Tonsilgon belongs to the group of herbal preparations with complex effects. The medicine is produced in the form of drops. It is a clear, yellow-brown liquid with a chamomile aroma. A small amount of sediment may appear during storage of the product. The drug is packaged in 50 mg and 100 mg bottles, equipped with a convenient drip dosing device.
Features of the composition of the drug
The drug can be purchased for the prevention and treatment of acute respiratory viral infections in children and adults. The product reduces pain and soreness in the scalp, which improves your well-being. In addition, the product improves immunity, which speeds up the healing process.
The composition of the drug is represented exclusively by herbal components. This:
- Marshmallow roots. They have an enveloping, softening, expectorant and anti-inflammatory effect. The plant covers the mucous membranes with a thin layer and remains on their surfaces for a long time, which allows to stop inflammation and accelerate tissue regeneration
- Chamomile flowers. They are distinguished by anti-inflammatory, disinfectant, and analgesic properties. The antibacterial effect of the medicinal plant is important in the composition of the drug.
- Horsetail grass. A characteristic feature of the component is its targeted anti-inflammatory effect in diseases of the oral cavity. In addition, the medicinal plant relieves swelling and restores breathing.
- Walnut leaves. And they normalize immunity, reduce the severity of cold symptoms, lower body temperature and increase the effectiveness of treatment of ARVI. In addition, the component has a mild analgesic effect.
- Yarrow herb. It contains a large amount of vitamin C and P. Combinations of various biologically active substances provide bactericidal, healing and anti-inflammatory effects.
- Oak bark. The tannins contained in the component have a protective effect against external irritants. This allows for faster tissue healing.
- Dandelion grass. This medicinal plant has a rich vitamin and mineral composition. When used, it is possible to enhance the body's natural defense reactions.
Tonsilgon drops, which are affordable, are distinguished by their ability to suppress the activity of harmful bacteria and viruses. When used, it is possible to stop inflammation.
They have an immunomodulatory effect. The combination of biologically active substances of plant origin reduces allergy symptoms, weakens cough, reduces swelling of the mucous membranes and makes breathing easier. In addition, the medicine has an antioxidant effect.
Tonsilgon N
Tonsilgon N is a disinfecting multicomponent herbal medicine. Shows anti-inflammatory and disinfecting effects. The drug exhibits immunomodulatory properties due to its complex composition, which includes a number of immunotropic plant components. Biologically active substances of marshmallow root exhibit antioxidant, antimicrobial and anti-inflammatory effects, reduce the intensity and frequency of cough caused by irritation of the mucous membrane of the pharynx, larynx, and trachea. Dandelion herb is a natural immunomodulator. Chamomile flowers are effective for inflammation, allergies, muscle spasms, bacterial and viral infections, as an antioxidant, wound healing and anti-ulcer agent. Horsetail herb has antibacterial, immunomodulating and anti-inflammatory effects. Walnut leaves exhibit antimicrobial, tonic, anti-inflammatory effects. Yarrow herb has a whole range of beneficial properties: it prevents blood loss, reduces inflammation, prevents the growth and development of pathogenic bacteria, relieves muscle spasms, suppresses allergies, and promotes the healing of ulcers. Oak bark has an antibacterial, anti-inflammatory, decongestant, and astringent effect. Tonsilgon N is indicated for inflammation of the mucous membrane of the tonsils, pharynx, larynx and other diseases of the upper respiratory tract of inflammatory origin, which are acute or chronic. The drug is also used as a means of preventing acute respiratory infections and as an adjuvant in antibacterial therapy.
