out: does using Neuromidin really help with a herniated disc, or is it just a waste of money?
This question is far from idle. Intervertebral protrusions and hernias have all the signs of “convenient” diseases for healers and charlatans. These are the signs:
- there is no immediate threat to life or disability;
- There are many intervertebral discs, and pain is common;
- Acute, discogenic back pain lasts for many years, with alternating exacerbations and remissions, and the patient can be “used” for many years, since the pain goes away anyway, and by using some dubious remedy, you can convince the patient that it helped;
- the severity of the pain is high, and with lumbago the patient cannot turn around and laugh for several days, since the inflamed nerve roots immediately shoot out, and at this time the patient is ready for anything.
Thus, there are many options for conservatively “treating” a hernia: ointments, creams, kinesiotherapy and craniosacral effects, massage and physiotherapy, manual techniques and blockades. One thing to remember: all these treatment methods have nothing to do with a hernia, as with an intervertebral disc defect. They help eliminate the unpleasant symptoms caused by the hernia by “rubbing” the nerve roots, ligaments and muscles.
Without exception, all conservative methods of treatment only help to relieve pain and increase range of motion in the back, but at the same time this is not evidence of a radical cure. This is the result of reduced inflammation, pain and swelling, improved blood supply to surrounding tissues and decreased muscle tone. The hernia will manifest itself again, perhaps it will enlarge, and these methods of conservative treatment will no longer help. Then only surgery will save you.
Modern spinal neurosurgery
Only modern minimally invasive surgical intervention (for example, video endoscopic microdiscectomy, or laser vaporization and nucleoplasty) can remove the hernia defect itself, or prevent its appearance in the case of protrusion. However, the Russian patient knows very well what surgery is. It hurts. This takes you out of normal life for a long time. It may be dangerous. There are so many such “buts” that surgery is considered the last type of treatment, when massage therapists, carboxytherapy sessions, manual therapists and kinesiotherapists stop helping.
Fortunately, in European countries, Israel, and the USA, the approach is completely different. If there are indications, the patient is operated on without pain, and often leaves the hospital on his own feet on the same day or the next. His quality of life is preserved. He is not prohibited from sitting for many days, and he is not forced to relieve himself while standing. Therefore, modern surgery is considered the best, fastest and most effective means of radical treatment. By the way, doctors in many Eastern European countries, for example, the Czech Republic, show excellent results in treating hernias surgically at fairly modest costs.
In Russia, they prefer not to immediately remove the hernial protrusion, but for many years to deal with its consequences and complications - to periodically treat inflammation, pain and swelling of the roots, which persistently arise again and again. And in this respect, the domestic patient resembles an unfortunate driver who, instead of finally changing a punctured tire, is forced to pump it up every half hour of driving. Only, unlike the driver, a patient who has been “treating” a hernia for a long time sometimes spends several times more money than the operation would cost.
Cervical hernia on MRI.
But even among the drugs for relieving swelling, back pain, and excess muscle tension, Neuromidin is not “listed.” However, it is sometimes prescribed for hernias, and is completely unjustified. The situation is aggravated by an unimaginably large number of sites that are written with stunning medical illiteracy. Because if there is a request “How to take Neuromidin for hernias,” then a helpful but illiterate article will immediately appear, which can even harm your health. How to take Neuromidin for hernias? Don't accept it at all. But first things first….
Mechanism of action of the drug
It is known that the nerves give the order to the muscles to contract, acetylcholine, which is released into the synaptic cleft - the place where the nerve connects with the muscle. Acetylcholine, if not removed in time, will keep the muscle in prolonged contraction. Therefore, “cleaning” the synaptic cleft from acetylcholine is very important, and this is done by the enzyme acetylcholinesterase. So, Neuromidin inhibits it, and acetylcholine circulates longer in the synaptic cleft, and the impulse becomes brighter, longer, more active. It affects the level of potassium channels. As a result, neuromuscular transmission and smooth muscle contractility improve.
Indications for use: can it be used for hernias?
Therefore, Neuromidin should be used where there is a defect in neuromuscular transmission (for example, muscle weakness and lethargy, when there is a hereditary deficiency of acetylcholine). These are myasthenia gravis and various mysthenic-like syndromes.
