An umbilical hernia is a protrusion of internal organs through the fibrous ring of the navel. Most often, intestinal loops, the stomach wall, or the greater omentum come out. In children, this problem occurs mainly in the first months of life, which is associated with the anatomical features of the abdominal muscles and intrapartum complications. Mostly girls get sick. In total, about 12% of newborns have an umbilical hernia. However, surgical treatment is necessary for 30-40% of such children.
Description of the disease
A hernia in a child’s navel is one of the most common surgical pathologies, which is more often observed in premature babies and underweight newborns, which is due to the immaturity of connective and muscle structures.
In itself, such a protrusion is completely harmless, although it frightens parents with its appearance. It does not cause pain, itching or other discomfort and in the vast majority of cases goes away on its own. The threat is posed by a condition called strangulation: it is compression of the hernial sac, which entails a disruption of the blood supply and the gradual death of surrounding tissues. Strangulation of an umbilical hernia in children is a direct indication for immediate surgical treatment.
One day and no hernia!
Operations are performed under general anesthesia, specially designed for one-day hospitals. All medications used during surgery and for postoperative pain relief do not cause adverse or perverse reactions, which makes it possible to treat children with increased allergies and concomitant diseases. After the operation, the small patient is brought to the ward in a state of medicated sleep, where his parents or other loved ones are waiting for him, and where he is under the supervision of medical staff until he fully awakens. This achieves psychological comfort for both children and their parents, ensures the safety of postoperative awakening, and also neutralizes the elements of excitement characteristic of the post-anesthesia period. Treatment ends a week later with a visit to our Center for a follow-up examination of the child and removal of the suture.
Classification
There are several classifications of the disease according to certain criteria. The main thing is to distinguish types based on origin. There are two types:
- congenital or embryonic defects that occur in a child even at the stage of intrauterine development, they are caused by disturbances in the formation of the abdominal wall;
- acquired or postnatal hernias that develop in infants during the first 1–4 months of life.
Additionally, direct and oblique hernias are distinguished depending on the direction of the protrusion, as well as reducible and irreducible.
Rehabilitation period
This operation belongs to the so-called outpatient surgery. After direct surgery, the child spends 6 to 12 hours in the hospital, after which he is sent home. Before discharge, it is imperative to consult with your doctor to receive recommendations for caring for your child. It is very important to clean the wound daily and keep it clean. After a week (or 10 days), you must come to the Center to remove the stitches and observe the surgeon. It is worth noting that the rehabilitation period is quite easy, since almost all children tolerate such surgical procedures well.
Symptoms of an umbilical hernia in a child
First of all, the disease manifests itself externally in the form of a protrusion in the navel area, which is noticeable all the time or occurs when the baby coughs or cries. In a calm state, for example, when a child is sleeping, the hernia can almost completely “hide” in the abdominal cavity.
The size of the bulge varies from a few millimeters to 1–2 cm or more, and the larger the bulge, the more difficult it is to reduce under pressure. Additional signs of pathology may include:
- the appearance of brown spots in the navel area, which is caused by tissue scarring and the use of local antiseptics to treat the umbilical wound;
- an increase in the volume of protrusion when crying, the whims of the baby, during the period of ARVI, constipation, flatulence and colic;
- manifestation of a visible capillary network on a large hernia.
Children of preschool and school age may complain of discomfort and mild pain during physical activity, nausea, constipation and increased gas formation.
What is an umbilical hernia and why does it appear?
Umbilical hernia is one of the most common diagnoses in newborns: it occurs in approximately 20% of infants (and in children born prematurely, this figure is even higher) and is more common in girls than in boys. Visually, it looks like a navel protruding forward. It appears due to delayed closure of the umbilical ring, which is facilitated by a variety of factors, ranging from genetic predisposition to rickets. As a result, the free space is occupied by intestinal loops, parts of the peritoneum or omentum, which create a “bulge.” It can form already in the prenatal period, but because the baby screams and cries after birth, it, contrary to popular belief, will not appear by itself.
A protruding navel is not always noticeable to parents right from birth. It can begin to bulge in the first few months of a baby’s life, and even after he is six months old. At the same time, when the baby lies on his back, his stomach looks normal.
Reasons for the development of the disease
Hernias form due to weak muscles in the anterior abdominal wall. The causes of a congenital hernia in a child can be:
- hereditary predisposition;
- intrauterine infection;
- congenital defects and developmental anomalies.