In pediatric practice it is used starting from the age of one. Do not use if you have an individual intolerance to one or more herbal components. The drug has a favorable safety profile and is well tolerated by patients. In rare cases, individual intolerance reactions occur - allergies, nausea, vomiting. In such situations, drug therapy should be interrupted. Tonsilgon N combines well with antibacterial drugs without interacting with them pharmacologically. If, when using Tonsilgon N, there is no improvement in the patient’s condition within a week, then it is necessary to consult a doctor. The drug is successfully used in pediatric practice, especially in patients with rhinovirus infection, inflammation of the mucous membrane of the tonsils and pharynx of acute and chronic origin. In the treatment of these diseases, the drug exhibits an immunotropic effect, stimulating the ability of phagocytes to capture, kill and digest pathogenic and opportunistic microorganisms. In children who often catch colds, when using Tonsilgon N, an increase in the level of immunoglobulins A and M in the blood is observed. The advantages of the drug include its herbal nature (which means minimal risk of side effects), good compatibility with antibacterial drugs, reducing the risk of recurrence of diseases of the oral cavity and pharynx of chronic nature, pronounced immunotropism, confirmed effectiveness in clinical studies, possibility of use in young children.
Indications and contraindications
Tonsilgon drops, the instructions for use focus on this, are prescribed for the treatment of children and adults. It increases the effectiveness of acute and chronic ARVI therapy.
In addition, the medicine can be used as a prophylactic agent to reduce the risk of complications of diseases caused by viruses. The drug increases the effectiveness of antibacterial therapy for various diseases caused by pathogenic bacteria. It increases the body's resistance to infectious pathologies.
Tonsilgon has serious contraindications, so its use should be agreed with a doctor if indicated. It is prohibited to use the medicine if you are hypersensitive to any component in the composition. The drug is not prescribed for the treatment of children under one year of age.
Treatment with Tonsilgon drops is carried out with caution when liver dysfunction is confirmed in patients, as well as in cases of traumatic brain injury. The drug is not recommended for the treatment of people with alcohol dependence or after undergoing treatment aimed at getting rid of addiction.
The pharyngeal tonsil, like other formations of the lymphopharyngeal ring, is one of the structurally formed accumulations of the so-called “mucosa associated lymphoid tissue (MALT)” and takes part in the mechanisms of immune defense. Together with nonspecific protective factors (mucociliary transport, production of lysozyme, interferon, etc.), it performs a barrier function, regulates the production of secretory immunoglobulin A and, as a result of lymphocytopoiesis, supplies lymphocytes to the mucous membranes of the upper respiratory tract (1).
Chronic inflammation of the pharyngeal tonsil (chronic adenoiditis - CA) is a multifactorial immunopathological process, the trigger of which is a viral infection (often with activation of bacterial agents persistent in the nasopharynx), developing against the background of predisposing factors, such as hereditary predisposition, crowding in children's groups, secondary immunodeficiencies states [2-4].
The prevalence of chronic adenoiditis, according to data from referrals and preventive examinations, ranges from 5.2 to 33.9 per 1000 people [5, 6], and hypertrophy of the pharyngeal tonsil has a maximum prevalence in the age group of 3-7 years [7-9] and is detected in 37 -76% of children [5, 10-12]. According to the results of preventive examinations of children in Novokuznetsk, 18.0±0.9% of children under the age of 3 years and 9.2±0.5% of children aged 3-7 years are sick with CA [13]. CA in 65.4% of cases is accompanied by diseases of the paranasal sinuses and in 76% by exudative otitis media.
To increase the effectiveness of treatment for CA, taking into account all the features of its pathogenesis, standard treatment protocols use herbal preparations that have anti-inflammatory and immunomodulatory properties.
Tonsilgon N (Bionorica, Germany) is a classic herbal medicine for the treatment and prevention of inflammatory diseases of the lymphoid apparatus of the pharynx, especially in frequently ill children. It has anti-inflammatory, antiseptic, immunomodulatory, antibacterial and enveloping effects. This variety of properties is due to the plant components included in the preparation: marshmallow root, chamomile flowers, horsetail herb, walnut leaves, yarrow herb, oak bark, dandelion herb. The active components included in chamomile, marshmallow and horsetail help to increase the body's nonspecific defense factors by increasing the phagocytic activity of macrophages and granulocytes. Polysaccharides, essential oils and flavonoids of chamomile, marshmallow, yarrow and oak tannins have an anti-inflammatory effect and reduce swelling of the mucous membrane of the respiratory tract. Oak and walnut tannins have an astringent effect and have antiviral activity.