The second indication is the actual bad nerves, through which the impulse is carried out poorly, with losses. This is polyneuropathy, for example, in diabetes mellitus, or alcoholic polyneuropathy. In the latter case, many years of alcohol consumption led to the destruction of nerves, and in the first case, high sugar levels. This also includes demyelinating diseases, for example, multiple sclerosis, when the myelin sheath of the nerves is defective, and a “short circuit” and impaired impulse transmission often occur due to poor insulation.
A wide group of indications are various paralysis and paresis, when neurons generate an impulse very poorly, and then it is necessary at the periphery, at the point where the nerve axon approaches the muscle, to somehow strengthen it. These are bulbar paralysis, paresis with motor deficit.
Finally, due to its effect on smooth muscle, Neuromidin is indicated for low intestinal tone and for the treatment of atonic constipation.
Is improved neuromuscular transmission necessary for hernias?
Of course not. Let's remember that:
- the motor neurons that “order” the back muscles to contract lie in the anterior horns of the spinal cord, and are very far from the hernia, which has no effect on them;
- improvement of neuromuscular transmission leads to increased impulse and long action time. With hernias, on the contrary, the muscles are excessively spasmed, and, on the contrary, they need to be weakened, removing the excessive action potential from them.
And finally, the “cherry on the cake”: acetylcholine is a transmitter of the parasympathetic nervous system, and it has nothing to do with the muscles of the trunk or lumbar region. Neuromidin stimulates effects such as:
- slowing heart contractions and dilating blood vessels in the periphery;
- decreased blood pressure;
- increased intestinal motility;
- contraction of the muscles of the gallbladder, bronchi and uterus;
- improved secretion of digestive juice;
- stimulation of the lacrimal and sweat glands, as well as reduction of pupils, due to the effect on the parasympathetic part of the oculomotor nerve.
In addition, acetylcholine is a nerve transmitter within the central nervous system and circulates within the brain. Its deficiency can cause Alzheimer's disease, and therefore Neuromidin can also be used as a drug to help slow the progression of symptoms of this disease.
As you can see, this remedy has nothing to do with herniated intervertebral discs, and cannot have it. Its mechanism of action lies outside the influence on inflammation, pain, swelling and muscle spasm, which occurs with protrusions and hernias.
Side effects and contraindications
Neuromidin is a serious drug. If it is used in high doses, it may cause chest pain, vomiting, dizziness, and headache. In women, the tone of the uterus may increase. Since muscarinic cholinergic receptors are stimulated, symptoms of overdose in patients may include diarrhea, sweating, palpitations, excessive sputum discharge, up to signs of bronchospasm, and even convulsions may occur.
The list of contraindications for taking Neuromidin is also quite impressive. This includes pregnancy, breastfeeding, and childhood and adolescence, including 18 years of age. The drug is strictly prohibited in patients with:
- epilepsy;
- dizziness and vestibulopathies;
- with sick sinus syndrome and rare heart contractions, in the presence of bradycardia;
- for bronchial asthma and angina pectoris;
- with intestinal obstruction or urinary tract obstruction;
- the drug is strictly prohibited in patients with gastric and duodenal ulcers and especially in the acute stage.
There is also a list of diseases when Neuromidin can be used according to indications, but with great caution. These are various obstructive pulmonary diseases, bronchitis and thyrotoxicosis, diseases of the cardiovascular system, in the presence of panic attacks, and cardioneurosis, since the drug can reduce the threshold of convulsive readiness.
It is strictly forbidden to drink alcohol during treatment, since the number of side effects of the drug together with ethyl alcohol increases. During treatment with Neuromidin, the patient should not drive a vehicle, or work in production if there are risk factors, since the drug cannot guarantee the speed of psychomotor reactions and good concentration.
The role of neuromidin in the rehabilitation of patients with vestibular dysfunction
Rehabilitation of patients with vestibular dysfunction remains one of the relevant and priority areas in modern otorhinolaryngological practice. The medical and social significance of the problem is determined by the high level of morbidity, persistent disability due to severe vegetosomatic symptom complex and the development of hearing loss that accompany the course of the disease [3, 4, 10, 14, 15, 16]. Limitation of the possibility of full communication, caused, among other things, by impaired auditory reception, leads to a significant decrease in the quality of life of patients with vestibular dysfunction [2].
