Losartan blocks the action of a natural substance in the body that causes constriction of the blood vessels of the heart, which leads to vasodilation, lowering blood pressure and reducing the load on the heart. The drug is incompatible with alcohol due to the strong effect of alcohol on the cardiovascular system.
Drinking alcohol first dilates blood vessels, thereby enhancing the effect of the drug, and then leads to their sharp narrowing (spasm). Combining Losartan tablets is dangerous due to consequences in the form of life-threatening side effects.
Release form of the drug Losartan
The drug Losartan is available in the form of tablets with different contents of the active substance. The tablets are white, round in shape. When cut, the contents are also white. A slight color deviation towards a yellow tint is acceptable.
The main active ingredient is losartan potassium. Additional components include:
- lactose monohydrate;
- pregelatinized starch;
- microcrystalline cellulose;
- Magnesium stearate.
Tablets are produced with different contents of active substance per unit of drug:
- 25mg;
- 50mg;
- 100 mg.
The difference in the concentration of the substance is needed to accurately select the dosage necessary to achieve a therapeutic effect in each specific case.
Losartan: what is it taken for?
Indications for the use of Losartan are:
- Nephropathy of the diabetic type, including damage to the tubules and glomeruli of the kidneys, as well as arterioles and arteries, developing due to disruption of metabolic processes in the renal tissue.
- Presence of a tendency to develop disorders of the cardiovascular system, including strokes.
- Arterial hypertension, in which the indicator exceeds 140 mm Hg. Art.
- Chronic heart failure, in which the circulatory system does not properly supply the body with oxygen either at rest or after exercise.
After entering the gastrointestinal tract, the drug is actively absorbed. As a result of filtration by the liver, a metabolite is formed that is many times more active than Losartan in its original form. The maximum concentration of Losartan in the blood is observed after 1 hour, and the metabolite - after 3-4 hours. About 98% of the drug actively binds to plasma proteins.
The half-life of Losartan is 2-2.5 hours, and the active metabolite is up to 9 hours, depending on the speed of metabolic processes in the body. The drug and its derivatives are excreted unchanged in feces, urine and bile. Most of the medicine comes out through the rectum.
Losartan: instructions for use
Eating does not affect the absorption and activity of the drug. The drug is swallowed whole with a sufficient amount of water. Depending on the diagnosis, a different therapeutic dose may be prescribed:
- Arterial hypertension is treated with a single dose of 50 mg of Losartan. If there is no desired effect, the single dose can be increased to 100 mg per day.
- For chronic heart failure, treatment begins with a single dose of half a tablet containing 25 mg of the active substance. After a week, the daily dose is gradually increased.
- The risk of developing problems in the functioning of the cardiovascular system is reduced by a single dose of 50 mg of Losartan or a two-time dose of 25 mg.
- Liver failure becomes a reason to prescribe 25 mg of the active substance.
Throughout the course of treatment, regardless of the diagnosis, it is necessary to monitor the patient’s blood pressure daily. If the patient takes the course at home, he must keep a diary of tonometer readings after each measurement.
If an excessive decrease in blood pressure is noted, the doctor is required to adjust the daily dose. In addition, the patient must comply with the time of taking the drug. In order to reduce the risk of overdose, the tablet is taken strictly at the same time. If one dose is missed, the next dose is taken at the allotted hour.
Losartan
Mechanism of action
Angiotensin II is a powerful vasoconstrictor, the main active hormone of the renin-angiotensin-aldosterone system (RAAS), as well as a decisive pathophysiological link in the development of arterial hypertension (AH). Angiotensin II binds to AT1 receptors found in many tissues (vascular smooth muscle, adrenal glands, kidneys and heart) and performs several important biological functions, including vasoconstriction and aldosterone release. In addition, angiotensin II stimulates the proliferation of smooth muscle cells. AT2 receptors are the second type of receptor to which angiotensin II binds, but its role in regulating cardiovascular function is unknown.
Losartan is a selective antagonist of angiotensin II AT1 receptors, highly effective when taken orally. Losartan and its pharmacologically active carboxylated metabolite (E-3174), both in vitro and in vivo, block all physiological effects of angiotensin II, regardless of its source or route of synthesis. Unlike some peptide angiotensin II antagonists, losartan does not have agonist properties.