The drug is available in the form of pills and drops, is well tolerated, can be combined with antibiotics and can be prescribed to children over 1 year of age. There are separate immunological studies indicating that after taking it, some indicators of systemic immunity significantly improve in people with acute respiratory infections and chronic diseases of the pharynx. In the studies of O.F. Melnikova and O.G. Rylskaya studied the effect of the drug on cellular and humoral immunogenesis [14-15]. The purpose of the study was to evaluate the effect of the drug on the manifestations of the phenotypic and functional characteristics of the palatine tonsils of patients with chronic tonsillitis in vitro.
The material for the research was cells from the palatine tonsils of patients with chronic tonsillitis.
The effect of the drug on the relative content of cells with the CD4, CD25 and CD56 phenotype in cell culture of the palatine tonsils of patients with chronic tonsillitis has been proven [14]. in vitro
studies indicate the presence of immunostimulating properties in this herbal preparation, which are manifested both in relation to factors of innate (natural cytotoxic activity and phagocytosis) and acquired (stimulation of antibody genesis) immunity [15].
The purpose of the study was to evaluate the effectiveness of the use of the drug tonsilgon N in the complex treatment of children with exacerbation of chronic adenoiditis.
Patients and methods
The clinical open prospective controlled study involved 62 children (32 in the main group and 30 in the control group) aged from 3 to 11 years, admitted for treatment at the ENT department of the Regional Perinatal Center for day hospital treatment with a diagnosis of exacerbation chronic adenoiditis."
Inclusion criteria: verified diagnosis of chronic adenoiditis, age from 3 to 11 years.
Exclusion criteria: age younger than 3 and older than 11 years, taking other mucoactive or immunocorrective drugs.
The parents of all children gave written informed consent to the study. The distribution of children by age is presented in table. 1.
The examination included: medical history, general examination, thermometry, rhino-, pharyngo- and otoscopy, if necessary, X-ray examination of the paranasal sinuses in direct and lateral projection, general clinical examination.
The complex of therapeutic measures included:
- systemic antibacterial therapy using β-lactam antibiotics (amoxicillin
50 mg/kg/day, course 5-7 days);
- rinsing the nasopharynx using the Proetz method, followed by the use of antiseptics or topical antibiotics;
— decongestants for a short course;
— physical therapy (microwaves, laser No. 7).
Patients of the main group additionally received the drug Tonzilgon-N: preschool children 10 drops 3 times a day, schoolchildren 15 drops 3 times a day for 14 days.
The assessment of clinical manifestations was carried out by a doctor on the 3rd, 5th, 7th and 9th days of treatment according to the scoring system we proposed (from 1 to 5 points) for the following symptoms.
1. Difficulty in nasal breathing during the day: 0 - normal breathing, 1 - slight intermittent difficulty, 2 - slight constant difficulty, 3 - severe difficulty less than 4 hours a day, 4 - severe difficulty more than 4 hours a day, 5 - absence of nasal breathing.
2. Intensity and nature of rhinorrhea: 0 - no discharge, 1 - a small amount of mucous discharge, 2 - moderate mucous discharge, 3 - abundant mucous discharge, 4 - purulent mucous discharge, 5 - abundant purulent discharge.
3. The degree of difficulty in nasal breathing at night: 0 - normal breathing at night, 1 - slight occasional snoring, 2 - slight constant difficulty, 3 - snoring, 4 - severe difficulty, snoring, 5 - lack of breathing at night.