Treatment tactics are traditionally based on knowledge about the etiology and pathogenesis of vestibular disorders. However, the lack of a unified concept of the development of disorders in the functional balance system [1, 4, 10, 16] leads to a variety of methods of conservative treatment of the disease, most of which are empirical, and the observed clinical effect is sometimes difficult to explain [9]. Hearing loss is associated with disturbances in hemo- and liquorodynamics, metabolic processes of receptor cells, and the ionic composition of the fluids of the inner ear. An important role in the deterioration of auditory perception is assigned to changes in cholinergic mediation [6, 7, 8]. In this regard, the treatment regimens for patients include anticholinesterase substances, used in courses in the interictal period. A new drug in this series is ipidacrine (neuromidin).
The mechanism of pharmacological activity of the drug is based on the blockade of potassium permeability of the cell membrane and reversible inhibition of cholinesterase, which increases the activity of the presynaptic axon and stimulates neuromuscular conduction.
We assessed the effectiveness of rehabilitation of patients with peripheral vestibular dysfunction when supplementing complex treatment with ipidacrine (neuromidine). 64 patients who were undergoing inpatient treatment at the clinic for ear, nose and throat diseases of SamSMU were examined. Among the examined, 21 were men (32.8%), 43 were women (67.2%), the average age of the patients was 48.8±0.5 years. In 85.9% of cases, unilateral lesions were diagnosed, in 14.1% of cases the disease was bilateral. The average duration of vestibular dysfunction was 14.8±0.3 years. The development of vestibular disorders in all patients preceded the appearance of hearing impairment. The main complaint was attacks of systemic dizziness, accompanied by gait disturbances and balance disorders, fluctuating hearing loss, speech intelligibility was impaired in 24 people (37.5%), tinnitus bothered 31 patients (48.4%).
The main group consisted of 30 patients with peripheral vestibular dysfunction, of which 11 were men (36.7%), 19 women (63.3%); the average age of patients in the group was 49.2±0.4 years. The control group included 34 patients: 10 men (29.4%), 24 women (70.6%); average age 48.4±0.5 years. All patients underwent acumetry, vestibulometry, and quality of life assessment using the SF-36 questionnaire before the start of treatment and after its completion.
The complex treatment regimen included the use of medications that improve hemomicrocirculation and metabolic processes of the brain, meatotympanic, intranasal blockades according to Ageeva-Maikova, and physical therapy exercises. Patients in the main group additionally received ipidacrine (neuromidine) in tablets of 20 mg 3 times a day after meals for 21 days. The criterion for limiting the use of the drug in the main group of patients with peripheral vestibular dysfunction was the presence of heart rhythm disturbances and severe forms of angina. The use of ipidacrine (neuromidin) in a complex treatment regimen did not cause a worsening of vestibular symptoms in any patient of the main group.
To characterize the severity of complaints and subjective sensations of a patient with vestibular dysfunction at the peripheral level, we used a rating scale in points. In patients of the main group, positive dynamics of the state of auditory function and a decrease in the intensity of ear noise were noted already on the 6th–7th day of treatment; similar changes in patients in the control group were observed on the 10th day.
An analysis of the dynamics of tonal hearing thresholds during air conduction (AP) and bone conduction (BC) was performed taking into account the degree of hearing loss. To assess the effect of the drug in patients with initial hearing loss, a degree of hearing loss of 0 was allocated, corresponding to a decrease in auditory sensitivity to tones in the speech frequency zone of up to 10 dB. Degree I of hearing loss was characterized by an increase in hearing thresholds in the specified range by 11–40 dB, degree II by 41–60 dB, degree III by 61–80 dB.
In all subjects of the main and control groups, after the course of treatment, a positive trend in the dynamics of tonal hearing thresholds was determined. Changes in hearing sensitivity turned out to be most significant at degrees 0 and 1 of hearing loss.
Tonal hearing thresholds during EP in patients of the main group with 0 degree of hearing loss decreased from 10.0±0.01 dB, with degree I - by 1.7±0.3 dB, with degree II - by 5.0±0.01 dB. Tonal hearing thresholds in CP also tended to improve: at grade 0 - by 2.5±0.9 dB, at grade I - by 3.3±2.1 dB. In patients with II degree of hearing loss according to the CP and III degree of hearing loss according to the VP and CP, no dynamics were observed. At frequencies of 4000–8000 Hz, no significant changes in auditory sensitivity were detected. A slight improvement in tonal hearing according to CP was determined in persons with II degree of hearing loss, and according to VP in patients with III degree of hearing loss.