Losartan selectively binds to AT1 receptors and does not bind to or block receptors of other hormones and ion channels that play an important role in regulating the function of the cardiovascular system. In addition, losartan does not inhibit angiotensin-converting enzyme (ACE, kininase II), which is responsible for the destruction of bradykinin. Therefore, effects not directly related to AT1 receptor blockade, such as increased bradykinin-mediated effects or the development of edema (losartan 1.7%, placebo 1.9%), are not related to the action of losartan.
Losartan suppresses the increase in systolic and diastolic blood pressure (BP) during angiotensin II infusion. At the moment of reaching the maximum concentration of losartan in the blood plasma (Cmax) after taking losartan at a dose of 100 mg, the above effect of angiotensin II is suppressed by approximately 85%, and 24 hours after single and multiple doses - by 26-39%.
During the period of taking losartan, elimination of the negative feedback, which consists in the suppression of renin secretion by angiotensin II, leads to an increase in plasma renin activity (PRA). An increase in ARP leads to an increase in the concentration of angiotensin II in the blood plasma. With long-term (6-week) treatment of patients with hypertension with losartan at a dose of 100 mg/day, a 2-3-fold increase in the concentration of angiotensin II in the blood plasma was observed at the time the losartan Cmax was reached. Some patients experienced an even greater increase in angiotensin II concentrations. especially with a short duration of treatment (2 weeks). Despite this, during treatment, an antihypertensive effect and a decrease in plasma aldosterone concentrations appeared after 2 and 6 weeks of therapy, indicating effective blockade of angiotensin II receptors. After discontinuation of losartan, ARP and angiotensin II concentrations decreased within 3 days to the values observed before the start of losartan administration. Since losartan is a specific antagonist of angiotensin II AT1 receptors, it does not inhibit ACE (kininase II), an enzyme that inactivates bradykinin. A study comparing the effects of losartan at doses of 20 mg and 100 mg with the effects of an ACE inhibitor on angiotensin I, angiotensin II and bradykinin showed that losartan blocked the effects of angiotensin I and angiotensin II without affecting the effects of bradykinin. This is due to the specific mechanism of action of losartan. The ACE inhibitor blocked responses to angiotensin I and increased the severity of the effects due to the action of bradykinin, without affecting the severity of the response to angiotensin II. which demonstrates the pharmacodynamic difference between losartan and ACE inhibitors. Plasma concentrations of losartan and its active metabolite, as well as the antihypertensive effect of losartan, increase with increasing dose of the drug. Since losartan and its active metabolite are angiotensin II receptor antagonists (ARA II), they both contribute to the antihypertensive effect.
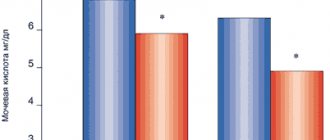
In a study with a single dose of 100 mg of losartan, which included healthy volunteers (men), oral administration of the drug under high- and low-salt diets did not affect the glomerular filtration rate (GFR), effective renal plasma flow and filtration fraction. Losartan had a natriuretic effect that was more pronounced with a low-salt diet and did not appear to be associated with suppression of early sodium reabsorption in the proximal renal tubules. Losartan also caused a transient increase in renal excretion of uric acid.
In patients with hypertension, proteinuria (at least 2 g/24 hours), without diabetes mellitus and taking losartan for 8 weeks at a dose of 50 mg with a gradual increase to 100 mg, a significant decrease in proteinuria (by 42%) and fractional excretion of albumin was observed and immunoglobulins (lgG). In these patients, losartan stabilized GFR and reduced the filtration fraction.
In postmenopausal women with hypertension who took losartan at a dose of 50 mg for 4 weeks, there was no effect of therapy on the renal and systemic levels of prostaglandins.
Losartan does not affect autonomic reflexes and does not have a long-term effect on the concentration of norepinephrine in the blood plasma.
In patients with hypertension, losartan in doses up to 150 mg/day did not cause clinically significant changes in the concentration of fasting triglycerides, total cholesterol and high-density lipoprotein cholesterol. At the same doses, losartan had no effect on fasting blood glucose concentrations.
The HEAAL clinical trial to evaluate the effect of high and low doses of ARB II (losartan) on the outcome of treatment in patients with chronic heart failure (CHF) included patients (n=3834) with CHF (II-IV functional class according to the NYHA classification) and intolerance to inhibitors APF. Patients were followed for more than 4 years (median follow-up 4.7 years) to compare the effects of losartan 50 mg/day and 150 mg/day on reducing all-cause mortality or hospitalization for heart failure. This study showed that losartan 150 mg/day significantly reduced the risk of all-cause mortality or hospitalization for heart failure compared with losartan 50 mg/day (hazard ratio [HR] 0.899, P = 0.027).