Statistical analysis of the obtained data was carried out using parametric and nonparametric statistics methods using the Statistica v software package. 6.0, SPSS 11.0, INSTAT 2.0. The normality of distribution of quantitative characteristics was checked using histograms, the Kolmogorov-Smirnov test with the Lilliefors correction and the Shapiro-Wilk test, and the homogeneity (homogeneity) of variance was checked using Levene’s test. To test statistical hypotheses about differences in absolute and relative frequencies and ratios in two independent samples, the &khgr;2 test with Yates' correction and Fisher's exact test were used. For quantitative traits, intergroup differences were assessed using the Kruskal-Wallis test. Paired intergroup comparisons of indicators were made using the Mann-Whitney U test. The relative significance level (p) was calculated, with the critical significance level taken equal to 0.05.
Results and discussion
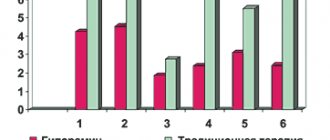
Assessment of the degree of difficulty in nasal breathing during the day (Fig. 1)
Figure 1. The degree of difficulty in nasal breathing during the day in the main and control groups during treatment. in both groups made it possible to establish that, with initially the same level of congestion, nasal breathing in the main group of children on the 5th day of treatment was 15% better than in the control group, on the 7th day - by 30%, and on the 9th day - by 73%.
The nature and dynamics of intensity of rhinorrhea also had their own characteristics (Table 2).
In the main group of children, upon admission to the department, 2 (6.25±2.47%) children had a purulent runny nose, 10 (31.25±5.3%) had a mucopurulent runny nose, 4 (12) each had heavy and moderate mucous discharge. .5±3.46%) children, a small amount of mucous discharge - 3 (9.38±3.02%) and no discharge in 9 (28.15±5.06%) children. In the control group, the percentage did not differ significantly and was 3.33±1.82, 33.33±5.48, 13.33±3.58, 10±3.11, 10±3.11 and 30±, respectively. 5.22%. On the 3rd day of treatment, the intensity of discharge decreased in children of both groups, although there were no significant differences. However, on the 5th day of treatment, there was no discharge in 15 (48.85%) children of the main group and in 10 (35.07%) of the control group (p = 0.04). On the 7th day, the percentage increased to 62.5% in the main group and to 53.33% in the control group (p=0.04). On the 9th day, 29 (90.63%) children receiving the herbal preparation had no discharge, while among children receiving standard therapy, this figure was only 25 (76.67%) (p = 0. 01). Abundant purulent and purulent-mucosal discharge ceased in both groups on the 5th day of treatment. At the same time, on the 5th day, moderate mucous discharge was diagnosed in 5 (15.63%) children of the main group and 7 (23.33%) of the control group, and on the 7th day these groups amounted to 4 (12.5%) and 5 (16.67%) children, respectively. Even on the 9th day of treatment, 10% of children in the control group still had moderate mucous discharge.
A small amount of mucous discharge was observed in 10-20% of children in the main group and in 16-26% of children in the control group on days 5-7 of treatment. On the 9th day, a small amount of discharge remained in 3 (9.3%) children of the main and 4 (13.3%) control groups (p = 0.05).
Thus, the intensity of rhinorrhea in the main group receiving the herbal preparation was relieved faster than in the control group.
Improvement in nasal breathing at night began already on the 5th day of treatment (Fig. 2).
Figure 2. The degree of difficulty in nasal breathing at night. However, the statistical significance of these differences appeared only on the 7th day, when the assessment of night breathing in the main group was 2.12 points, and in the control group - 2.8 points. On the 9th day of treatment, breathing at night in children of the main group was 1.4 times better than in children in the control group.
Conclusion
Treatment of children with CA was more successful in the group receiving tonsilgon N: the severity of rhinorrhea was relieved faster, nasal breathing became 73% better both at night and during the day. Thus, the study made it possible to establish that the inclusion of the drug Tonsilgon N in the treatment regimen for CA increases the effectiveness of therapy and accelerates the recovery process.