In the control group, the thresholds of tonal hearing during air conduction in patients with degree 0 hearing loss did not change, with degree I they decreased by 2.5 ± 7.5 dB, with degree II they decreased by 5.0 ± 0.01 dB. Tonal hearing thresholds with bone conduction also tended to improve at grade 0 by 2.5±2.5 dB, at grade I by 2.9±0.6 dB. In case of II degree according to CP and III degree of hearing loss according to VP and CP, no changes were detected. At frequencies of 4000–8000 Hz, there was a slight improvement in tonal hearing in CP in persons with 0 degrees of hearing loss and in VP in patients with 1 degree of hearing loss.
A comparative assessment of the dynamics of auditory sensitivity to tones of the speech and high-frequency ranges indicated large positive changes in patients receiving ipidacrine (neuromidin) as part of complex treatment.
We did not detect any significant changes in the differential threshold for the perception of sound intensity (DPST) at frequencies of 500, 1000, 2000, 4000 Hz in patients of the main and control groups (p > 0.05). Changes in the thresholds of 50% and 100% speech intelligibility in patients of both groups were characterized by a tendency to improve. A direct correlation was revealed (r = 0.31, p < 0.05) between the treatment result for auditory function and the duration of the disease.
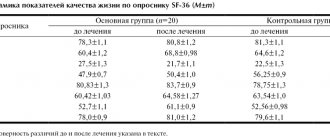
To assess the quality of life of patients with vestibular dysfunction at the peripheral level, we used the nonspecific questionnaire SF-36, which allows us to determine the physical and psychological components of the patient’s health. According to the analysis, patients in the main group showed an improvement in their general health and treatment prospects from 42.5±3.7 to 56.4±6.2 points. The psychological component of health increased due to an increase in the degree of social activity (SF) by 9.26±2.3 points, the patient's vital activity (VT) by 5.4±1.9 points and his emotional state.
In the control group, similar changes in quality of life as the main criterion for the effectiveness of rehabilitation measures were characterized by lower values and were observed in a smaller number of patients.
Thus, the inclusion of ipidacrine (neuromidin) in a complex treatment regimen for patients with vestibular dysfunction at the peripheral level made it possible to achieve greater improvements in auditory function and quality of life indicators. The results of complex acumetry justify the need for possible early administration of the drug already at the initial stages of hearing impairment. The use of ipidacrine (neuromidine) in a comprehensive rehabilitation program for peripheral vestibular dysfunction in the interictal period did not lead to the appearance of vestibular symptoms.
Literature
- Askova L.N. Meniere's disease. Publishing house Saratov. Univer., Samara branch, 1991. 254 p.
- Babiyak V.I., Mitrofanov V.V. Some psychological and philosophical aspects of the problem “quality of human life”//Sb. tr. All-Russian conference. The problem of rehabilitation in otorhinolaryngology. Samara, 2003. pp. 36-40.
- Babiyak V.I., Lantsov A.A., Bazarov V.G. St. Petersburg: Hippocrates, 1996. P. 130-143.
- Gofman V. R. History of the development of vestibulology at the Department of Otorhinolaryngology of the Military Medical Academy // Theoretical and practical problems of modern vestibulology: Abstracts. report All-Russian Scientific Conference October 29-30, 1996. St. Petersburg, 1996, pp. 15-24.
- Eremina N.V. Medical aspect of rehabilitation of patients with vestibular disorders: Author's abstract. dis. ...Dr. med. Sci. Samara, 2000. 508 p.
- Nekhamkina G. S., Khrappo N. S., Mirkina A. Ya. To study the state of the cholinergic system in otosclerosis and Meniere’s disease // Non-purulent diseases of the ear: Tr. Kuibysh. honey. Institute named after D. I. Ulyanova. Kuibyshev, 1975. T. 95. P.125-129.
