Contraindications
Conditions in which this manipulation cannot be performed include:
- varicose veins of the esophagus
- obstruction of the esophagus (narrowing, diverticula)
- exacerbation of gastritis, gastric ulcer and duodenal ulcer
- stomach/intestinal bleeding and conditions after it
- oncological diseases of the gastrointestinal tract
- cholelithiasis (presence of movable stones in the gallbladder), surgery to remove the gallbladder
- chronic cholecystitis and/or pancreatitis in the acute stage
- aortic aneurysm
- cardiovascular failure
- decompensated diabetes mellitus
- asthma attack
- pathologies of the oropharynx, accompanied by impaired swallowing
- general serious condition of the patient
- pregnancy and breastfeeding period.
General characteristics of the anatomy and functioning of the liver and gallbladder
The liver and gallbladder form part of the digestive tract. In addition to participating in the digestion process, the liver is an organ of the immune system; in addition, it performs a protective function, partly the function of hematopoiesis, and most importantly, detoxification.
Anatomically, the liver is located in the abdominal cavity, it is formed by two parts - the left and right lobes. Most of the organ is located in the upper right part of the abdominal cavity. The left lobe partially passes into the left half of the abdominal cavity.
The liver is located under the diaphragm, its upper border is at chest level, it is convex and follows the shape of the diaphragm. The lower edge is 1-2 centimeters below the arch of the ribs, concave and in contact with other internal organs.
The right lobe of the liver is approximately 6 times larger than the left. The mass of the organ ranges from one and a half to two kilograms.
In the middle part of the internal surface of the organ, the hepatic gate is located - at this place the hepatic artery enters the liver, from there exit the portal vein and the hepatic duct, which removes bile from the liver.
The gallbladder is “hidden” under the gate of the organ - a small hollow organ 12 to 18 cm long, which is adjacent to the outer edge of the liver and lies on the duodenum. The structure of the bladder is represented by the bottom, body and neck, which passes into the cystic duct.
The liver is responsible for the secretion of bile, which breaks down fats, enhances intestinal motility and the action of pancreatic and intestinal enzymes. Bile also helps neutralize the acidic environment of the food bolus that leaves the stomach, promotes the absorption of cholesterol, amino acids, calcium salts and fat-soluble vitamins.
The liver is involved in all metabolic processes in the body - protein, fat, carbohydrates.
The organ also synthesizes hormones and stimulates the production of hormones by the adrenal glands, thyroid and pancreas.
In addition, the liver is a huge protective filter that neutralizes the effects of toxins, poisons, medications, and allergens.
Bile produced by the liver enters the gallbladder, where it accumulates until the food entering the body is digested.
Necessary preliminary studies
The duodenal intubation procedure, like any invasive, i.e. penetrating into the body, study is a serious procedure that requires the so-called tolerance to minimize possible complications. The task of the specialists of the EXPERT Clinic is to responsibly approach the issue of examination and the safety of its implementation.
Therefore, duodenal intubation is performed in patients only if:
- referrals from a specialist who clearly assesses the validity of the procedure and the competence of its implementation for a specific patient
- preliminary ultrasound of the gallbladder, which will assess the condition of the gallbladder and its contents. If there are stones or inflammation of the wall, the procedure can be extremely dangerous. Shelf life: 1 month.
- FGDS, which is carried out to assess the condition of the mucous membrane of the stomach and duodenum, because the presence of inflammation, ulcers, or anatomical features may be a contraindication or impossibility of the procedure. Shelf life: 1 month.
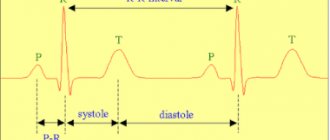
- An ECG, which will allow you to assess the presence or absence of risks of cardiovascular complications during the probing process, because The procedure lasts several hours with possible fluctuations in blood pressure, in particular. Shelf life: 1 month.
What types of procedures can be performed
Duodenal sounding may differ depending on how it is carried out:
- blind probing, when the patient does not have to swallow the probe - the procedure uses the process of stimulating bile formation;
- fractional or multi-moment: in this case, content is collected at a certain interval, for example, every five minutes;
- chromatic sounding implies that before diagnosis, a dye is injected into the patient;
- a minute-long procedure makes it possible to assess the condition and functioning of the sphincters.
Preparation for the procedure
Duodenal intubation is performed in the morning strictly on an empty stomach. Two hours before the procedure, it is permissible to take a few sips of plain water. Immediately before the procedure, you should not drink, smoke, or take medications. The oral cavity must be rinsed, the nasal passages cleaned, and dentures removed (if any).
Dinner on the eve of the procedure should be no later than 18.00. Products that cause gas formation are prohibited. This:
- fermented milk products
- black bread
- fresh vegetables and fruits
- legumes
- potato
- carbonated drinks, etc.
Taking medications is possible only with the permission of a doctor.
5 days before probing, you must stop taking medications:
- choleretic (allochol, cholenzym, liv-52, holosas, etc.)
- digestive enzymes (pancreatin, festal, panzinorm, etc.).
