Under normal conditions, the human heart beats smoothly and regularly. The heart rate per minute ranges from 60 to 90 beats. This rhythm is set by the sinus node, which is also called the pacemaker. It contains pacemaker cells, from which excitation is transmitted further to other parts of the heart, namely to the atrioventricular node, and to the His bundle directly in the tissue of the ventricles.
This anatomical and functional division is important from the point of view of the type of a particular disorder, because a block in the conduction of impulses or acceleration of impulses can occur in any of these areas.
Disturbances in heart rhythm and conduction are called arrhythmias and are conditions when the heart rate becomes less than normal (less than 60 per minute) or more than normal (more than 90 per minute). Arrhythmia is also a condition when the rhythm is irregular (irregular, or non-sinus), that is, it comes from any part of the conduction system, but not from the sinus node.
Classification
All rhythm and conduction disorders are classified as follows:
- Heart rhythm disturbances.
- Conduction disorders in the heart.
In the first case, as a rule, there is an acceleration of the heart rate and/or irregular contraction of the heart muscle. In the second, the presence of blockades of varying degrees with or without slowing of the rhythm is noted.
In general, the first group includes disorders of the formation and conduction of impulses:
- In the sinus node, manifested by sinus tachycardia, sinus bradycardia and sinus arrhythmia - tachyarrhythmia or bradyarrhythmia.
- According to the tissue of the atria, manifested by atrial extrasystole and paroxysmal atrial tachycardia.
- At the atrioventricular junction (AV node), manifested by atrioventricular extrasystole and paroxysmal tachycardia.
- Along the fibers of the ventricles of the heart, manifested by ventricular extrasystole and paroxysmal ventricular tachycardia.
- In the sinus node and along the tissue of the atria or ventricles, manifested by flutter and fibrillation (fibrillation) of the atria and ventricles.
The second group of conduction disorders includes blockades in the path of impulses, manifested by sinoatrial block, intraatrial block, atrioventricular block of 1, 2 and 3 degrees and bundle branch block.
Peculiarities
ECG sinus rhythm what is it? Sinus rhythm detected on the ECG indicates good activity of the heart muscle, in which there are no pathologies. This rhythm characterizes oscillations that arise from impulses in a certain node and diverge throughout the atrium and ventricle. As a result, the heart muscle contracts. For the examination to show the correct result, the patient should not worry, he needs to be in a calm state.
What does sinus rhythm ECG mean? If the doctor notes on the transcript that sinus rhythm is present, then this means that the P peaks manifest themselves on a homogeneous basis, the pulse is 60-80 beats per minute, the distances between P-P and RR are similar.
Compliance of features is checked as follows:
- The elevations P are equal in height;
- Before the QRS complex, the presence of P armholes is mandatory;
- The PQ distance remains stable;
- The P notch in the second lead is positive.
Causes of cardiac arrhythmia
The causes of arrhythmia (the occurrence of heart rhythm disturbances) are so diverse that listing absolutely everything is a very difficult task. However, in many cases, the safety of the arrhythmia for the patient’s life and further treatment tactics depend on the cause of the arrhythmia.
Many different classifications of the causes of arrhythmia have been proposed, but none of them is currently generally accepted. We consider the following classification to be the most acceptable for the patient. It is based on the presence or absence of primary heart disease in the patient. If there is heart disease, the arrhythmia is called organic, and if there is no heart disease, it is called inorganic. Inorganic arrhythmias are also commonly called functional.
Electrocardiogram indicators
- A small P wave representing atrial contraction.
- The QRS complex, which corresponds to the contraction of the ventricles.
- The ST interval with the T wave, which follows the ventricular complex and represents the moment of ventricular relaxation.
Each contraction of the atria must be followed by a contraction of the ventricles - the main law of heart rhythm. This means that after each P wave there is a QRS complex.
Most often, two types of changes occur on the ECG: disturbances in heart rhythm (arrhythmia) or disturbances in the blood supply to the myocardium (ischemia).
In the first part of our article we will talk about arrhythmias.