The causes of acquired umbilical hernia in children can be:
- gastrointestinal disorders (constipation, colic, flatulence);
- getting up and walking earlier;
- hacking cough;
- constant crying and screaming;
- prematurity;
- excess body weight;
- accumulation of fluid in the abdominal cavity;
- birth weight deficiency;
- rickets;
- heredity;
- malnutrition.
It has been proven that the pathology is more common in premature babies: every third child born prematurely experiences this disease.
"Conspiracy" against hernia
Hernias of the lower part of the anterior abdominal wall in children and adults have different origins, and, therefore, the methods of their treatment in children and adults differ. Treatment of a hernia is possible only with surgery. The indication for surgery is an established diagnosis of a hernia, regardless of age. In children under 1 year of age, repeated strangulations are indications for hernia repair. The main purpose of the operation is the isolation and high excision of the hernial sac. The technique is traditional, but the art of the surgeon is to correctly assess the situation during the operation and try, if possible, to maintain the normal anatomical relationships of the organs in the groin area. The fact is that in the inguinal canal in boys there passes the spermatic cord, the elements of which are a vein and an artery that supply the testicle, as well as the vas deferens. Compression of these elements during surgery can lead to the death of the testicle, and insufficient strengthening of the wall of the inguinal canal can lead to recurrence of the hernia. In girls, when isolating the hernial sac, it is imperative to release the round ligament of the uterus, damage to which can cause infertility. It should also be taken into account that strangulation of a hernia in a girl is no less dangerous than in a boy, since the ovary very often descends into the hernial sac in girls, which, if strangulated, can die in 20 - 30 minutes.
Treatment of umbilical hernia in childhood
In general, the tactics of treating the disease can be divided into two areas: conservative techniques and surgical intervention.
A conservative approach is rational if the hernia is small in size, does not cause inconvenience and is not fraught with danger. Basically, a wait-and-see tactic is used: in most cases, umbilical hernias in young children go away on their own as they grow older. Additionally, the doctor may prescribe wearing a special bandage that minimizes the risks of pinching and further growth of the protrusion, massage, application of a patch and other auxiliary measures.
If the hernia has not healed in a child under 5 years of age, there are signs of strangulation, acute intestinal obstruction, or the size of the formation is alarming, surgical treatment is performed. It consists of repositioning the prolapsed internal structures into the abdominal cavity and suturing the hernial orifice. This operation is called hernioplasty and is carried out mainly as planned.
Which doctor deals with umbilical hernia?
A child with a hernia should be consulted with a pediatric surgeon. His task is to conduct an initial examination and make a qualified decision about whether surgery is needed in this case and, if necessary, when. The fact is that in almost 90% of cases the problem disappears with age on its own, without surgical intervention. Closing the umbilical ring is facilitated by infant massage and physical therapy. If the problem does not go away on its own, the operation is usually performed at the age of 5-6 years, before school.
It is almost impossible to miss an umbilical hernia, since in the first year of life the baby must visit a pediatric surgeon at least 2 times (at 1 month and at 12 months).
Is it necessary to operate on an umbilical hernia in a child?
During routine visits, the doctor performs a visual examination and palpation of the hernia. Each case has its own anatomical features, and the decision on surgical intervention should be made only by a competent pediatric surgeon! The size of the hernia and its structure are critical.
The main indication for hernioplasty in a baby is complications caused by an umbilical hernia: strangulation, tissue rupture. They are very rare. If the patient does not experience discomfort or pain in the abdominal area, he is less than 5 years old, and the bulge is small, then the likelihood of spontaneous closure of the ring remains, and the decision about surgery is postponed to a later date.
However, if the child has already turned 5, and it has not disappeared, most often surgery is still recommended. The same operation in a person over 14 years of age is more difficult.
Prevention
To prevent the intrauterine development of hernias, it is necessary to take planning and management of pregnancy seriously, regularly visit a doctor and undergo prescribed examinations.
The following measures will help avoid the formation of pathology:
- natural feeding of the baby or careful selection of formula;
- putting babies on their tummy every day;
- During breastfeeding, the mother follows a balanced diet without foods that increase gas formation (legumes, cabbage, flour confectionery);
- daily bathing and gymnastics.
It is undesirable to let babies cry and scream for a long time and hysterically: increased pressure on the abdominal wall can provoke divergence of the hernial orifice and further growth of pathology.
What not to do if parents identify signs of an umbilical hernia in a child:
- heat, cool, rub and knead the protrusion area;
- apply any ointments, creams, folk remedies to the navel;
- independently give children any medications without a doctor’s prescription;
- forcefully reduce the protrusion if it does not respond to light pressure.