Methodology
Duodenal intubation is carried out with a disposable sterile probe, much smaller in diameter and more flexible than the probe for FGDS. Initial position of the patient: sitting with the chin pressed to the chest and the mouth wide open.
- The end of the probe (olive) is placed on the root of the tongue and, at the moment of swallowing, is advanced into the esophagus and further into the stomach (it is recommended to breathe deeply).
- Then the patient is placed on the couch on his right side, placing a small cushion.
- The patient is asked to make a swallowing movement, while simultaneously advancing the probe into the duodenum. The accuracy of the actions performed is confirmed by the flow of golden-yellow liquid into the probe. So, within about half an hour, the first portion of duodenal contents of 15-40 ml is collected - portion “A”.
- Then a substance that enhances secretion (xylitol, sorbitol, magnesium sulfate) is introduced into the lumen of the duodenum, and the lumen of the probe is clamped with a clamp. After 5-10 minutes, the instrument is removed, and dark green bile begins to flow into the probe. Portion “B” with a volume of about 60 ml is collected within 20-30 minutes.
- When there is a noticeable change in the color of the liquid to bright yellow, they begin collecting portions “C” with a volume of 10-20 ml.
Upon completion of the collection of all types of portions (A, B and C), the patient is placed in a sitting position and the probe is carefully removed. If a bitter taste is felt in the mouth, the patient is offered to rinse with antiseptics or glucose solution.
How is research done using a probe?
The probing procedure can take from an hour to an hour and a half.
Before starting the diagnostic procedure itself, the doctor asks the patient to take a standing position and measures the distance from the oral cavity to the navel of the subject.
A specialist will need this information to correctly calculate the length of the probe to use. After this, the patient is seated on the couch, given a special tray, and the examination begins directly.
The main difficulty of probing is that the patient will have to “swallow” the probe on his own. If the patient does this incorrectly, he will provoke a strong gag reflex. How can this be avoided? In this regard, experts give several clear recommendations:
- The internal organs of the subject should not be “squeezed”. That is why before the procedure he should wear the loosest and most comfortable clothes possible.
- During the examination itself, it is recommended to loosen the belt on your trousers and unbutton the top buttons on your blouse or shirt.
- During the procedure itself, the patient should try to breathe through the nose and as deeply as possible, tightly fixing the probe with his lips.
- While “absorbing” the probe, the patient should try to simultaneously swallow the saliva that has accumulated in the mouth. However, this must be done very slowly, otherwise you may choke and provoke a gag reflex. Moreover, if the probe is quickly swallowed, there is a risk that the hose will simply curl up in the subject’s stomach.
The patient should follow all the above recommendations until the research device reaches his stomach. You can judge that this happened by the marks on the probe itself. Or - by blowing air through the hose (usually this is done using a syringe). If during such manipulations in the chest area the patient hears gurgling and bubbling, then everything is going as planned.
Recommendations after the procedure
Eating is allowed 30-40 minutes after probing (light breakfast). Throughout the day, you must follow a diet with the exception of heavy foods - fatty, fried, spicy foods.
After the procedure, the patient’s blood pressure and pulse may destabilize, so it is advisable for him to remain in the ward or in the clinic lobby for an hour under the supervision of medical workers. It is also possible for the body to develop a response to the administration of magnesium sulfate in the form of diarrhea (loose stools).
Results of duodenal sounding
Duodenal sounding is a very informative diagnostic method for specialists.
- Studying the dynamics of bile secretion allows us to assess the functional state of the gastrointestinal tract. For example, acceleration or deceleration of the intake of portion “B” is usually observed with functional disorders of the gallbladder (dyskinesia), the release of bile more than 60 ml indicates congestion, and its complete absence indicates a possible obstacle to the outflow of bile (stone, tumor, inflammatory infiltrate , scar deformity, etc.).
- Laboratory analysis makes it possible to determine the presence of cholelithiasis, helminthic infestations, bacterial infections, as well as assess the exocrine function of the pancreas, the consistency of the sphincters and muscles of the gallbladder.
- In addition, duodenal intubation allows the administration of medications bypassing the stomach, which can be very important for some gastrointestinal pathologies. Also, the method of probing is used to introduce nutritional mixtures in the process of caring for “severe” patients.
- The results of this examination are decisive in the process of making a diagnosis and developing a conservative treatment regimen and very often allow patients to avoid serious surgery.
Why are such examinations prescribed?
Duodenal intubation - examination of the biliary tract.
Duodenal intubation is considered one of the advanced research methods, indispensable in the diagnosis of diseases of the bile ducts.
In other words, if inflammatory processes begin in the pancreas, liver or organs communicating with them, the composition of the secretions produced by the digestive system will change. And duodenal sounding will help detect and record such changes.
On what basis are such examinations prescribed? An indication for referring a patient for duodenal intubation may be the manifestation of such alarming symptoms as:
- bitterness in the mouth;
- copious sputum production;
- pain in the hypochondrium (usually on the right);
- nausea and vomiting syndrome;
- increased concentration of urine.