- Palchun V. T., Buyanovskaya O. Ya., Almazova V. I. The role of serum osmolarity in the pathogenesis of Meniere’s disease // Vestn. otorhinolaryngology. 1983. No. 3. P. 3-7.
- Pluzhnikov M. S., Komarovich G. M., Yantareva L. I. On the content of free acetylcholine in human perilymph // Vestn. otorhinolaryngology. 1972. No. 5. P. 28-32
- Sagalovich B. M., Palchun V. T. Meniere's disease. M.: MIA, 1999. pp. 433-435.
- Soldatov I. B. Physiology and pathology of the vestibular apparatus // Eighth Congress of Otorhinolaryngologists of the USSR: Abstracts of reports. Suzdal, 1982. pp. 177-184.
- Soldatov I. B., Khrappo N. S. Acute vestibular dysfunction and its treatment: Methodological letter for otorhinolaryngologists. Kuibyshev, 1975. 13 p.
- Soldatov I. B., Khrappo N. S. Drug treatment of Meniere’s disease // Pathology of the hearing organ: Coll. tr. Moscow Research Institute of Ear, Nose and Throat. M., 1984. P. 50-57.
- Soldatov I. B., Sushcheva G. P., Khrappo N. S. Vestibular dysfunction. M.: Medicine, 1980. P. 182-188.
- Guide to otorhinolaryngology/Ed. I. B. Soldatova. M.: Medicine. 1997. 608 p.
- Shvartsman N. A. Some questions of the pathogenesis of labyrinthine dysfunctions / Journal of ear, nose and throat diseases. 1984. No. 2. P. 48-55.
- Yanov Yu. K., Novikov V. S., Gerasimov K. V. Beginnings of system analysis in clinical and experimental vestibulology. St. Petersburg: Nauka, 1997. 240 p.
N. V. Eremina , Doctor of Medical Sciences, Professor T. Yu. Vladimirova Samara State Medical University, Samara
Interactions with other medications
Neuromidin may also interact with other medications. It enhances its sedative effect if used with drugs that depress the central nervous system, such as sleeping pills, tranquilizers from the benzodiazepine group, or together with barbiturates. Let us recall that a well-known representative of barbiturates, phenobarbital, is included in Valocordin and Corvalol, which are sold without a prescription. If you combine Neuromidin with beta-blockers, which reduce the heart rate and heart function, there is a risk of bradycardia, collapse and fainting.
Neuromidin
The drug Neuromidin is an m-, n-cholinomimetic, belonging to the group of anticholinesterase drugs and used in the treatment of diseases of the peripheral and central nervous system, as well as intestinal atony (in this case, only tablets). For many years, in the practice of a neurologist, the drug prozerin was used (and is still used), which has a powerful effect on postganglionic cholinergic synapses. Today, in a number of cases, clinicians prefer the drug neuromidin, as a drug that undoubtedly has a wider range of pharmacological activity, which can be successfully used not only for diseases of the peripheral nervous system, but also in cases of organic lesions of the central nervous system. The advantage of Neuromidin is its good tolerability and minimal negative side effects, which opens up additional opportunities for its use in elderly patients suffering from many comorbidities. You can learn about how this drug works, its benefits and features of use from this article.
Neuromidin stimulates the conduction of excitation waves along nerve fibers and synapses of the central and peripheral nervous system. Its action develops in two directions: blockade of potassium channels in the membranes of neurons and myocytes and temporary suppression of the activity of the cholinesterase enzyme in interneuronal and neuromuscular synapses. At the same time, neuromidin potentiates the effect of not only acetylcholine but also other mediators, including serotonin and histamine.
As a result, in addition to optimizing the conduction of nerve impulses and neuromuscular transmission, the drug enhances the contractility of smooth muscle cells and also improves memory. The initial effect of injection of neuromidin is observed, on average, after 15–20 minutes and lasts another 3–5 hours, which is due to prolonged blockade of potassium channels (while the effect of prozerin disappears 2–3 hours after a single injection). Neuromidin, unlike proserin, is in most cases well tolerated by patients: side effects, if they occur, are mild and do not require cessation of pharmacotherapy. When taking the drug, you should refrain from consuming alcohol, otherwise you can “create” a whole “bouquet” of negative side reactions for yourself with your own hands.