Use and adverse reactions
Tonsilgon drops are taken orally. There is no need to dilute them with water. The product should be kept in the mouth before swallowing. When the disease is acute, the recommended dosage for adults is 25 drops. The product should be taken 5-6 times a day.
For children of school and preschool age in the acute phase of the disease, 15 drops and 10 drops are recommended 5-6 times per day, respectively. After the pronounced symptoms of the disease have been relieved, children and adults should continue taking drops in the same dosage 3 times a day.
If contraindications are excluded, adverse negative reactions of the body while taking the drug rarely occur. The most common problems are in the gastrointestinal tract. They are manifested by nausea and vomiting.
Overdose of the drug has not been recorded in practice. But most likely it can increase negative side reactions to the drug. In such cases, symptomatic treatment is indicated.
Therapeutic tactics for tonsillitis
If we consider that chronic tonsillitis is only a long-term inflammatory process in the tonsils, then it is unlikely that this disease should have received so much attention from other medical specialties. Therefore, the very definition of tonsil disease as chronic tonsillitis requires clarification. This will make the motivation for different types of conservative or surgical treatment clearer. So, chronic tonsillitis is a process of constant interaction between lymphoid tissue and the contents of the lacunae of the palatine tonsils (purulent detritus with elements of foreign protein, toxins as a result of the vital activity of pathogenic flora, microorganisms themselves, dead epithelial cells from the walls of the lacunae of the palatine tonsils, nutritional particles). The discharge in the lacunae can be purulent, caseous, accumulate in narrow lacunae convoluted with spurs, and form so-called fetid plugs. This process, which takes place in the lacunae of the palatine tonsils, is under the control of the body until a certain time, i.e. There is constant active and passive drainage of tonsil lacunae along with the activity of macrophages, which, preventing inflammation of the palatine tonsil, contributes to the development of immunity to many microorganisms that enter the oral cavity and pharynx along with air and food.
This kind of balance between the vital activity of pathogenic active flora and the protective capabilities of the body can be disturbed for many reasons, as a result of which inflammation of varying intensity develops (it captures only the covering epithelium of the oral surface of the tonsils without its destruction), which passes to the epithelial cover of the lacunae of the tonsils with its destruction and formation necrotic plaques; suppuration of the tonsil follicles. Catarrhal, lacunar or follicular tonsillitis develops
.
In foreign literature, they tend to combine two diseases of the oropharynx and designate inflammation of the tonsils and pharyngeal mucosa as “tonsillopharyngitis.” However, experts in Russia quite reasonably believe that such a combination of two nosological units is possible only in cases of a combination of acute catarrhal pharyngitis and catarrhal tonsillitis. Lacunar and follicular tonsillitis have their own clearly defined clinical, morphological and microbiological aspects
, and they cannot be confused with manifestations of pharyngitis, especially from the point of view of the approach to treatment.
According to modern concepts, angina is an acute infectious-allergic disease, and it is necessary to approach the treatment of a patient with angina from this point of view.
As was said, the presence and persistent preservation of purulent detritus in the lacunae of the palatine tonsils is a determining factor both in making the diagnosis of “chronic tonsillitis” and in choosing the appropriate method of treatment - conservative or surgical.
A sore throat with destruction of the integumentary epithelium of the lacunae promotes the formation of scars in their lumen, which subsequently complicates the drainage of the lacunae of the tonsils. A kind of vicious circle arises - sore throat develops under the influence of pathogenic flora against the background of sensitization by a foreign protein due to a violation of the epithelial cover of the lacunae. Moreover, a sore throat can occur both under the influence of a pathogenic infection and as a result of nonspecific irritation (general hypothermia, drinking cold water).
Each previous angina, especially lacunar, follicular, can contribute to the development of conditions for relapse of inflammation, accompanied by otitis, sinusitis, and bronchitis.
