Pharmacological properties of the drug Rebamipide
Rebamipide increases the endogenous content of prostaglandins E2 and I2 (PGE2 and PGI2) contained in gastric juice, and also increases the level of prostaglandin E2 (PGE2) in the gastric mucosa, promoting protection against damaging factors. Rebamipide exhibits a cytoprotective effect, proven in in vitro , improves blood circulation in the gastric mucosa and stimulates cell proliferation. By increasing the activity of enzymes that stimulate the biosynthesis of high molecular weight glycoproteins, rebamipide increases the amount of surface gastric mucus. Rebamipide does not affect basal and stimulated gastric secretion. After a single oral dose of 100 mg of rebamipide, the maximum concentration in the blood plasma - about 210 ng/ml - was determined after 2 hours. In in vitro , about 90% of rebamipide was bound to blood plasma proteins, however, numerous studies have proven that the substance does not accumulate in the body person. Subject to minor metabolism, most of it is excreted unchanged. The plasma half-life is approximately 1.5 hours. When rebamipide was used at a dose of 100 mg in patients with renal failure, there were no significant differences in the plasma concentrations and half-life of rebamipide between healthy and patients.
Rebamipide is a gastrointestinal protector with pleiotropic properties
In 2016, the drug Rebagit (rebamipide), which has no analogues in Russia, with proven effectiveness and safety, appeared on the domestic pharmaceutical market. This unique gastro- and enteroprotector is effective in the treatment and prevention of diseases not only of the gastrointestinal tract, but also of other organs and systems.
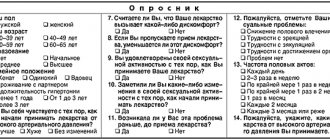
Table 1. Mechanisms of action of rebamipide
Table 2. Confirmed effects of rebamipide
The relevance of protecting the mucous membrane of the gastrointestinal tract (GIT) is due to the variety of exogenous and endogenous factors of aggression. The gastrointestinal tract's own protective apparatus (tight intercellular junctions, secretion of bicarbonates, growth factors, powerful blood supply system, etc.) does not always cope with this task, especially when simultaneously exposed to several damaging factors - hydrochloric acid, proteolytic enzymes, Helicobacter pylori
, non-steroidal anti-inflammatory drugs (NSAIDs), alcohol, nicotine, bile components, etc. [1, 2].
A new drug with gastro- and enteroprotective properties, rebamipide (a 2-quinolinone derivative), was developed by Japanese scientists at the end of the 20th century. Subsequently, its main effects were revealed: induction of the synthesis of prostaglandins E2 and GI2, improvement of blood flow in the gastrointestinal mucosa, reduction of its increased permeability, removal of free radicals, anti-inflammatory effect, increased secretion of gastric mucus [3–5] (Table 1).
Experimental studies of rebamipide
The first reports of the drug appeared in the late 1980s. Most of the experimental work on its study was carried out by Japanese scientists. In experiments on rats, it was shown that a new drug - a suspension of rebamipide - had an excellent effect on the healing of ulcerative defects of various origins (aspirin, indomethacin, stress, chemical agents) and prevented their development. However, the drug did not inhibit gastric secretion [6].
The results of another study demonstrated the ability of rebamipide to suppress celecoxib-associated apoptosis of cells in the gastrointestinal mucosa, which explained its protective effect, which was later confirmed [3].
To induce acute small intestinal injury, mice were treated with aspirin (200 mg/kg/day) for five days. Then the animals received rebamipide (320 mg/kg/day) for five days. Structural changes in the small intestine were assessed using electron microscopy. In mice treated with rebamipide, the damage was less pronounced and the intercellular spaces were more dense.
The researchers concluded that rebamipide administration during aspirin-induced injury improves intestinal barrier structure and promotes small intestinal regeneration by regulating cyclooxygenase 2 expression and beta-catenin accumulation [7].
In a number of in vitro
When using rebamipide in rats, the integrity of the intestinal barrier improved and the permeability of gastric epithelial cells decreased [8, 9].
Japanese scientists studied the capabilities of rebamipide in the prevention of gastrointestinal bleeding. In experiments on rats, gastric secretion was stimulated with histamine, after which aspirin was perfused. Oral clopidogrel was administered 24 hours before aspirin perfusion. Researchers evaluated the preventive effects of various antiulcer drugs, including rebamipide at doses of 3–30 mg/kg. As the results showed, the ability of rebamipide to prevent bleeding is comparable to that of antisecretory drugs and other protectors (irsogladine, teprenone). At the same time, rebamipide did not affect gastric secretion [10] .
Rebamipide is also characterized by an anti-inflammatory effect, and not only in relation to gastrointestinal diseases. The drug reduces the inflammatory response associated with the action of tumor necrosis factor (TNF) alpha, stabilizes the macrophage cell line, reduces the activation of nuclear factor kappa B (NF-kappa B), interrupting the inflammatory signaling pathway [11].
Due to its highly effective gastroprotective properties, rebamipide served as a standard in the study of other gastroprotectors. Thus, in a study of the gastroprotective properties of the drug PMK-S005 (synthetic S-allyl-L-cysteine) in acute ethanol-induced gastric damage in rats, it was compared with rebamipide (50 mg/kg) [12].