Organic arrhythmias
Organic arrhythmias include:
- Arrhythmias arising from coronary heart disease (myocardial infarction, angina). Arrhythmia is caused by damage to the heart muscle. It makes it difficult for electrical impulses to propagate correctly through the conduction system of the heart. Sometimes damage can even affect the cells of the main pacemaker - the sinus node. In place of the dead cells, a scar of connective tissue (cardiosclerosis) is formed, which is not able to perform the functions of a healthy myocardium. This, in turn, leads to the formation of arrhythmogenic foci and the appearance of rhythm and conduction disturbances.
- Rhythm disturbances that occur after an inflammatory process in the heart muscle - myocarditis. As a consequence, after suffering from inflammation, the myocardium is also replaced by connective tissue (cardiosclerosis).
- Arrhythmias observed in cardiomyopathies. For an unknown reason, myocardial cells are damaged, the pumping function of the heart is disrupted, and heart failure develops. In addition, various rhythm disturbances are very often associated.
- Arrhythmias that appear with various heart defects (congenital and acquired during life). It should be noted that there are congenital primary diseases of the conduction system of the heart itself.
Reasons for violations
Cardiac dysfunction in the human body occurs for the following reasons:
- Regular consumption of drinks containing strong alcohol;
- Constant smoking;
- Heart disease;
- Heart failure;
- Excess thyroid hormones;
- Mitral valve protrusion;
- Uncontrolled use of glycosides or drugs against arrhythmia.
An increase in heart rate eliminates disturbances in a person’s respiratory activity.
An electrocardiogram (ECG) is not a new and time-tested method of identifying heart pathologies. This procedure requires very little time and does not require any preparatory steps. However, in order to get the correct result, transcript and doctor’s conclusion, sometimes you need to undergo such an examination several times. Based on the data obtained and clinical examinations, the cardiologist will diagnose the patient and prescribe treatment.
Functional arrhythmias
This is also a fairly large group, including:
- Rhythm disturbances of neurogenic origin It is known that the heart is under the influence of the autonomic nervous system, which controls the activity of all internal organs. It consists of sympathetic and parasympathetic nerves. Their effect on the heart is opposite. An increase in the tone of the vagus nerve (this is a parasympathetic nerve) inhibits the work of the heart, and an increase in the tone of the sympathetic nervous system, on the contrary, stimulates its activity. Usually the influence of the vagus nerve and the sympathetic nerves are in a state of balance. However, during the day the activity of the sympathetic division of the autonomic nervous system prevails, and at night - the parasympathetic one. Excessive activation of sympathetic tone is promoted by stress, strong emotions, intense mental or physical work, smoking, drinking alcohol, strong tea and coffee, and spicy foods. The arrhythmias that arise at these moments are called sympathodependent. Often such rhythm disturbances occur in patients with neuroses. Activation of sympathetic tone also occurs in diseases of the thyroid gland, intoxication, feverish conditions, and blood diseases.
- Another group consists of vagus-dependent arrhythmias (from the Latin nervus vagus - vagus nerve). In such patients, interruptions in heart function occur at night. Diseases of the gastrointestinal tract: intestines, gallbladder, peptic ulcer of the stomach and duodenum, and diseases of the bladder can lead to an increase in the parasympathetic effect on the heart and, accordingly, to the appearance of gastrointestinal rhythm disturbances. Reflexes are formed in diseased organs, as a result of which the activity of the vagus nerve increases.
Atrial fibrillation (atrial fibrillation).
Both flutter and atrial fibrillation are often accompanied by a drop in blood pressure and cause hospitalization. If the doctor suggests going to the hospital, it is better to agree, because these arrhythmias worsen the functioning of the heart, but most importantly, they significantly increase the risk of stroke.
Before this, we talked about tachyarrhythmias, accompanied by acceleration of the heart, but bradyarrhythmias are also often encountered, in which the heart rate drops below 60. This is often quite safe, as with 1st degree AV block, when the time of impulse conduction from the atria to the ventricles is prolonged.