Neuromidin is available in two dosage forms: solution for intramuscular or subcutaneous administration and tablets. As for the doses and duration of use of the drug, everything is very individual: the doctor assesses the severity of the disease and a number of factors before deciding on treatment tactics. In case of an overdose of Neuromidin, they follow the popularly known principle of “knock out a wedge with a wedge”: in terms of biochemical realities, it will consist of taking drugs from the group of m-anticholinergics (atropine, cyclodol, etc.).
Release forms and analogues
Neuromidin contains the active substance - ipidacrine, it is available in the form of tablets, as well as a solution for injection. Tablets are sold in packages of 20 mg No. 50, and the solution for injection is sold in two dosages. The first is 5 mg per milliliter, and the second is three times more concentrated: 15 mg per milliliter of ipidacrine. One package contains 10 ampoules.
It is advisable to use Neuromidin for polyneuropathy, on average, one tablet from one to 3 times a day, the course of treatment is from one to 2 months. In the case of severe myasthenic crises, Neuromidin is administered intravenously, one or two ml, that is, up to 30 mg of a 1.5% solution, and then switched to tablet form.
In case of severe paralysis, the patient is prescribed 1 tablet 3 times a day for a long course, up to 6 months. In the presence of intestinal atony, the dosage is the same, one tablet 2-3 times a day, but the course is short - no more than 2 weeks. The maximum daily dose should not be more than 10 tablets, or 200 mg.
Neuromidin itself is not cheap: one package of tablets, which is enough for two weeks of use (1 tablet 3 times a day), costs an average of 1,350 rubles. Neuromidin is produced by the Latvian company Olainfarm.
An analogue is the Slovak (NVM-pharma) drug Ipigrix (1100 rubles for the same package), as well as the domestic Aksamon. It is produced by Peak Pharma, at an average price of 1263 rubles. per pack of 50 tablets.
Sensorineural hearing loss (SNHL) is observed in almost 3/4 of patients suffering from hearing impairment, and is a disease, the problem of diagnosis and treatment of which has not lost its relevance for many decades. Sensorineural (perceptual) hearing loss is a lesion of various parts of the auditory analyzer - from the hair cells of the cochlea (in most cases) to the auditory zone of the cerebral cortex.
Recently, the number of patients with sensorineural hearing loss aged 20-40 years who first sought help from an audiologist-otolaryngologist has been increasing. Such patients complain of hearing loss and tinnitus, which often causes more discomfort than with hearing impairment [1-3].
The wide prevalence of hearing loss in modern conditions is due to a large number of unfavorable factors leading to hearing loss and deafness. With all the variety of causes of SNT, microcirculation disorders up to capillary stasis play a leading role in its pathogenesis, which leads to ischemia of cochlear hair cells [4].
In the clinical picture of acute SNT, the leading place is occupied by complaints of sudden deterioration in hearing, a feeling of ear fullness, tinnitus, and often dizziness [5, 6]. The modern approach to diagnosing damage to the organ of hearing dictates the need to conduct a multifaceted examination of the patient, including a study of the function of the sound-conducting and sound-receiving systems, the vestibular analyzer, the study of indicators of the blood coagulation system and liver function, assessment of the state of the cardiovascular, excretory and endocrine systems, which makes it possible to establish the cause diseases and choose the most effective treatment tactics.
Treatment of patients with SNT remains a pressing problem in modern healthcare. This is determined by the growing number of hearing impaired people in industrialized countries, the growing social significance of hearing defects, and the low effectiveness of treatment [7].
Particular attention should be paid to the fact that only treatment started as early as possible will be effective. Taking into account the characteristics of the disease, medications are used that improve blood supply, including the inner ear, cerebral hemodynamics and rheological properties of blood, anticholinesterase agents, nootropic drugs, B vitamins, drugs with antioxidant properties, etc. [1, 4, 5, 8]. It should be noted that when using complex therapy with proserin, no positive dynamics were observed in 45% of cases.
To improve the conduction of nerve impulses from the receptor to the cerebral cortex and enhance cholinergic mediation in the treatment of SNT of various etiologies, the anticholinesterase drug neuromidin, an original modulator of neuroplasticity, produced in tablet and injection forms, is successfully used [9-11]. Unlike other drugs in this group, which temporarily inactivate the enzyme acetylcholinesterase in synapses, neuromidin additionally causes a blockade of potassium permeability of the membrane. This leads to an extension of the repolarization phase of the action potential and an increase in the activity of the presynaptic membrane, a subsequent increase in the entry of calcium ions into the presynaptic terminal and, as a consequence, an increase in the release of the transmitter into the synaptic cleft in all synapses.