Today, due to the widespread use of NSAIDs, including low-dose aspirin (LDA), a drug with high protective properties is more relevant than ever. The number of patients, especially the elderly, chronically taking aspirin and/or NSAIDs is steadily increasing. At the same time, the frequency of gastrointestinal bleeding, particularly severe bleeding, increases. Active use of NDA for the prevention of cardiovascular and cerebrovascular complications leads to gastrointestinal ulceration and bleeding. The study of this problem, as well as preventive measures, largely concerned the upper gastrointestinal tract. The use of video capsule enteroscopy (VCE) has shown that NSAIDs damage not only the upper gastrointestinal tract, but also the small intestine, resulting in ulceration, bleeding and anemia. If gastric secretion plays a certain role in bleeding from the internal parts of the gastrointestinal tract, then the mechanism of damage to the intestinal mucosa, where there is no acidic environment, is not fully understood [13–15].
In a number of studies, NSAID-induced increases in reactive oxygen species (ROS) resulted in mitochondrial damage. As a result, the integrity of the intestinal mucosa was compromised. These data were confirmed in experiments on mice. When studying areas of damage to the small intestine while taking NSAIDs using fluorescence, an increased concentration of ROS was detected. The administration of rebamipide significantly reduced the concentration of ROS and the number of damaged cells in the mucous membrane of the small intestine. Most likely, this was due to the activation of manganese superoxide dismutase [16].
The enteroprotective properties of rebamipide are explained by its modulating effect on the microbiota. With the use of the drug, the concentration of enterococcus and enterobacteria in the mucous membrane of the ileum decreases to normal levels. In addition, inflammation is reduced due to the suppression of the gene responsible for the expression of TNF-alpha and Duox2 (dual oxidase that regulates the secretion of the salivary glands and gastrointestinal glands) [17].
Experiments on rats have shown that the use of rebamipide changes the composition of the esophageal microbiome, resulting in a reduced risk of developing Barrett's esophagus [18].
Unfortunately, eradication of H. pylori
, is not able to completely eliminate the risk of developing stomach cancer. Therefore, the problem of its prevention is still relevant today. Experiments on rats with induced carcinogenesis (N-methyl-N'-nitro-N-nitrosoguanidine) showed the preventive effect of rebamipide. The incidence of cancer in the rebamipide group was significantly lower than in the control group (p
A large number of patients require antiplatelet therapy. But even NDAs, when taken regularly, in more than 90% of cases lead to the development of gastro- and enteropathies (dyspepsia, acute damage to the mucous membrane, erosion, ulcers and their complications - ulcerative bleeding and death). Proton pump inhibitors (PPIs) are not always effective for the prevention and treatment of NSAID gastropathy. PPIs are ineffective for damage to the small intestinal mucosa and may reduce the effectiveness of antiplatelet therapy (omeprazole, esomeprazole).
The protective properties of rebamipide have been confirmed not only experimentally, but also clinically (Table 2).
Clinical researches
The antiulcer and anti-inflammatory effects of rebamipide against NSAID enteropathies, including when taking NDAs, were recorded in a study involving healthy volunteers. The total number of aspirin-associated ileal injuries by the fourth week of therapy in healthy volunteers was three times lower when using rebamipide (p = 0.03). Interestingly, the effectiveness of rebamipide is due not only to systemic action after absorption from the gastrointestinal tract, but also to direct local penetration into the gastrointestinal mucosa when moving through the gastrointestinal tract [20–22].
One of the key mechanisms for the development of enteropathy is a violation of the permeability of the mucous membrane of the small intestine. This mechanism was proven in a study comparatively assessing the effectiveness of rebamipide and PPIs in the treatment of diclofenac-induced enteropathy [23].
Another study examined changes in the histological appearance of gastritis in patients treated with rebamipide after eradication of H. pylori
.
169 patients who achieved successful eradication were randomly divided into two groups - study (n = 82) and control (n = 87). Patients in the main group received rebamipide. Histopathological changes were assessed using the updated Sydney system at baseline and one year later. The results showed a significant decrease in the severity of chronic inflammation in the area of the lesser curvature of the gastric body when taking rebamipide after eradication of H. pylori
compared with the control group (1.12 ± 0.08 versus 1.35 ± 0.08; p = 0.043) [24 ].
176 patients with chronic gastritis received rebamipide for 26 weeks. When assessing before and after treatment in the main and control groups using immunohistochemistry, it was found that rebamipide improved the condition of the gastric mucosa by reducing the expression of CDX2 (p = 0.021) and TFF3 (p = 0.012) - immunohistochemical markers of dysplasia and carcinoma. The drug was highly effective and safe, as well as good patient adherence to treatment [25].
In 38 patients receiving LDA (100 mg) for more than three months, high doses of rebamipide (300 mg/day) were used to treat enteropathy. After eight weeks of treatment, the number of lesions (ulcers, erosions) of the mucous membrane significantly decreased in the rebamipide group compared to the placebo group (p = 0.046), which was confirmed during VCE. High doses were tolerated satisfactorily [26].