But even such a harmless blockade can serve as a harbinger that a pacemaker may be required in the future. If 2nd degree AV block occurs, daily ECG monitoring is indicated to identify the total number of pauses in heart contractions and their maximum duration. If there are pauses of more than 4 seconds, consultation with a cardiac surgeon specializing in the implantation of pacemakers is necessary.
Well, pacemaker implantation is absolutely indicated if third-degree AV block occurs or, as it is also called, complete transverse block. In this case, the atria contract in their own rhythm (many small P waves), but the impulses do not reach the ventricles, which contract on their own, usually at a frequency not exceeding 35-40 beats per minute.
We hope that this collection of basic knowledge on electrocardiography will help you if the doctor did not have time to answer additional questions. In the second part of the article, we will tell you how to recognize a dangerous situation - ischemia and myocardial infarction, and also understand what left ventricular hypertrophy is.
Do cardiac arrhythmias manifest themselves in the same way?
All rhythm and conduction disorders clinically manifest themselves differently in different patients. Some patients do not feel any symptoms and learn about the pathology only after a scheduled ECG. This proportion of patients is insignificant, since in most cases patients note obvious symptoms.
Thus, rhythm disturbances accompanied by rapid heartbeat (from 100 to 200 beats per minute), especially paroxysmal forms, are characterized by a sharp sudden onset and interruptions in the heart, lack of air, pain in the sternum.
Some conduction disorders, such as fascicular blocks, do not show any signs and are recognized only on an ECG. Sinoatrial and atrioventricular blockades of the first degree occur with a slight decrease in heart rate (50-55 per minute), which is why clinically they can manifest only slight weakness and increased fatigue.
Blockades of the 2nd and 3rd degrees are manifested by severe bradycardia (less than 30-40 per minute) and are characterized by short-term attacks of loss of consciousness.
In addition, any of the listed conditions may be accompanied by a general severe condition with cold sweat, intense pain in the left half of the chest, decreased blood pressure, general weakness and loss of consciousness. These symptoms are caused by impaired cardiac hemodynamics and require close attention from a doctor.
How to make a diagnosis?
ECG results - sinus rhythm
If all the parameters reflected on the cardiogram correspond to sinus rhythm, this means that the innervation impulses correctly follow from top to bottom. Otherwise, the impulses come from secondary parts of the heart.
What does a vertical position mean when there is sinus rhythm on an ECG? This is the normal location of the heart in the thoracic region on the line of the conventional location of the central axis. The location of the organ is permissible at different angles of inclination and in different planes, both vertical and horizontal, as well as in intermediate ones. This is not a pathology, but only indicates the distinctive characteristics of the structure of the patient’s body and is detected as a result of an ECG examination.
Types of arrhythmias
Most people by arrhythmia mean erratic contractions of the heart muscle (“the heart beats as it wants”). However, this is not quite true. The doctor uses this term for any disturbance of cardiac activity (decreased or increased heart rate), so the types of arrhythmias can be presented as follows:
- Sinus arrhythmia, which may be associated with cycles of respiratory activity (increased rhythm during inhalation and slower rate during exhalation) or occur independently of breathing, but indicate some kind of cardiovascular pathology (coronary artery disease in old age) or be a consequence of autonomic dysfunction, for example, in teenagers. This type of arrhythmia is harmless and does not require special treatment measures. The ECG shows a difference between cardiac cycles (> 0.05 s).
- Sinus tachycardia is diagnosed if the heart rate exceeds 90 beats/min, of course, for no apparent reason (running, exercise, excitement). Typically, with such tachycardia, the heart rate does not exceed 160 beats per minute under calm conditions, and only during intense exercise can it reach up to 200 beats. It is caused by many factors associated with pathological processes in the body, therefore the treatment of such tachycardia is aimed at the underlying disease.
- Sinus bradycardia is characterized by a regular but slow sinus rhythm (less than 60 beats/min), associated with a decrease in the automaticity of the sinus node and resulting from excessive physical exertion (in professional athletes), pathological changes (not necessarily cardiovascular, for example, peptic ulcer). ), taking certain medications (digitalis, antiarrhythmic and antihypertensive drugs). Therapy is also aimed at eliminating the cause that caused bradycardia, that is, the underlying disease.