The purpose of the work is to evaluate the effectiveness of using neuromidin for the treatment of SNT of various etiologies.
Patients and methods
Over the past 3 years, in the audiology department of the Samara Regional Clinical Hospital
them. M.I. Kalinin" observed 230 patients with SNT. Of these, 32 patients had acute CHF.
There were 168 patients in the age group from 40 to 60 years. The main cause of HF in this group was vascular disorders - hypertension, atherosclerosis of cerebral vessels, transient ischemic attacks. In 24 patients in the group from 20 to 40 years old, the cause of HF was acute viral infections, in 6 - acoustic and barotrauma, in 21 - vascular disorders (vegetative-vascular dystonia), in 5 - intoxication, in 6 - traumatic brain injury. Among patients diagnosed with SNT, 65% were women. Exclusion criteria from the study were the presence of severe angina and bradycardia in patients, pregnancy or lactation, epilepsy, mechanical obstruction of the intestine and urinary tract.
Patients of the 1st group (100 people) received traditional methods of treatment - prozerin 1 ml of 0.05% solution intramuscularly for 10 days, trental intravenously with glucose for 10 days, piracetam - 20% solution 2-6 g / day in a 0.9% solution of sodium chloride intravenously daily, 5 injections in total, nicotinic acid - 0.1% solution, starting with 1 ml, increasing the dose to 5 ml, then reducing it to 1 ml intramuscularly or intravenously; stugeron (cinnarizine) 0.05 g 2-3 times a day orally with meals. In case of acute CHF, glucocorticoids were added to therapy - dexamethasone (4 mg/day), prednisolone (30-60 mg/day) intramuscularly or intravenously.
Patients of the 2nd group (130 people) in the above complex therapy, instead of proserin, were prescribed intramuscularly the drug Neuromidin, 1 ml of 1.5% solution for injection (15 mg/day) for 10 days and then in tablets of 20 mg 3 times a day within a month. The effectiveness before and after treatment was assessed using clinical audiometric studies and rheoencephalography (REG).
Results and discussion
The majority of patients showed improvement in hearing and speech intelligibility, and in cases of acute SHL, in some cases, complete restoration of hearing. The effectiveness of therapy directly depended on the timing of the start of treatment. Improvement and complete recovery were noted in patients who applied within 10 days of hearing loss.
Subjectively, 28.5% of patients in group 1 and 54.3% of patients in group 2 noted an improvement in hearing and intelligibility of speech addressed to them. A decrease in subjective ear noise was noted by 25.7 and 47.1% of patients, respectively. A decrease in auditory sensitivity thresholds at frequencies of 500-2000 Hz with air sound conduction was recorded in 28.6 and 54.3% of patients, with bone conduction - in 30.6 and 54.3% of cases. Similar changes were noted at a frequency of 4000 Hz: in 28.6% in group 1 and in 47.1% in group 2, more often in persons with hearing impairment of noise origin. Improvement in cerebral hemodynamics was observed in 28.6 and 54.3% of patients, respectively. This was manifested by an increase in volumetric blood supply, a decrease in interhemispheric asymmetry of blood supply, and an improvement in venous blood flow.
Noteworthy are the results of treatment of patients who, along with basic therapy, took neuromidin: the number of cases of complete recovery increased and the number of cases without dynamics sharply decreased, in contrast to the group of people who did not take the drug. In addition, patients subjectively noted a decrease in tinnitus.
No side effects were identified while taking Neuromidin.
conclusions
Thus, the use of the drug Neuromidin intramuscularly at 1 ml of 1.5% solution for injection (15 mg/day) for 10 days and then in tablets of 20 mg 3 times a day for a month is justified and necessary in the treatment of sensorineural hearing loss, in including acute forms. Neuromidin has high clinical efficacy, good tolerability, and does not have serious side effects even with long-term use, which makes it possible to increase the effectiveness of therapy and improve the quality of life of patients.