Rebamipide significantly reduced the risk of small bowel bleeding as demonstrated by VCE in a study of 31 patients with coronary artery disease treated with an antiplatelet drug (thienopyridine) and an NSAID (hazard ratio 0.31, 95% confidence interval 0.12–0.82 , p = 0.02) [27].
Certain difficulties are associated with the prevention and treatment of gastric ulcers after endoscopic submucosal dissection. A systematic review and meta-analysis found that the addition of rebamipide to a PPI for eight weeks before and four weeks after the procedure reduced the incidence of ulceration and accelerated the healing time of postoperative ulcers compared with PPI alone [28–30].
In pilot projects (six studies, 611 patients), the addition of rebamipide increased the effectiveness of H. pylori
. Thus, in the group of patients who received rebamipide in addition to amoxicillin and PPIs, eradication was 73.3%, in the group without rebamipide - 61.4% (p
Side effects of the drug
As a protector, rebamipide is comparable to misoprostol, but is safer. Of 10,047 patients taking rebamipide, 54 (0.54%) reported adverse reactions, including laboratory abnormalities. Adverse events were predominantly associated with the gastrointestinal tract: constipation, flatulence, nausea, diarrhea. However, with the use of rebamipide, these phenomena were observed less frequently than with the use of misoprostol. In addition, minor changes in blood test results were recorded: increased levels of liver enzymes, urea nitrogen, alkaline phosphatase, leukopenia, lymphocytosis and thrombocytopenia. An important point: the nature and frequency of adverse reactions did not differ between elderly and non-elderly patients. Of 3035 patients over the age of 65 years, adverse reactions occurred in 18 (0.59%) [32].
Possible menstrual irregularities. Triple doses of rebamipide (900 mg/day) administered to healthy volunteers, as well as to patients with NSAID-induced enteropathy, were well tolerated [26].
A slight increase in transaminase levels without a hepatotoxic effect has been described in histological examination of the liver of rats treated with rebamipide. There were no structural changes in the liver, and the concentration of oxidative stress biomarkers did not change [33–35].
A 12-week, randomized, multicenter, double-blind study compared the efficacy and safety of rebamipide with those of misoprostol in 479 patients at high risk of NSAID complications. Rebamipide was better tolerated [33].
Thus, rebamipide has a cytoprotective effect on the mucous membrane of the stomach and small intestine under the damaging effects of various factors, primarily NSAIDs. The drug promotes the activation of enzymes that accelerate the biosynthesis of high molecular weight glycoproteins, increases the mucus content on the surface of the stomach wall, improves blood supply to the gastric mucosa, activates its barrier function, enhances the proliferation and metabolism of gastric epithelial cells, cleanses the mucosa of hydroxyl radicals and suppresses superoxides produced by polymorphonuclear leukocytes and neutrophils. This is confirmed by the results of experimental and clinical studies.
Effects of rebamipide on different organs and systems
The positive effects of the drug are observed not only in the gastrointestinal tract. A number of studies have shown that rebamipide inhibits joint inflammation by restoring the imbalance between Th17 and T-regulatory cells and activating Nrf2/HO-1 oxygenase [36]. In addition, after using a 2% solution of rebamipide in the form of eye drops for two weeks, the level of interleukins (IL) 6, 17, TNF-alpha in the tear fluid, and therefore the level of inflammation, decreases .
It has been shown that a 2% rebamipide suspension is much more effective than a 0.1% sodium hyaluronate solution in patients with dry eye syndrome [37].
The results of pilot studies of rebamipide demonstrated a good effect in the healing of ulcers and erosions of the oral mucosa in recurrent aphthous stomatitis and Behçet's disease. Rinsing with rebamipide solution is effective for inflammation of the oral mucosa in patients after chemotherapy [38–40].
The possibility of using rebamipide for vitiligo is being studied. Rebamipide, by inhibiting the cytokines IL-6, IL-8, IL-10, TNF-alpha and Th17, affects oxidative stress, which plays a role in the development of vitiligo [41].
In 2016, rebamipide appeared on the Russian pharmaceutical market under the trade name Rebagit (“PRO.MED.CS Prague a.o.”). Now in the arsenal of domestic doctors there is a unique gastro- and enteroprotector, which has no analogues in Russia, with proven effectiveness and safety. The drug can be used to treat and prevent diseases not only of the gastrointestinal tract, but also of other organs and systems.
Special instructions for the use of the drug Rebamipide
It should be prescribed with caution to elderly patients, since this category of patients has a risk of developing gastrointestinal disorders. Children . Rebamipide is not prescribed to children under 14 years of age as no studies have been conducted in this age group. Use during pregnancy and lactation. The safety of rebamipide during pregnancy has not been proven. Since rebamipide passes into breast milk, breastfeeding should be stopped and the issue of artificial feeding of the child should be decided if it is necessary to prescribe rebamipide to the mother during breastfeeding. There is no definite data regarding the effect on the ability to drive vehicles and operate complex mechanisms, but according to pharmacokinetic studies, such an effect is unlikely.