At the first signs of infringement, which include discoloration of the skin in the navel area, vomiting, bloating against the background of the child’s crying, it is necessary to call emergency assistance as quickly as possible or take the child to the hospital yourself.
If you suspect the presence of an umbilical hernia in your baby, make an appointment with the surgeons of the SM-Doctor clinic. Our specialists will conduct a thorough diagnosis and prescribe effective and most gentle treatment in accordance with the indications.
Surgery without hospitalization...
Up to 80% of all operations for surgical diseases in children can be performed in a one-day hospital setting. The specialists of the CELT Children's One-Day Hospital came to this opinion a long time ago—one of the first in our country. The advantages of a one-day hospital are obvious: reducing the waiting time for surgery, eliminating the psycho-emotional trauma of the child from separation from parents and maintaining the usual biorhythm during postoperative rehabilitation, reducing treatment costs due to the elimination of costs for a long hospital stay and paying for additional staff, eliminating the risk of intra-hospital infections. This primarily applies to diseases such as hernia. In the postoperative period, children do not require medical care, observation, regimen or diet. Rehabilitation at home is much faster and easier. The use of medications at home is limited to a single dose of an analgesic tablet on the first day.
Intervertebral hernia in children and adolescents - how to detect an intervertebral hernia?
Spinal diseases, including intervertebral hernias, are unfortunately not such a rare phenomenon.
These diseases greatly reduce the child’s quality of life and affect his overall well-being, performance and learning. The degree of severity of organic lesions in intervertebral hernias can be completely different - accordingly, the nature of the pain and loss of ability to work can also be very different - from mild health problems and periodic pain to severe damage to the spine, severe pain and complete loss of the child’s ability to move.
Using an adhesive patch
This remedy can be used for newborns as soon as their umbilical wound has healed. The patch is glued so that a small fold is formed. The course of wearing the patch is 10 days. Typically, three courses are required with breaks in order to completely eliminate a hernia in an infant. The patch must be selected from a hypoallergenic material that allows air to pass through, so as not to irritate the baby’s sensitive skin. To ensure that the treatment of the disease is as effective as possible, it is recommended to combine the use of the patch with other methods. In this case, the result is more stable.
How can you tell if your child has an inguinal hernia?
A hernia appears as a round or oval bulge that is noticeable when the child is standing, sitting, or lying on his side, but may not be noticeable when he is lying on his back. It becomes more distinct if the baby cries, screams, coughs, sneezes, strains, and if he is already walking, when walking. Boys may experience asymmetry of the scrotum, while girls may experience asymmetry of the labia. As a rule, the place of protrusion is painless - pain may indicate infringement and require immediate medical attention. Repeated vomiting is also an alarming symptom. The risk of strangulation is especially high in the first three months of a baby’s life (about 30%) and decreases with age.
At the appointment, the pediatric surgeon conducts a more thorough visual examination and palpation of the protrusion site. In some cases, additional studies are necessary: ultrasound or x-ray.
According to the preschool plan, a child should be examined at the ages of 1 month, 12 months, 3 years and 6 years. However, if you notice a characteristic bulge, you need to contact a surgeon at the clinic as soon as possible, without waiting for the next scheduled examination.
Publications in the media
Regarding the treatment of this disease, you can contact the Surgical Department No. 1 of the Clinic of Faculty Surgery named after. N.N. Burdenko
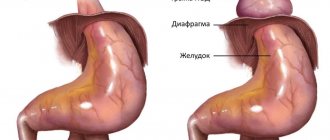
A congenital abdominal hernia occurs when the abdominal wall or diaphragm is underdeveloped • Congenital hernia is an anatomical concept. Its first manifestations can occur not only in early childhood, but also in adults (especially with a congenital inguinal hernia). This is explained by the fact that a weak spot in the abdominal wall becomes a hernial orifice only under the influence of a provoking factor - an increase in intra-abdominal pressure, often caused by heavy lifting, persistent cough, frequent anxiety (crying) or straining with chronic constipation or difficulty urinating • This group includes congenital inguinal and diaphragmatic hernias.
Congenital inguinal hernias in children are exclusively oblique. The viscera with them enter the inguinal canal outward from the lateral inguinal fold and pass obliquely through the inguinal canal.
• Frequency - 1-3% of children. In 35% of patients, the diagnosis is made before the age of 6 months •• Right-sided localization is 60% of cases, left-sided - about 30%, in 10-15% of cases the hernia is bilateral •• In boys it is registered 6 times more often •• In premature infants the incidence 1.5–2 times higher.