- Extrasystoles that occur with premature excitation and contraction of one part of the heart or all of them at once, therefore, depending on where and in what place the impulse was formed that disrupted the normal sequence of heart contractions, extrasystoles are divided into atrial, ventricular and those coming from the atrioventricular node. Extrasystolic arrhythmia is dangerous if it is group, early and frequent, since it poses a threat to hemodynamics, and as a result can “develop” into ventricular tachycardia or ventricular fibrillation, which will have serious consequences. During myocardial infarction, extrasystolic arrhythmia is recorded in 100% of cases.
- Paroxysmal supraventricular (supraventricular) tachycardia, which develops suddenly and also suddenly stops, is characterized by a regular, strict rhythm, although the contraction frequency can reach 250 beats/min. Such tachycardias include: atrial tachycardia, AV nodal tachycardia and tachycardia with WPW syndrome.
- Arrhythmias associated with conduction disturbances (blockades) are usually well recorded on the ECG, are a companion and symptom of various pathologies and are treated by influencing the underlying disease. Blockades that quite often produce (sinoauricular and atrioventricular) bradycardia (40 beats per minute and below) are considered life-threatening and require the installation of a pacemaker that compensates for cardiac activity.
- Atrial fibrillation, in terms of frequency of occurrence, follows immediately after extrasystole and holds 2nd place in prevalence. It is characterized by the formation of excitation and contraction only in certain areas (fibers) of the atrium, when these processes are absent as a whole. Such chaotic and disorderly excitation of individual fibers prevents the passage of impulses into the atrioventricular node, as well as into the ventricles, to which single impulses nevertheless reach, causing excitation there that responds with random contractions.
Based on heart rate, there are 3 forms of atrial fibrillation:
- Heart rate less than 60 beats/min – bradysystolic;
- 60-100 beats/min – normosystolic;
- Heart rate exceeds 100 beats/min – tachysystolic.
On an ECG with AF, the P wave is not recorded because there is no excitation of the atria, and only atrial f waves are detected (frequency 350-700 per minute), which are characterized by irregularity, differences in shape and amplitude, which gives the electrocardiogram a unique appearance.
The cause of MA may be:
- Organic damage to the heart muscle;
- Age-related changes (coronary heart disease, often in combination with arterial hypertension);
- In young people: rheumatism, valve defects (mitral valve stenosis, aortic valve disease);
- Thyroid dysfunction;
- Congenital pathology (heart defects);
- Acute and chronic heart failure;
- Myocardial infarction;
- Acute cor pulmonale;
- Myocarditis, pericarditis;
- Cardiomyopathy.
The incidence of atrial flutter (AF) is 20-30 times lower than AF. It is also characterized by contractions of individual fibers, but a lower frequency of atrial waves (280-300 per minute). On the ECG, atrial waves have a greater amplitude than in AF.
It is interesting that on one ECG you can see the transition of flicker to flutter and vice versa.
The causes of atrial flutter are similar to the causes of fibrillation.
Symptoms of flickering and fluttering are often absent altogether, but sometimes there are some clinical manifestations caused by erratic activity of the heart or symptoms of the underlying disease. In general, such a pathology does not give a clear clinical picture.
ECG interpretation
ECG interpretation plan
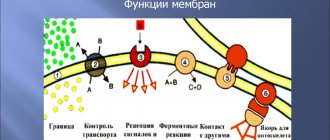
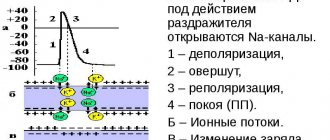
An electrocardiogram reflects only electrical processes in the myocardium: depolarization (excitation) and repolarization (restoration) of myocardial cells.
Correlation of ECG intervals with the phases of the cardiac cycle (ventricular systole and diastole).
Normally, depolarization leads to contraction of the muscle cell, and repolarization leads to relaxation.