In general, losartan caused a decrease in serum uric acid concentrations (usually less than 0.4 mg/dL) that persisted during long-term treatment. In controlled clinical studies involving patients with hypertension, no cases of drug withdrawal due to an increase in creatinine concentration or serum potassium levels were recorded.
A 12-week parallel study, which included patients with left ventricular failure (NYHA functional class II-IV), most of whom were taking diuretics and/or cardiac glycosides, compared the effects of losartan at doses of 2.5, 10, 25 and 50 mg/day with placebo. At doses of 25 and 50 mg/day, the drug exhibited positive hemodynamic and neurohormonal effects, which persisted throughout the study. Hemodynamic effects included an increase in cardiac index and a decrease in pulmonary capillary wedge pressure, as well as a decrease in total peripheral vascular resistance, mean systemic blood pressure, and heart rate. The incidence of arterial hypotension in these patients depended on the dose of the drug. Neurohormonal effects included decreased concentrations of aldosterone and norepinephrine in the blood.
Concomitant use with other drugs
Concomitant use with ACE inhibitors leads to the development of such a dangerous condition as hyperkalemia, in which the level of potassium in the blood increases. In addition, this combination increases the risk of kidney failure and life-threatening low blood pressure.
In combination with diuretics, the risk of hypotension is also high. This is due to the fact that taking diuretics itself leads to a decrease in blood pressure, which enhances the effect of Losartan.
It is not recommended to drink Losartan with lithium-containing drugs, so as not to provoke an excess of lithium in the blood, since the combination of drugs disrupts natural metabolic processes.
Side effects and consequences
To reduce the risk of side effects, you should stop drinking alcohol during the period of treatment and carefully follow the warnings of doctors and the manufacturer (instructions for the drug).
Losartan should not be taken if there are contraindications:
- Allergy to the components of the drug.
- Individual intolerance to the active substance or auxiliary components.
- Low blood pressure (blood pressure may drop too much).
- Chronic gastritis.
- Acute form of heart failure.
- Children's age up to 18 children.
- Dehydrated state of the body (including from exposure to alcohol).
- During pregnancy and breastfeeding.
The drug has a relatively low likelihood of side effects. Symptoms are relatively mild, so symptomatic therapy or discontinuation/adjustment of the dosage of the drug is usually not required. The most dangerous symptoms occur in case of drug overdose: a sharp and severe decrease in blood pressure, bachycardia and brachycardia (decrease in heart rate to 30-40 beats per minute).
In rare cases (less than 1% of patients), the following side effects are possible:
- Feeling of dry mouth, nausea and vomiting.
- Functional gastrointestinal disorders (diarrhea or diarrhea).
- Deterioration of potency, disruption of the normal functioning of the liver and kidneys.
- Upper respiratory tract infections, bronchitis and rhenitis with symptoms corresponding to the disease.
- Pain in the back, shoulders and lower extremities; exacerbation of arthritis.
- Increased sweating.
- Increased fatigue, chronic fatigue syndrome, sleep disorders.
- Headaches and dizziness.
All these side effects, with some probability, can also occur in a person who fully complies with the recommendations of doctors and does not drink alcohol. Drinking alcohol causes a serious blow to health and increases the likelihood of negative consequences.
Consequences of combining Losartan tablets with alcohol:
- A sharp decrease in pressure. Alcohol dilates blood vessels, thereby causing a decrease in blood pressure for some time. If you have blood pressure-lowering drugs in your body, your blood pressure may drop too much and your heart rate may slow down dangerously.
- A double blow to the gastrointestinal tract and organs. The liver, kidneys and gastrointestinal tract react negatively to both alcohol and most medications. Alcohol abuse puts a strain on the kidneys and liver, increasing the likelihood of side effects and pathological processes.
- Symptoms of incompatibility. Symptoms can appear suddenly after drinking even a small amount of alcohol: nausea, dizziness, sudden weakness, cold extremities, loss of coordination and orientation in space.
To avoid negative consequences, do not combine alcohol with medications, spacing out taking pills and alcohol as much as possible over time. It is advisable to consult a doctor regarding the possibility of drinking alcohol for health reasons. It should be remembered that other medications taken may be incompatible with alcohol and may also change the effect of other medications.