• Etiology: protrusion of internal organs into the lumen of the unopened processus vaginalis of the peritoneum (by the time of birth it is obliterated in 75% of newborns) •• Processus vaginalis of the peritoneum is a protrusion of the parietal peritoneum in the form of a blind sac descending into the scrotum, where the testicle moves from its original location in the lumbar areas •• Similar phenomena are observed in the female fetus. But normally the ovary remains in the pelvis. The inguinal canal in girls is much narrower and contains the round uterine ligament. The protruding vaginal process of the peritoneum closes. However, it may remain open after birth in the form of the so-called Nukki canal.
• Clinical picture •• History and physical examination ••• Round formation or swelling in the groin, scrotum or labia ••• Appears during an increase in intra-abdominal pressure (with screaming or straining) ••• Usually disappears after a decrease in intra-abdominal pressure, but in most cases, it easily recurs ••• Even if there is no hernial protrusion at the time of examination, in boys a compaction of the spermatic cord is found - a sign of an unstretched hernial sac (silk glove sign) •• Surgical findings in men ••• The hernial sac is covered with fascia of the levator muscle testicle ••• The tunica vaginalis of the testicle is absent ••• The testicle protrudes into the lumen of the hernial sac and is visible after opening the latter.
• Differential diagnosis •• Hydrocele of the testicle or spermatic cord: the tumor does not retract into the abdominal cavity and does not change its size when straining, gives a dull sound when percussed. It should be remembered that when hydrocele of the testicle communicates with the abdominal cavity, the tumor is reduced •• Inflammation of the inguinal lymph nodes: the formations are dense, limited from the external opening of the inguinal canal, and do not change when straining. Inguinal lymphadenitis is very painful, hot to the touch, the skin over it is swollen and reddish in color.
• Treatment is surgical. Even in the absence of a palpable hernia, but with a typical history, surgical intervention is usually performed. In children, hernia repair is used without opening the inguinal canal according to Roux-Krasnobaev. Stages of the operation: •• Isolation of the hernial sac •• Dissection of the hernial sac and revision of its contents. Reduction of the latter into the abdominal cavity •• Separation of the spermatic cord and testicle along with the peritoneum of the hernial sac covering them •• Applying a purse-string suture to the neck of the hernial sac (care must be taken not to damage the spermatic cord) •• Excision of the rest of the hernial sac •• Anterior plastic surgery the walls of the inguinal canal ••• First, the legs of the external inguinal ring are captured in the suture so that it has a sufficient opening for the passage of the spermatic cord ••• Then the formed fold of the aponeurosis of the external oblique abdominal muscle is strengthened with another 2-3 silk sutures.
Strangulated congenital inguinal hernia
• In boys, a strangulated hernia usually contains an intestinal loop •• There is a high probability of developing obstruction and ischemia of the intestine with necrosis of its wall •• Edematous strangulated intestine compresses the vessels of the spermatic cord, which leads to ischemia of the testicles with their necrosis and atrophy.
• In girls, as a rule, strangulation of the ovary occurs.
• Clinical picture •• Incarceration often occurs for no apparent reason or after some minor reason (coughing attack, straining during defecation) •• The child screams, complaining of pain in the hernia area, and sometimes throughout the abdomen •• The hernial swelling becomes dense, tense, very sensitive to palpation and irreducible •• Nausea and vomiting soon occur •• There may be an urge to defecate.
• Treatment •• Conservative ••• In children in the first months of life or with severe somatic pathology in the early stages (up to 12 hours), the following measures are indicated: warm bath - IM 1% trimeperidine solution and 0.1% solution atropine - position with a raised pelvic end ••• Forced attempts at reduction are unacceptable ••• If conservative treatment is ineffective within 2-3 hours, surgery is indicated •• Surgical. Stages of the operation: ••• Isolation and opening of the hernial sac ••• Fixation of the strangulated organ ••• Dissection of the strangulated ring. In case of an indirect inguinal hernia, it is unacceptable to dissect the ring downwards (danger of injury to the femoral vessels) and medially (danger of damage to the lower epigastric vessels) ••• Assessment of the viability of the strangulated organ with its subsequent removal or reduction ••• Plastic surgery of the anterior wall of the inguinal canal.
Congenital diaphragmatic hernias are caused by the presence of holes in the diaphragm, allowing the contents of the abdominal cavity to penetrate into the chest.
• Frequency - 1 in 1,700 births.