To simplify further, instead of “depolarization-repolarization” I will sometimes use “contraction-relaxation”, although this is not entirely accurate: there is the concept of “electromechanical dissociation”, in which depolarization and repolarization of the myocardium do not lead to its visible contraction and relaxation.
Elements of a normal ECG
Before moving on to deciphering the ECG, you need to understand what elements it consists of.
Waves and intervals on the ECG. It is curious that abroad the PQ interval is usually called PR.
Any ECG consists of waves, segments and intervals.
Teeth are convex and concave areas on the electrocardiogram. The following waves are distinguished on the ECG:
- P (atrial contraction),
- Q, R, S (all 3 teeth characterize ventricular contraction),
- T (ventricular relaxation),
- U (non-permanent wave, rarely recorded).
SEGMENTS A segment on an ECG is a segment of a straight line (isoline) between two adjacent teeth. The PQ and ST segments are of greatest importance. For example, the PQ segment is formed due to a delay in the conduction of excitation in the atrioventricular (AV) node.
INTERVALS An interval consists of a tooth (a complex of teeth) and a segment. Thus, interval = tooth + segment. The most important are the PQ and QT intervals.
Waves, segments and intervals on the ECG. Pay attention to large and small cells (more about them below).
QRS complex waves
Since the ventricular myocardium is more massive than the atrial myocardium and has not only walls, but also a massive interventricular septum, the spread of excitation in it is characterized by the appearance of a complex QRS complex on the ECG.
How to correctly identify the teeth in it?
First of all, the amplitude (size) of individual waves of the QRS complex is assessed. If the amplitude exceeds 5 mm, the tooth is designated by a capital (capital) letter Q, R or S; if the amplitude is less than 5 mm, then lowercase (small): q, r or s.
The R wave (r) is any positive (upward) wave that is part of the QRS complex. If there are several teeth, subsequent teeth are indicated by strokes: R, R', R”, etc.
The negative (downward) wave of the QRS complex, located before the R wave, is designated as Q (q), and after - as S (s). If there are no positive waves at all in the QRS complex, then the ventricular complex is designated as QS.
Variants of the QRS complex.
Fine:
the Q wave reflects depolarization of the interventricular septum (the interventricular septum is excited)
R wave - depolarization of the bulk of the ventricular myocardium (the apex of the heart and adjacent areas are excited)
S wave - depolarization of the basal (i.e. near the atria) parts of the interventricular septum (the base of the heart is excited)
The RV1, V2 wave reflects the excitation of the interventricular septum,
and RV4, V5, V6 - excitation of the muscles of the left and right ventricles.
Necrosis of areas of the myocardium (for example, during myocardial infarction) causes expansion and deepening of the Q , so close attention is always paid to this wave.
ECG analysis
General scheme of ECG decoding
- Checking the correctness of ECG registration.
- Heart rate and conduction analysis:
- assessment of heart rate regularity,
- heart rate (HR) counting,
- determination of the source of excitation,
- conductivity assessment.
- Determination of the electrical axis of the heart.
- Analysis of the atrial P wave and P-Q interval.
- Analysis of the ventricular QRST complex:
- QRS complex analysis,
- analysis of the RS - T segment,
- T wave analysis,
- Q-T interval analysis.
- Electrocardiographic report.
Normal electrocardiogram.
1) Checking the correctness of ECG registration
At the beginning of each ECG tape there must be a calibration signal - the so-called control millivolt. To do this, a standard voltage of 1 millivolt is applied at the beginning of the recording, which should display a deviation of 10 mm on the tape. Without a calibration signal, the ECG recording is considered incorrect.
Normally, in at least one of the standard or enhanced limb leads, the amplitude should exceed 5 mm, and in the chest leads - 8 mm. If the amplitude is lower, this is called reduced ECG voltage, which occurs in some pathological conditions.
2) Heart rate and conduction analysis:
- assessment of heart rate regularity
Rhythm regularity is assessed by RR intervals. If the teeth are at an equal distance from each other, the rhythm is called regular, or correct. The spread of the duration of individual RR intervals is allowed no more than ± 10% of their average duration. If the rhythm is sinus, it is usually regular.