The main reason for this is the viruses that cause most respiratory tract infections, which can weaken the body's defenses. Viruses reduce the ability of macrophages and granulocytes to absorb infectious agents. In this way, the epithelium of the mucous membrane is damaged, which impedes the activity of the epithelial villi and leads to stagnation of mucus. Weakening of local protective mechanisms in many cases leads to infection of the upper and lower respiratory tract with bacteria Haemophilus influenzae, Streptococcus pneumoniae and Staphilococcus aureus, which are usually found in the oral cavity and trachea.
The chronic nature of infections is an indicator that the body's immune system is unable to cope with its functions. Constant but insufficient activation of nonspecific defense mechanisms often causes an inflammatory response, but this is not enough to suppress infectious agents.
Undoubtedly, the nature of the pathogenic flora plays a big role in the occurrence of a particular sore throat,
but the background against which it occurs also influences the clinical picture of the disease. Therefore, therapy should be prescribed and carried out taking into account all identified features in each case (time from the onset of angina, age of the patient, frequency of exacerbations, concomitant diseases: general and from the ENT organs, clinical manifestations, including in the oropharynx, nature of the flora , previous treatment, its effectiveness).
Currently, much attention is paid to the role of group A streptococcus in the occurrence of acute tonsillitis and pharyngitis, although b-hemolytic streptococcus still occupies a leading position among bacterial pathogens. Thus, it is believed that in late autumn and spring it is group A streptococci that cause disease in 40% of children and 10% of adults. Along with this, there is an opinion that in the vast majority of cases, the incidence of the lymphadenoid ring of the pharynx in children is determined by a viral infection, the features of which are a protracted and recurrent course, insufficient effectiveness of conservative anti-inflammatory measures, and a tendency to hyperplasia of the palatine and pharyngeal tonsils. Usually, the doctor diagnoses a sore throat “by eye,” only on the basis of clinical experience, and prescribes antibacterial treatment without taking into account the advisability of antiviral therapy. This not only slows down the healing process, but can also contribute to a decrease in the protective properties of the pharyngeal mucosa, since under the influence of antibiotics a-hemolytic streptococcus, which produces bactericin, a natural antibiotic, disappears. It is penicillins
to a greater extent than cephalosporins, they suppress this beneficial flora of the oropharynx and allow pathogenic streptococci to take its place on the epithelium of both the tonsils and the entire pharynx. Therefore, irrational (too early and without taking into account the flora) prescription of antibiotics leads to a decrease in antibacterial immunity and contributes to relapses of sore throat.
Based on the foregoing, the treatment tactics for patients with acute and chronic tonsillitis should consist of an accurate determination of the nature of the inflammatory process (acute, exacerbation of chronic or its sluggish course), justification of the type of inflammation (catarrhal, purulent, phlegmonous), determination of the type of pathogen (streptococcus, spirochete, bacillus , virus, mushrooms). To this it is necessary to add that all sore throats can be divided into two groups
- primary tonsillitis, as a self-developing acute inflammatory process in the tonsils, and secondary tonsillitis, as a symptom of the underlying disease, for example, in blood diseases. Only the correct diagnosis, taking into account the general condition of the patient, determines the choice of treatment tactics.
Acute sore throat
Catarrhal tonsillitis is the mildest form of tonsillitis, which affects the mucous membrane of the tonsils, sometimes in combination with inflammation of the mucous membrane of the oropharynx (mainly the area of its posterior wall), which gives a mixed picture of tonsillitis and pharyngitis. The main complaint is pain when swallowing food and saliva (with pharyngitis, swallowing saliva is more painful - “empty swallow”). The general condition is satisfactory, the disease lasts 6-7 days, body temperature is within the subfebrile range. Treatment involves the widespread use of physiotherapeutic procedures, frequent rinsing with warm disinfectant solutions, a gentle diet, plenty of warm drinks, and the use of salicylates. Prescribing antibiotics for identified catarrhal tonsillitis is considered inappropriate, especially without a clear idea of the causative agent
.