• Classification •• By localization of congenital defects of the diaphragm ••• Hernia of the dome of the diaphragm (66% of cases) ••• Hernia of the esophageal opening of the diaphragm (19%) ••• Hernia in the anterior part of the diaphragm (15%) •• Depending on the presence of a hernia sac ••• True (there is a hernial sac) ••• False (there is no hernial sac, the abdominal organs are in direct contact with the pleura).
• Clinical picture •• Soon after birth, cyanosis may occur, which differs from cardiac cyanosis in that it is intermittent in the form of attacks associated with eating or crying •• If the stomach is displaced into the pleural cavity and stretched by liquid and gases, then, in addition to shortness of breath, cyanosis and increased heart rate, coughing, vomiting and difficulty swallowing also occur •• On the affected side, respiratory sounds are weakened (or absent) •• Percussion is used to determine the displacement of the heart to the side opposite the hole in the diaphragm •• In the affected half of the chest, peristaltic noises are heard •• Due to the migration of contents into the chest cavity, the abdomen acquires a scaphoid shape •• When a diaphragmatic hernia is strangulated, intestinal obstruction develops, not accompanied by bloating •• Hiatal hernias in older children are characterized by the development of anemia: gastric bleeding occurs due to ulceration of the esophagus and stomach, which are constantly injured in the area of the hernial orifice •• Anterior hernias of the diaphragm are mostly detected only with age. The leading symptom is abdominal pain due to partial strangulation of displaced intestinal loops.
• Method of examination - X-ray of the chest while lying down and in an upright position of the body •• Gas bubbles with fluid levels (stomach or intestinal loops) in the affected half of the chest •• Displacement of the mediastinal organs to the side opposite to the affected side •• Collapse of the lung on the affected side • • After insertion of a nasogastric tube through the esophagus, it is found in the affected side of the chest.
• Treatment •• Indications for surgery ••• In case of severe breathing problems, children with large hernias of the diaphragm should be operated on in the first days of life ••• For hiatal hernias, surgery can be delayed until the age of 1 year ••• Emergency surgery is indicated for strangulated hernia and bleeding from the stomach •• Surgical treatment. Stages of the operation: ••• Transperitoneal access ••• Reduction of the hernia into the abdominal cavity ••• Closing the hernial orifice (plasty or alloplasty for large defects) ••• Revision of the abdominal organs to identify associated congenital anomalies (diaphragmatic hernia is often accompanied by incomplete intestinal rotation ) ••• Drainage of the affected half of the chest.
• The results of surgery in newborns with diaphragmatic hernias depend on the timing of their detection and the severity of clinical manifestations •• Mortality in the preoperative period reaches 50% •• Postoperative mortality - 12–20%. The cause of death in newborns and infants is most often pulmonary failure ••• With diaphragmatic hernias, the lung on the affected side is often hypoplastic due to compression by the hernia during intrauterine development ••• Relief of respiratory failure in the postoperative period depends on the compensatory capabilities of the healthy lung ••• If the outcome of the operation is favorable, a hypoplastic lung may develop with age.
ICD-10 • Q40.1 Congenital hiatal hernia • Q79.0 Congenital diaphragmatic hernia
Rehabilitation after surgery
Recovery after surgery varies. Children recover the fastest after laparoscopy. Since this method is the most gentle of all, rehabilitation here takes 2-3 days maximum. Most often, babies are discharged within a day after such an operation.
Now we’ll tell you how a child feels after an umbilical hernia operation performed in other ways. If the surgical intervention was planned and timely, then the rehabilitation period takes no more than 14 days. This means that the child was operated on while still in preschool age. In this case, there should be no complications. The doctor will prescribe the wearing of a postoperative bandage, as well as the diet necessary for the little patient. You will not be able to eat foods that can cause gas in the intestines for some time. Physical activity will also need to be temporarily reduced.
The rehabilitation process takes the longest for those children who were urgently hospitalized. If the operation was unplanned, the hernia was strangulated or the hernia sac ruptured, then a longer recovery will be required. Usually, a course of medications and physical therapy are also prescribed.
What leads to the formation of intervertebral hernias in children and adolescents?
- Injuries, blows to the spine, falls.
- Strength sports, excessive stress on the spine.
- Insufficient development of the child’s muscle corset, skeletal bones and connective tissue.
- Strong flexion and twisting of the spine in games or sports - for example, in gymnastics, somersaults, etc.
- Weakness of the body due to poor nutrition, sedentary lifestyle, environmental factors, and previous illnesses.
- Anatomical and genetic factors.
- Underweight or overweight.