- heart rate (HR) counting
The ECG film has large squares printed on it, each of which contains 25 small squares (5 vertical x 5 horizontal).
To quickly calculate heart rate with the correct rhythm, count the number of large squares between two adjacent R-R waves.
At a belt speed of 50 mm/s: HR = 600 / (number of large squares). At a belt speed of 25 mm/s: HR = 300 / (number of large squares).
At a speed of 25 mm/s, each small cell is equal to 0.04 s,
and at a speed of 50 mm/s - 0.02 s.
This is used to determine the duration of the teeth and intervals.
If the rhythm is abnormal, the maximum and minimum heart rate is usually calculated according to the duration of the shortest and longest RR interval, respectively.
- determination of the excitation source
In other words, they are looking for where the pacemaker is located, which causes contractions of the atria and ventricles.
Sometimes this is one of the most difficult stages, because various disorders of excitability and conduction can be very confusingly combined, which can lead to incorrect diagnosis and incorrect treatment.
To correctly determine the source of excitation on an ECG, you need to have a good knowledge of the conduction system of the heart.
SINUS rhythm (this is a normal rhythm, and all other rhythms are pathological). The source of excitation is located in the sinoatrial node.
Signs on the ECG:
- in standard lead II, the P waves are always positive and are located before each QRS complex,
P waves in the same lead have the same shape at all times.
P wave in sinus rhythm.
ATRIAL rhythm. If the source of excitation is located in the lower parts of the atria, then the excitation wave propagates to the atria from bottom to top (retrograde), therefore:
- in leads II and III the P waves are negative,
- There are P waves before each QRS complex.
P wave during atrial rhythm.
Rhythms from the AV connection. If the pacemaker is located in the atrioventricular (atrioventricular node) node, then the ventricles are excited as usual (from top to bottom), and the atria are excited retrogradely (i.e. from bottom to top).
At the same time, on the ECG:
- P waves may be absent because they are superimposed on normal QRS complexes,
- P waves can be negative, located after the QRS complex.
Rhythm from the AV junction, superimposition of the P wave on the QRS complex.
Rhythm from the AV junction, the P wave is located after the QRS complex.
Heart rate with a rhythm from the AV junction is less than sinus rhythm and is approximately 40-60 beats per minute.
Ventricular, or IDIOVENTRICULAR, rhythm
In this case, the source of rhythm is the ventricular conduction system.
Excitation spreads through the ventricles in the wrong way and is therefore slower. Features of idioventricular rhythm:
- QRS complexes are widened and deformed (they look “scary”). Normally, the duration of the QRS complex is 0.06-0.10 s, therefore, with this rhythm, the QRS exceeds 0.12 s.
- There is no pattern between QRS complexes and P waves because the AV junction does not release impulses from the ventricles, and the atria can be excited from the sinus node, as normal.
- Heart rate less than 40 beats per minute.
Idioventricular rhythm. The P wave is not associated with the QRS complex.
To properly account for conductivity, the recording speed is taken into account.
To assess conductivity, measure:
- the duration of the P wave (reflects the speed of impulse transmission through the atria), normally up to 0.1 s.
duration of the P-Q interval (reflects the speed of impulse conduction from the atria to the ventricular myocardium); interval P - Q = (wave P) + (segment P - Q). Normally 0.12-0.2 s.
Measuring the internal deviation interval.
3) Determination of the electrical axis of the heart.
4) Analysis of the atrial P wave.
- Normally, in leads I, II, aVF, V2 - V6, the P wave is always positive.
- In leads III, aVL, V1, the P wave can be positive or biphasic (part of the wave is positive, part is negative).
- In lead aVR, the P wave is always negative.
- Normally, the duration of the P wave does not exceed 0.1 s, and its amplitude is 1.5 - 2.5 mm.
Pathological deviations of the P wave:
- Pointed high P waves of normal duration in leads II, III, aVF are characteristic of hypertrophy of the right atrium, for example, with “cor pulmonale”.