Due to the fact that even without the use of antibiotics all the symptoms of the disease disappear quite quickly (on the 2-3rd day), early prescription of antibiotics in cases of catarrhal tonsillitis leads to the fact that patients stop taking them without observing the course dose. In addition, complete suppression, for example, by phenoxymethylpenicillin, amoxicillin (the most commonly used antibiotics), group A streptococci (and with them a-hemolytic streptococcus, which resists pathogenic flora) leads to the fact that the person returning to the normal environment (home, school and etc.) the recovered patient again encounters this flora, but already capable of transmission, i.e. the possibility of relapse of inflammation of the tonsils increases - natural immunity is suppressed. When prescribing antibiotics in the first days of a sore throat, it is also necessary to remember about the possible resistance of a number of strains of streptococci to the prescribed antibiotics, for example, to macrolides such as erythromycin, clarithromycin. Therefore, the most rational prescription of antibiotics in the treatment of mild forms of sore throat is after laboratory confirmation of the sensitivity of the flora to them
. These provisions are classics, but in practice, for many reasons, they are not always observed, which will ultimately lead humanity to complete disarmament in the face of transforming strains of pathogens, including those that cause sore throat.
Severe forms of angina - lacunar, follicular
- require the prescription of antibiotics, but also in compliance with the rules for combating infection and taking into account all factors: diagnosis, flora, somatic status, the need to prevent complications, the full course of taking an antibiotic.
Chronic tonsillitis
What are the treatment tactics for recurrent tonsillitis, recurring 2 times a year or more often?
In these cases, the disease is defined as “chronic tonsillitis,” however, for it, the frequency of relapses of tonsillitis may not always be the determining factor, since the concept of “chronic tonsillitis” also includes other parameters that support the diagnosis. These are, first of all, complications clearly associated with it from other organs and systems of the body.
For a practicing physician, both a general practitioner and an otorhinolaryngologist, after making a diagnosis of “chronic tonsillitis,” it is important to choose the tactics of treating the patient and decide the question: in which cases is surgery indicated, and in which - conservative therapy.
We divide chronic tonsillitis into only two forms: chronic tonsillitis I and chronic tonsillitis II
. In the first case, conservative treatment is required, in the second - surgical treatment. The determining factor is the combination of local signs of tonsillitis with complications and features of the course.
Conservative treatment
Conservative treatment involves, first of all, systematic sanitation of the lacunae of the palatine tonsils while preserving the lymphoid tissue of the tonsils.
as an immune, to a certain extent, organ. Conservative treatment is indicated for uncomplicated chronic tonsillitis in cases where surgery can be delayed due to the general condition of the patient; if the patient has not previously received any therapy or is mainly concerned about local manifestations of tonsillitis - purulent plugs in the tonsils, bad breath, etc.
Among the methods of conservative treatment for chronic tonsillitis, the most effective are the following: washing the lacunae of the tonsils and removing purulent plugs and detritus (carrying out repeated courses using the “Tonsilor” apparatus, when simultaneously washing the lacunae of the tonsils with a disinfectant solution, suctioning out the pathological contents from them and ultrasonic exposure with low-frequency ultrasound on the tonsil tissue), as well as the introduction of various medications into the tonsil using phonophoresis. Physiotherapeutic treatment – KUF, “Yakhont-F”.
Both for sore throat and for accompanying pharyngitis, gargling, inhalation, and irrigation of the mucous membrane with disinfectant solutions are indicated.
Increasing the effectiveness of treatment can be achieved by prescribing immunostimulating plant extracts. Tonsilgon N
is a combination preparation of plant origin. The chamomile, marshmallow and horsetail components included in its composition stimulate the body's defense mechanisms by increasing the phagocytic activity of macrophages and granulocytes. The drug has anti-inflammatory, immunostimulating, anti-edematous and antiviral effects, accelerates the healing process and shortens the duration of the disease; can be used in the future to prevent relapse of the disease. There were no side effects when using the drug.