- Split with 2 apexes, widened P wave in leads I, aVL, V5, V6 is characteristic of left atrium hypertrophy, for example, with mitral valve defects.
Formation of the P wave (P-pulmonale) with hypertrophy of the right atrium.
Formation of the P wave (P-mitrale) with left atrial hypertrophy.
4) PQ interval analysis:
normally 0.12-0.20 s.
An increase in this interval occurs when the conduction of impulses through the atrioventricular node is impaired (atrioventricular block, AV block).
There are 3 degrees of AV block:
- I degree - the PQ interval is increased, but each P wave corresponds to its own QRS complex (there is no loss of complexes).
- II degree - QRS complexes partially fall out, i.e. Not all P waves have their own QRS complex.
- III degree - complete blockade of conduction in the AV node. The atria and ventricles contract at their own rhythm, independently of each other. Those. idioventricular rhythm occurs.
5) Analysis of the ventricular QRST complex:
- analysis of the QRS complex.
- The maximum duration of the ventricular complex is 0.07-0.09 s (up to 0.10 s).
The duration increases with any bundle branch block.
- Normally, the Q wave can be recorded in all standard and enhanced limb leads, as well as in V4-V6.
- The amplitude of the Q wave normally does not exceed 1/4 of the height of the R wave, and the duration is 0.03 s.
- In lead aVR, there is normally a deep and wide Q wave and even a QS complex.
- The R wave, like the Q wave, can be recorded in all standard and enhanced limb leads.
- From V1 to V4, the amplitude increases (while the rV1 wave may be absent), and then decreases in V5 and V6.
- The S wave can have very different amplitudes, but usually no more than 20 mm.
- The S wave decreases from V1 to V4, and may even be absent in V5-V6.
- In lead V3 (or between V2 - V4), a “transition zone” is usually recorded (equality of the R and S waves).
- RS-T segment analysis
- The ST segment (RS-T) is the segment from the end of the QRS complex to the beginning of the T wave. — — The ST segment is analyzed especially carefully in case of coronary artery disease, since it reflects the lack of oxygen (ischemia) in the myocardium.
Normally, the ST segment is located in the limb leads on the isoline (± 0.5 mm).
- In leads V1-V3, the ST segment may shift upward (no more than 2 mm), and in leads V4-V6 - downward (no more than 0.5 mm).
- The transition point of the QRS complex to the ST segment is called point j (from the word junction - connection).
- The degree of deviation of point j from the isoline is used, for example, to diagnose myocardial ischemia.
- T wave analysis.
- The T wave reflects the process of repolarization of the ventricular myocardium.
In most leads where a high R is recorded, the T wave is also positive.
- Normally, the T wave is always positive in I, II, aVF, V2-V6, with TI> TIII, and TV6> TV1.
- In aVR the T wave is always negative.
- Q-T interval analysis.
- The QT interval is called electrical ventricular systole, because at this time all parts of the ventricles of the heart are excited.
Sometimes after the T wave a small U wave is recorded, which is formed due to short-term increased excitability of the ventricular myocardium after their repolarization.
6) Electrocardiographic report. Should include:
- Source of rhythm (sinus or not).
- Regularity of rhythm (correct or not). Usually sinus rhythm is normal, although respiratory arrhythmia is possible.
- Heart rate.
- Position of the electrical axis of the heart.
- Presence of 4 syndromes:
- rhythm disturbance
- conduction disturbance
- hypertrophy and/or overload of the ventricles and atria
- myocardial damage (ischemia, dystrophy, necrosis, scars)
ECG interference
In connection with frequent questions in the comments about the type of ECG, I will tell you about the interference that may be on the electrocardiogram:
Three types of ECG interference (explained below).
Interference on an ECG in the lexicon of health workers is called interference: a) induction currents: network interference in the form of regular oscillations with a frequency of 50 Hz, corresponding to the frequency of alternating electric current in the outlet. b) “swimming” (drift) of the isoline due to poor contact of the electrode with the skin; c) interference caused by muscle tremors (irregular frequent vibrations are visible).
ECG analysis algorithm: determination method and basic standards