Tonsilgon N is available in two forms: in the form of drops for oral administration and in the form of tablets. For adults, the drug is prescribed 25 drops or 2 tablets 5-6 times a day, for children under 5 years old - 5-10 drops, for children 5-10 years old - 15 drops, for teenagers 10-16 years old - 20 drops 5-6 times a day. day. After the disappearance of acute manifestations of the disease, the frequency of taking Tonsilgon N is reduced to 3 times a day. The duration of basic therapy is 4-6 weeks.
The prescription of systemic antibiotic therapy for uncomplicated forms of tonsillitis of non-streptococcal etiology is not always justified. In this case, local prescription of antimicrobial drugs is more rational (from the first day of the disease until the results of a microbiological study are obtained). The main requirements for local antibacterial agents are a wide spectrum of antimicrobial action, including the most typical pathogens, lack of absorption from the mucous membrane, and low allergenicity.
Fusafyungin (Bioparox) has the most optimal combination of the above requirements.
- inhaled antibiotic with anti-inflammatory properties. The wide spectrum of antibacterial action of fusafyungin, the absence of resistant strains of microorganisms, and the drug’s own anti-inflammatory properties make it especially effective in the treatment of tonsillitis of non-streptococcal etiology. The most optimal is to use 4 doses of the drug every 4 hours for 10 days.
Other drugs used in the treatment of sore throats and exacerbations of chronic tonsillitis are:
Clarithromycin
- 1 tablet 2 times a day.
Coldrex
- 2 tablets 2 times a day. Children 6-12 years old - 1 tablet 4 times a day.
Tonsillotren
(lozenges) - 1 tablet every hour.
Treatment of tonsillitis such as agranulocytic and monocytic requires the participation of a hematologist.
Surgery
Indications for surgical intervention:
1. Frequent (2-4 times a year) sore throats, accompanied by high body temperature; pathological purulent detritus is noted in the lacunae; there is one or another complication associated with an exacerbation of the process (polyarthritis, pyelonephritis, etc.).
2. Frequent sore throats (2-4 times a year or more often), accompanied by high body temperature, local signs of chronic tonsillitis are observed, without identified complications. Frequently recurring sore throats indicate a weakened immune system.
3. As a result of one of the rare cases of tonsillitis (once every 5-7 years), some complication of the heart, joints, etc. developed. Local signs of chronic tonsillitis, adenitis of the lymph nodes in the area of the angle of the lower jaw.
4. There were no cases of tonsillitis, however, against the background of emerging diseases of the heart, joints, etc., local signs of chronic tonsillitis are revealed, mainly the accumulation of purulent contents in the lacunae of the tonsils.
Fuzafyungin –
Bioparox (trade name)
(Servier)
Combined preparation of herbal origin –
Tonsilgon N (trade name)
(BIONORICA Arzneimittel GmbH)
| Applications to the article |
| Chronic tonsillitis is a process of constant interaction between lymphoid tissue and the contents of the lacunae of the palatine tonsils. |
| After making a diagnosis of chronic tonsillitis, it is important to choose a treatment strategy for the patient and decide the question: in which cases is surgery indicated, and in which - conservative therapy. |
Special Recommendations
If there is no improvement in the patient's condition when using Tonsilgon drops for 7 days, you should urgently consult a doctor. If any allergic reactions occur, treatment with the drug should be discontinued.
The appearance of sediment and slight turbidity of the liquid in the bottle during storage does not reduce the effectiveness of the drug. The solution should be shaken before use. Since Tonsilgon drops contain ethyl alcohol, you should avoid driving vehicles during treatment with the drug.
You can buy the medicine in pharmacies without a prescription. But it should only be taken if recommended by a doctor. The shelf life of the medicine is 2 years at a temperature not exceeding 25°C. It is important to store the spray in a dry place out of the reach of children.